Last Updated on December 1, 2025 by Bilal Hasdemir
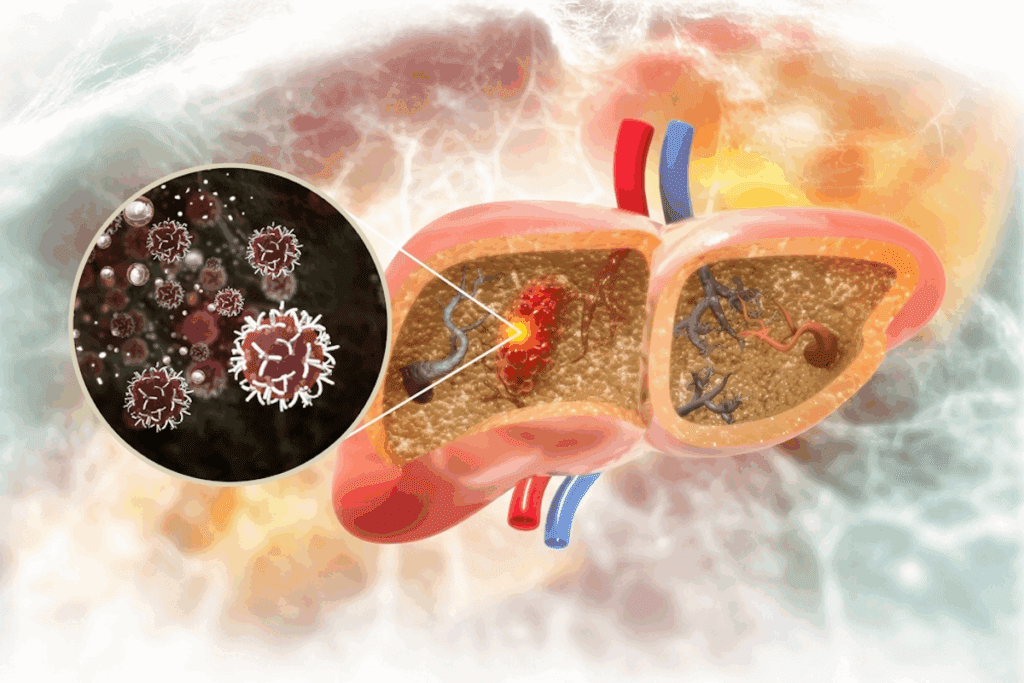
Did you know that hepatoblastoma, a rare liver cancer, is the most common liver malignancy in children? We are here to explore the genetic aspects of this condition.
Hepatoblastoma mainly hits young kids. Knowing its genetic roots helps us understand its causes and treatments. Scientists are working hard to find the genetic links to hepatoblastoma.
Looking into hepatoblastoma‘s genetics shows that some genes are key to its growth. We’ll look at what we know about these genes and what they mean.
Key Takeaways
- Understanding the genetic basis of hepatoblastoma can provide insights into its causes.
- Genetic mutations are a significant factor in the development of hepatoblastoma.
- Research is ongoing to uncover the underlying genetic factors.
- The genetic aspects of hepatoblastoma are critical for developing treatments.
- Hepatoblastoma mainly affects young children.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
Hepatoblastoma is a rare liver cancer that mainly affects children. It’s a complex condition that needs a deep understanding. Knowing its definition, how common it is, and its impact on kids is key.
Definition and Prevalence of Hepatoblastoma
Hepatoblastoma is a cancer of the liver found mostly in kids. It’s the top liver cancer in children, making up about 1% of all cancers in kids. Studies show it affects about 1.2 kids per million under 15.
As a study found, “Hepatoblastoma is a rare tumor that usually shows up in the first two years of life. It most often happens between 6 to 12 months old.”
“The number of cases of hepatoblastoma has gone up in recent years, but it’s not very common.”
Age Groups Most Commonly Affected
Hepatoblastoma mostly hits young kids, with most cases found in the first two years. The highest number of cases is between 6 to 12 months old. It’s less common in kids over 3.
