Starting an IVF journey is both emotionally tough and exciting. It’s important to understand how embryos grow from fertilization to the blastocyst stage. About 80% of mature eggs will fertilize, but not all will make it to the blastocyst stage.
The path from fertilization to day 5 is complex. 30-50% of fertilized eggs successfully reach the blastocyst stage. This shows a natural selection process that picks the healthiest embryos for transfer.
Key Takeaways
- Approximately 80% of mature eggs fertilize during IVF.
- 30-50% of fertilized eggs progress to the blastocyst stage by day 5 or 6.
- The attrition rate during IVF reflects a natural biological selection process.
- Understanding embryo development stages is key for managing expectations.
- IVF success rates are influenced by many factors, including embryo quality.
The IVF Journey: From Egg Retrieval to Blastocyst
Learning about the IVF process is key for those going through fertility treatment. It covers egg retrieval, fertilization, and blastocyst development. Each stage is important for the success of the IVF cycle.
The Egg Retrieval Process
Egg retrieval is the first big step in IVF. It’s when eggs are taken from the ovaries through a minor surgery. This is done under sedation to make it less painful.
The success of this step is very important. It decides how many eggs can be fertilized. About 80% of mature eggs can fertilize, so the quality and number of eggs matter a lot.
Laboratory Fertilization Methods
After eggs are taken out, they’re fertilized in a lab. There are two main ways to do this: conventional IVF or ICSI. The choice depends on the sperm quality and past fertilization results.
- Conventional IVF mixes eggs with sperm in a dish, letting fertilization happen naturally.
- ICSI injects a single sperm into an egg, helping more in cases of male infertility.
The Critical First 24 Hours
The first 24 hours after fertilization are very important. This is when the fertilized egg starts dividing its cells.
Key events during this time include:
- Fertilization confirmation
- Initial embryo development
- Checking how well fertilization went
The journey from egg retrieval to blastocyst is complex. It involves many stages that need careful medical care. Knowing about these steps helps patients understand their fertility treatment better.
Understanding Day 1: Fertilization Success Rates
Fertilization success rates are key to a successful IVF cycle. On Day 1, the fertilization process is vital. It sets the stage for the embryo’s growth.
Normal Fertilization Expectations (80% Rate)
In a typical IVF cycle, about 80% of mature eggs fertilize successfully. This rate can change due to many factors. These include egg and sperm quality, and the IVF techniques used.
Egg quality is very important for fertilization success. Eggs that are mature and have the right shape are more likely to fertilize.
Signs of Successful Fertilization
Successful fertilization is shown by two pronuclei (2PN) in the egg. This means both the sperm and egg have given their genetic material. This usually happens within 16-18 hours after insemination.
Other signs include:
- Normal cleavage: The fertilized egg starts to divide.
- Symmetrical cell division: Evenly sized cells show healthy development.
Common Reasons for Fertilization Failure
Even with a high fertilization rate, some eggs may not fertilize. Common reasons include:
- Poor sperm quality: Low sperm count, poor motility, or abnormal shape can stop fertilization.
- Egg quality issues: Immature or degenerated eggs may not fertilize.
- Technical issues: Problems in the lab or handling errors can affect fertilization success.
Knowing these factors can help improve the IVF process and increase success rates.
Embryo Development: Days 2-3 Progression
Between days 2 and 3, embryos grow fast, dividing their cells many times. This is a key time for their growth. It’s when they start to get ready to implant in the uterus.
Cell Division and Cleavage Stage
Days 2-3 are when embryos divide their cells in a stage called cleavage. This early stage is vital for the embryo’s growth.
Cell division is a complex process controlled by genes and the environment. Any problem here can hurt the embryo’s chances of survival.
The 6-8 Cell Milestone
By day 3, a healthy embryo should have 6-8 cells. This is a big sign of how well it’s doing.
“The 6-8 cell stage is a critical indicator of embryo quality,” says Medical Expert, a fertility expert. Embryos not reaching this stage might have genetic problems.