Age Distribution:
| Age Group | Percentage of Cases |
| 0-1 year | 40% |
| 1-2 years | 30% |
| 2-3 years | 15% |
| >3 years | 15% |
General Prognosis and Survival Rates
The outlook for hepatoblastoma has gotten better thanks to better treatments. Now, kids have a 70% to 80% chance of survival in places with good healthcare.
How well a kid does depends on when the cancer is found and how it’s treated. Finding it early and treating it right is key to better chances.
The Hepatoblastoma Genetic Connection
Hepatoblastoma is a rare liver cancer mainly found in children. It’s linked to genetic mutations. Knowing the genetic causes helps in finding better treatments and understanding risks.
Overview of Cancer Genetics
Cancer genetics looks at how genes change in cancer. In hepatoblastoma, research has found key mutations. These insights help in treating the disease.
Genetic changes can happen in two ways: in cells that aren’t reproductive or in reproductive cells. Changes in non-reproductive cells are not passed on, but changes in reproductive cells can be inherited.
Somatic vs. Germline Mutations
In hepatoblastoma, CTNNB1 gene mutations are common. These mutations can make tumors grow. Germline mutations, like those in FAP, raise the risk of getting hepatoblastoma.
| Type of Mutation | Description | Impact on Hepatoblastoma |
| Somatic Mutations | Acquired during a person’s lifetime, not inherited | Contribute to tumor development and growth |
| Germline Mutations | Inherited, passed to future generations | Increase the risk of developing hepatoblastoma |
Evidence for Genetic Basis of Hepatoblastoma
Research links CTNNB1 gene mutations to hepatoblastoma. Other genetic changes also play a role. For example, APC gene mutations, linked to FAP, are found in some patients.
Genetic testing and counseling are key for families with hepatoblastoma. This helps in providing tailored care and surveillance.
Common Genetic Mutations in Hepatoblastoma
Hepatoblastoma has many genetic mutations that start and grow the tumor. Knowing these mutations helps in making better treatments and improving patient care.
Beta-Catenin (CTNNB1) Mutations
The CTNNB1 gene, which makes beta-catenin, is often changed in hepatoblastoma. These changes make beta-catenin build up in the nucleus. This buildup turns on genes that help cells grow and live longer.
Research shows that CTNNB1 mutations are common in hepatoblastoma. This makes them key in how the disease starts.
APC Gene Mutations
The APC gene is also a big deal in hepatoblastoma. APC helps control beta-catenin levels. When APC is mutated, beta-catenin builds up and moves into the nucleus, just like with CTNNB1 mutations.
Familial adenomatous polyposis (FAP) is linked to APC mutations. It raises the risk of getting hepatoblastoma, mostly in kids.
AXIN1 and AXIN2 Mutations
AXIN1 and AXIN2 help keep the Wnt/β-catenin pathway in check. But when they’re mutated, this pathway gets activated. This helps grow hepatoblastoma.
Other Significant Genetic Alterations
There are more genetic changes in hepatoblastoma. These include changes in genes that control cell growth, fix DNA, and other pathways.
| Gene | Function | Effect of Mutation |
| CTNNB1 | Encodes beta-catenin, a key component of the Wnt signaling pathway | Activation of Wnt/β-catenin pathway, leading to increased cell proliferation |
| APC | Tumor suppressor gene regulating beta-catenin levels | Stabilization and nuclear translocation of beta-catenin, promoting tumorigenesis |
| AXIN1/AXIN2 | Negative regulators of the Wnt/β-catenin pathway | Activation of Wnt/β-catenin pathway, contributing to tumor development |
Knowing about these genetic changes is key for making new treatments. It also helps in better managing hepatoblastoma.
Hereditary Syndromes Associated with Hepatoblastoma Risk
Hepatoblastoma, a rare liver cancer in kids, is linked to several genetic syndromes. These conditions raise the risk of this cancer. Knowing about these syndromes helps in early detection and treatment of hepatoblastoma.
Familial Adenomatous Polyposis (FAP)
Familial adenomatous polyposis (FAP) causes many polyps in the colon and rectum. It increases the risk of cancers, including hepatoblastoma. FAP is caused by mutations in the APC gene, which controls cell growth and division.
People with FAP face a higher risk of hepatoblastoma, often in early childhood. Families with FAP history should get genetic tests and surveillance to manage the risk.
Beckwith-Wiedemann Syndrome
Beckwith-Wiedemann Syndrome (BWS) is a growth disorder that raises the risk of tumors, like hepatoblastoma. BWS is linked to genetic and epigenetic changes on chromosome 11p15.5, affecting growth genes.
Children with BWS are at a higher risk of hepatoblastoma and other cancers. Regular checks and screenings are key for early treatment.
Simpson-Golabi-Behmel Syndrome
Simpson-Golabi-Behmel Syndrome (SGBS) is a rare disorder with overgrowth, unique facial features, and a higher cancer risk, including hepatoblastoma. SGBS is caused by mutations in the GPC3 gene, which regulates cell growth.
Boys with SGBS are at higher risk due to its X-linked nature. Genetic testing can help identify families at risk.
Trisomy 18 and Other Chromosomal Abnormalities
Trisomy 18, or Edwards syndrome, is a chromosomal condition that raises the risk of tumors and congenital anomalies, including hepatoblastoma. Other chromosomal issues may also increase the risk of hepatoblastoma.
| Syndrome | Genetic Basis | Risk of Hepatoblastoma |
| Familial Adenomatous Polyposis (FAP) | APC gene mutations | Increased risk in early childhood |
| Beckwith-Wiedemann Syndrome (BWS) | Genetic/epigenetic alterations on chromosome 11p15.5 | Increased risk of various tumors |
| Simpson-Golabi-Behmel Syndrome (SGBS) | GPC3 gene mutations | Increased risk, particular in males |
| Trisomy 18 | Chromosomal abnormality | Increased risk of congenital anomalies and tumors |
Understanding these genetic syndromes is key to early detection and management of hepatoblastoma. Genetic testing and surveillance can identify at-risk individuals and improve outcomes.
Hepatoblastoma Genetic Risk Factors
Hepatoblastoma is a rare liver cancer in kids. It’s linked to several genetic risk factors. Knowing these factors helps us spot kids at higher risk and maybe prevent the disease.
Family History and Inheritance Patterns
Family history is key in hepatoblastoma risk. Kids with a family history of certain genetic syndromes face higher risks. We’ll look into how these conditions raise the risk of hepatoblastoma.
Genetic Syndromes and Hepatoblastoma Risk
- Familial Adenomatous Polyposis (FAP) greatly increases the risk of hepatoblastoma.
- Beckwith-Wiedemann Syndrome also raises the risk.
Environmental Factors That May Interact with Genetic Predisposition
Genetics are important, but environmental factors can also play a part. We’ll see how exposure to certain toxins or factors might impact kids with a genetic predisposition.
Potential Environmental Influences
- Exposure to certain chemicals might be a risk factor.
- Maternal health and prenatal factors could also matter.
Assessing Individual Risk Based on Genetics
Understanding a child’s genetic profile and family history is key. We’ll talk about how genetic testing and counseling help families grasp their risk. This way, they can make informed choices.
Differences in Risk Across Populations
Hepatoblastoma risk varies among different groups. Some ethnic and demographic groups have higher rates. We’ll look into these differences and their possible causes.
By grasping the genetic risk factors for hepatoblastoma, we can better spot at-risk kids. This could lead to better outcomes through early detection and action.
Genetic Testing for Hepatoblastoma
Hepatoblastoma genetic testing is key to finding mutations linked to this rare liver cancer. It gives vital info on genetic changes that lead to hepatoblastoma.
Available Testing Methods
There are many genetic testing methods for diagnosing and managing hepatoblastoma. These include:
- Next-Generation Sequencing (NGS): This advanced tech quickly sequences large DNA amounts. It helps spot mutations in genes linked to hepatoblastoma.
- Sanger Sequencing: A traditional method used to confirm mutations found by NGS or other tests.
- Array Comparative Genomic Hybridization (aCGH): This technique detects copy number variations in the genome. These can be linked to hepatoblastoma.
These methods can be used alone or together. They give a detailed genetic profile of the tumor.
When Genetic Testing Is Recommended
Genetic testing for hepatoblastoma is suggested in certain cases:
- When there’s a family history of hepatoblastoma or related cancers.
- In cases where the patient is diagnosed with hepatoblastoma at a very young age.
- If the patient has other congenital anomalies or syndromes linked to a higher risk of hepatoblastoma.
Genetic testing can spot those at higher risk. It guides clinical management decisions.
Interpreting Test Results
Understanding genetic testing results for hepatoblastoma needs expertise in genetics and oncology. A positive test may show a mutation linked to a higher risk of hepatoblastoma. But remember:
- A positive result doesn’t mean you’ll definitely get hepatoblastoma.
- A negative result doesn’t rule out the risk completely.
Genetic counseling is key in the testing process. It helps families grasp the meaning of test results. This way, they can make informed decisions about their care.
Hepatoblastoma Genetic Predisposition: What It Means for Families
Families with a history of hepatoblastoma can learn a lot about its genetic factors. Knowing about genetic predisposition can change how families see their risk, plan for the future, and feel about their health.
Recurrence Risk in Siblings
For families with a history of hepatoblastoma, the biggest worry is the risk of it happening again in siblings. Studies show that siblings might face a higher risk, mainly if a genetic mutation is found. Genetic counseling can help families grasp this risk and make smart choices.
Implications for Future Generations
The genetic effects of hepatoblastoma don’t just stop with the immediate family. They can also affect future generations if a genetic mutation is found. Understanding these effects can help families plan and prepare for the future.
Family Planning Considerations
Families with a history of hepatoblastoma might need to think about genetics when planning for kids. Genetic counseling can offer insights into risks, helping families make informed choices about family planning.
Psychological Impact of Genetic Risk
Learning about the genetic risk of hepatoblastoma can deeply affect families. Feelings of anxiety, fear, and uncertainty are common. Support from genetic counselors, psychologists, and support groups can be very helpful in dealing with these feelings.
| Genetic Factor | Implication | Family Planning Consideration |
| Known Genetic Mutation | Increased risk for siblings and future generations | Genetic counseling recommended |
| Family History | Potential increased risk | Monitoring and screening recommended |
| Genetic Predisposition | Variable risk depending on mutation | Personalized risk assessment |
Genetic Counseling for Families Affected by Hepatoblastoma
Getting a diagnosis of hepatoblastoma can be scary. But, genetic counseling can guide families through the genetic side of it.
The Role of Genetic Counselors
Genetic counselors are experts in genetics and counseling. They have special training.
They help families understand hepatoblastoma’s genetic roots. They also talk about the risk of it happening again and what it means for other family members.
Genetic counselors offer emotional support. They help families decide on genetic testing and planning for the future.
What to Expect During Genetic Counseling
In a genetic counseling session, families talk about their health and family history.
The counselor looks at the risk factors for hepatoblastoma. They also talk about the possible genetic causes.
Families learn about genetic testing and what the results mean.
Finding Specialized Genetic Counselors
To find a genetic counselor for hepatoblastoma or cancer genetics, start with your doctor.
Look for certified genetic counselors through organizations like the National Society of Genetic Counselors (NSGC). They have directories online.
It’s key to find a counselor with experience in pediatric cancer genetics. This ensures you get the right and accurate information.
Resources and Support Groups for Families
Families with hepatoblastoma can find help and support.
Groups like the Children’s Liver Disease Foundation and the Hepatoblastoma Research Foundation offer support. They also connect families with others who have gone through similar things.
Genetic counselors can also tell you about local and online support groups.
Hepatoblastoma Genetic Markers and Their Clinical Significance
Understanding the genetic markers of hepatoblastoma is key to better treatments. This rare liver cancer mainly hits kids. It’s linked to genetic changes that affect how well it responds to treatment.
Prognostic Markers
Prognostic markers tell us about a disease’s likely outcome. In hepatoblastoma, some genetic changes, like in the CTNNB1 gene, are important. These changes can mean a better or worse outlook.
| Genetic Mutation | Prognostic Significance |
| CTNNB1 mutation | Favorable prognosis in certain contexts |
| APC gene mutation | Associated with Familial Adenomatous Polyposis (FAP) |
| AXIN1/AXIN2 mutations | Potential impact on Wnt/β-catenin pathway |
Predictive Markers for Treatment Response
Predictive markers show which treatments will work best. In hepatoblastoma, some genetic changes help predict how well treatments will work. For example, tumors with certain Wnt/β-catenin pathway mutations might react differently to treatments.
Key Predictive Markers:
- Mutations in CTNNB1 and other genes in the Wnt/β-catenin pathway
- Genetic alterations affecting cell cycle regulation
Emerging Biomarkers in Research
New research is finding more genetic biomarkers for hepatoblastoma. It looks like some microRNAs and genetic elements play a big role in the disease. They could be targets for new treatments.
Using Genetic Markers to Guide Treatment Decisions
Genetic markers help tailor treatments for hepatoblastoma. By knowing a tumor’s genetics, doctors can create a treatment plan that fits the patient. This could lead to better results.
As we learn more about hepatoblastoma’s genetics, genetic markers will play a bigger role in treatment. This could bring new hope to patients and their families.
Advances in Genetic Research on Hepatoblastoma
Genetic studies have made big strides in understanding hepatoblastoma, a rare liver cancer in kids. They’ve found genetic mutations and how they affect diagnosis and treatment.
Recent Discoveries in Hepatoblastoma Genetics
Studies have found several genetic mutations linked to hepatoblastoma. One key mutation is in the CTNNB1 gene, which codes for beta-catenin. These findings help us understand the disease better and find new treatments.
Genetic factors in hepatoblastoma have become clearer. For example, mutations in the APC gene are linked to Familial Adenomatous Polyposis (FAP). This condition raises the risk of getting hepatoblastoma.
Ongoing Clinical Trials
Many clinical trials are testing new treatments for hepatoblastoma. They focus on targeted therapies that target specific genetic mutations.
- Trials examining the efficacy of drugs targeting the Wnt/β-catenin pathway
- Studies on the use of immunotherapy in treating hepatoblastoma
- Research into the role of genetic markers in predicting treatment response
International Collaborative Research Efforts
International collaboration is key in advancing hepatoblastoma research. Global networks share data, resources, and expertise. This speeds up the discovery of new treatments.
| Research Initiative | Focus Area | Participating Countries |
| International Hepatoblastoma Consortium | Genetic profiling and targeted therapies | USA, UK, Japan |
| Global Pediatric Liver Cancer Study Group | Immunotherapy and genetic markers | Germany, France, Australia |
Future Directions in Research
Future research will look into new genetic markers and personalized medicine. It will also explore how genes and environment interact in hepatoblastoma.
We expect ongoing and future research to reveal more about hepatoblastoma’s genetics. This will lead to better and more targeted treatments for this rare cancer.
Personalized Medicine Approaches Based on Genetic Profiles
Genetic profiling is leading the way in personalized medicine for hepatoblastoma. It brings new hope to patients. By using genetic info in treatment plans, we’re changing how we fight this rare liver cancer in kids.
Understanding the genetic roots of hepatoblastoma helps us create targeted treatments. These treatments are more effective and tailored to each patient.
Targeted Therapies for Specific Genetic Mutations
Targeted therapies based on genetic profiles are being tested for treating hepatoblastoma. For example, mutations in the CTNNB1 gene are common. Treatments that block the Wnt/beta-catenin pathway are showing promise in trials.
Therapies targeting other genetic mutations, like in the APC and AXIN1 genes, are also being developed. These genes are part of the same pathway as CTNNB1.
Immunotherapy Based on Genetic Markers
Immunotherapy is another promising area for personalized treatment. By looking at a patient’s genetic markers, we can find targets for immunotherapy. For example, some tumors might respond well to checkpoint inhibitors or CAR-T cell therapy.
There’s growing interest in using immunotherapy for hepatoblastoma. Ongoing research aims to see how well and safely it works.
Precision Medicine in Pediatric Liver Cancer
Precision medicine is key in treating pediatric liver cancer. It tailors treatment to the tumor’s unique genetic traits. This approach boosts treatment success and reduces side effects from traditional treatments.
We’re dedicated to improving precision medicine in hepatoblastoma. This includes ongoing research and developing new targeted therapies.
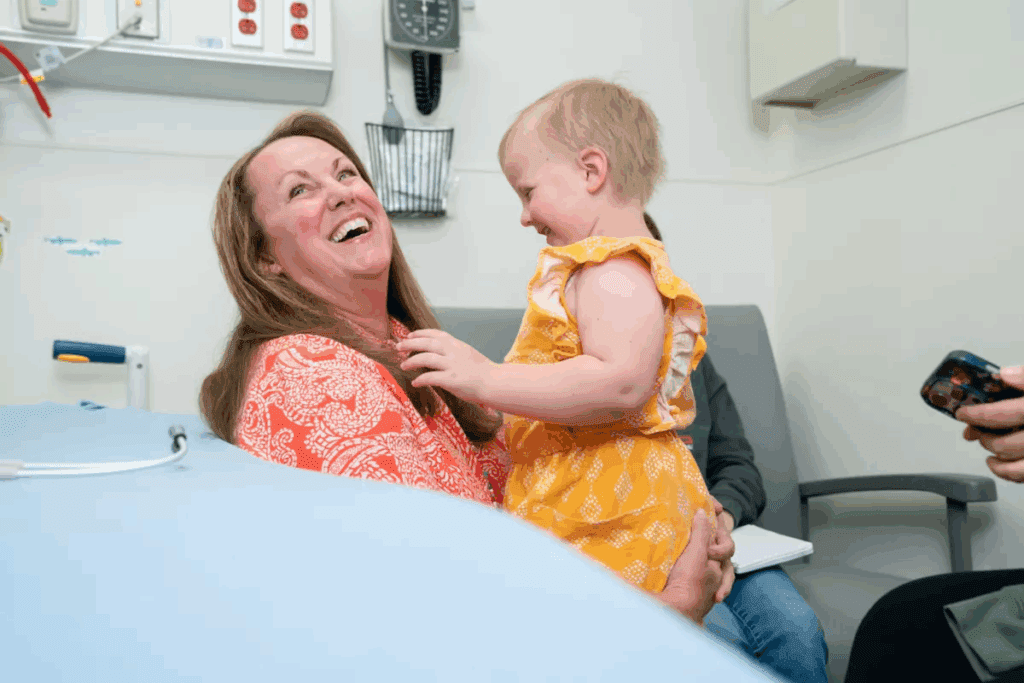
Case Studies of Successful Genetically-Guided Treatments
Several case studies show the power of genetically-guided treatments in hepatoblastoma. For example, a patient with a specific CTNNB1 mutation had a great response to a targeted therapy. These stories highlight the value of genetic profiling in treatment decisions.
In conclusion, personalized medicine based on genetic profiles is changing how we treat hepatoblastoma. With targeted therapies, immunotherapy, and precision medicine, we’re moving towards better treatments. As research keeps advancing, we expect even better results for patients.
Ethical Considerations in Hepatoblastoma Genetic Testing
Genetic testing in hepatoblastoma raises many ethical questions. As we learn more about this rare liver cancer, we face complex dilemmas. We must address these issues carefully.
Privacy and Genetic Information
Privacy of genetic info is a big concern. Tests can reveal personal details, not just for the patient but also for their family. Keeping this info private is very important. We need to protect it while sharing it with doctors for the best care.
With new testing methods, keeping genetic data safe is a growing worry. Strong data protection is needed to stop unauthorized access.
Testing in Children and Informed Consent
Testing children raises questions about consent. Hepatoblastoma mainly affects young kids. Parents or guardians usually decide, but they must be well-informed.
It’s important to explain the benefits and risks of testing clearly. This includes talking about the emotional impact and future family planning.
Insurance and Employment Discrimination Concerns
Genetic tests can lead to worries about insurance and jobs. There’s a chance genetic info could lead to unfair treatment. We must keep these laws strong and enforced.
Balancing Knowledge and Psychological Burden
Genetic testing offers benefits but can also be stressful. It’s key to offer support to families going through this.
We must handle these ethical issues with care. This way, we can use genetic testing to help while respecting our patients and their families.
Conclusion: The Future of Genetic Understanding in Hepatoblastoma
As we learn more about hepatoblastoma, it’s clear that genes are key in this rare liver cancer. We’ve made big strides in understanding the genes behind it. This has helped us see how the disease works.
Knowing about certain gene changes, like in the CTNNB1 gene, helps doctors diagnose and treat better. Next, research will aim to use this knowledge to create new, targeted treatments. This could make treatments more effective and safer for kids.
Looking ahead, we must keep studying how genes and the environment interact. Working together and improving genetic testing will be key. By using genetic research, we can make treatments more tailored to each child. This could lead to better results for kids with this serious disease.
FAQ
Is hepatoblastoma a genetic condition?
Hepatoblastoma can be linked to genetic mutations and hereditary syndromes. But it’s not just about genetics. Both genetic and environmental factors play a role in its development.
What genetic mutations are commonly found in hepatoblastoma?
In hepatoblastoma, you often see mutations in CTNNB1, APC, AXIN1, and AXIN2. These genes are part of the Wnt/β-catenin pathway. They’re key in how the disease grows and spreads.
Are there hereditary syndromes associated with an increased risk of hepatoblastoma?
Yes, certain syndromes like Familial Adenomatous Polyposis (FAP), Beckwith-Wiedemann Syndrome, and Simpson-Golabi-Behmel Syndrome raise the risk of hepatoblastoma.
What is the role of genetic testing in hepatoblastoma?
Genetic testing can spot mutations and syndromes linked to hepatoblastoma. It’s vital for diagnosis, treatment, and planning for families.
How is genetic risk assessed for hepatoblastoma?
To assess genetic risk, look at family history, genetic mutations, and environmental factors. These can all affect the risk.
What does a genetic predisposition to hepatoblastoma mean for families?
A genetic predisposition means siblings might face a higher risk. It also affects future generations, family planning, and the mental health of family members.
What is genetic counseling, and how can it help families affected by hepatoblastoma?
Genetic counseling helps families understand their genetic risk. It guides them in making informed decisions about family planning and treatment.
Are there any ethical considerations surrounding genetic testing for hepatoblastoma?
Yes, there are ethical concerns. These include privacy, informed consent, and the psychological impact on families. There’s also the risk of discrimination in insurance and employment.
How are genetic markers used in the treatment of hepatoblastoma?
Genetic markers help tailor treatments and predict how well they’ll work. They’re essential in personalized medicine for hepatoblastoma.
What is the future of genetic research on hepatoblastoma?
Research is ongoing to find new genetic discoveries and improve treatments. Advances in technology and collaboration will keep driving progress in this field.
Reference
- Czauderna, P., Lopez-Terrada, D., Hiyama, E., Häberle, B., Malogolowkin, M., & Meyers, R. (2019). Hepatoblastoma state of the art: Pathology, genetics, risk stratification, and chemotherapy. Current Opinion in Pediatrics, 31(3), 380-387. https://journals.lww.com/co-pediatrics/abstract/2019/04000/deliveries_at_extreme_prematurity__outcomes,.4.aspx