Grading Systems for Day 3 Embryos
To check day 3 embryos, experts use a grading system. They look at cell count, how broken the cells are, and if the cells are even.
Embryos are graded from best to worst. Grade 1 is the top, and lower grades mean possible problems.
Knowing how embryos grow from day 2 to 3 is key. By using grading systems, doctors can pick the best embryos for transfer. This helps increase the success of IVF.
The Critical Day 3 to Day 5 Transition
Between day 3 and day 5, embryos go through big changes. These changes are key to the success of IVF treatment.
Metabolic Activation and Genomic Switching
During this time, embryos start using their own genes instead of just maternal ones. This is called genomic switching. They also need more energy, which is a big change.
Metabolic activation means they switch from using pyruvate to glucose for energy. This shows how complex and demanding their needs are. This change is vital for becoming a blastocyst.
Why 50-70% of Embryos Arrest at This Stage
Many embryos struggle to make it from day 3 to day 5. 50-70% arrest at this stage. This is due to genetic issues, poor culture conditions, and the embryo’s inability to adapt.
Learning why this happens is key to improving IVF success. Research on better culture media and lab conditions helps support embryo growth during this tough time.
Cellular Challenges During This Period
Embryos face many challenges during this time. They must:
- Activate their genome and start gene expression
- Make big metabolic changes
- Build the cells needed for blastocyst formation
These challenges show how complex early human development is. We need to create the right lab conditions to help embryos during IVF.
Developmental Stage | Key Characteristics | Challenges |
Day 3 | Cleavage stage, 6-8 cells | Genomic activation, metabolic shift |
Day 5 | Blastocyst formation, inner cell mass, and trophectoderm development | Energy requirements, cellular differentiation |
Understanding the day 3 to day 5 transition helps us grasp IVF’s complexities. This knowledge is vital for improving IVF success and supporting those going through fertility treatments.
Percentage of Embryos That Make It to Day 6
Learning about the percentage of embryos reaching Day 6 helps us understand IVF success. Moving from Day 5 to Day 6 is key for embryo growth.
Extended Culture Success Rates
Extending culture to Day 6 helps pick the best embryos. Research shows that 30-50% of embryos become blastocysts by Day 6.
Embryo quality on Day 6 can be as good as on Day 5. But, extending culture depends on many things, like initial embryo quality and lab conditions.
Day 5 vs. Day 6 Blastocyst Quality
Day 5 and Day 6 blastocysts have different qualities. Day 5 ones are often seen as the best. But, Day 6 ones can also have a good chance of implanting.
Characteristics | Day 5 Blastocysts | Day 6 Blastocysts |
Expansion | More expanded | Less expanded |
Inner Cell Mass | Tighter, more compact | Looser, less compact |
Trophectoderm | Thicker, more cells | Thinner, fewer cells |
Implantation Potentials
There’s debate on the implantation chances of Day 5 and Day 6 blastocysts. Some say Day 5 ones do better. But, others think the difference isn’t big when looking at euploid embryos.
“The implantation chance of Day 6 blastocysts is not much different from Day 5 ones when looking at euploid embryos.”
Looking at Day 6 embryo success, many factors are involved. Understanding these helps us improve IVF treatment plans.
Blastocyst Formation: The 30-50% Success Rate
About 30-50% of fertilized eggs turn into blastocysts during IVF. This is a key stage because it shows if the embryo can implant and lead to pregnancy.
Cellular Composition of Blastocysts
A blastocyst has two main parts: the inner cell mass (ICM) and the trophectoderm (TE). The ICM grows into the fetus. The TE makes the placenta and other tissues needed for growth.
Creating these cells is a complex process. The ICM is vital for the embryo. The TE is key for implantation and making the placenta.
Inner Cell Mass and Trophectoderm Development
The ICM and TE develop through a tightly controlled process. The ICM forms the three germ layers: ectoderm, endoderm, and mesoderm. These layers create all body tissues.
The TE turns into cytotrophoblast and syncytiotrophoblast. These are important for implantation and making the placenta. Both ICM and TE must develop well for a successful pregnancy.
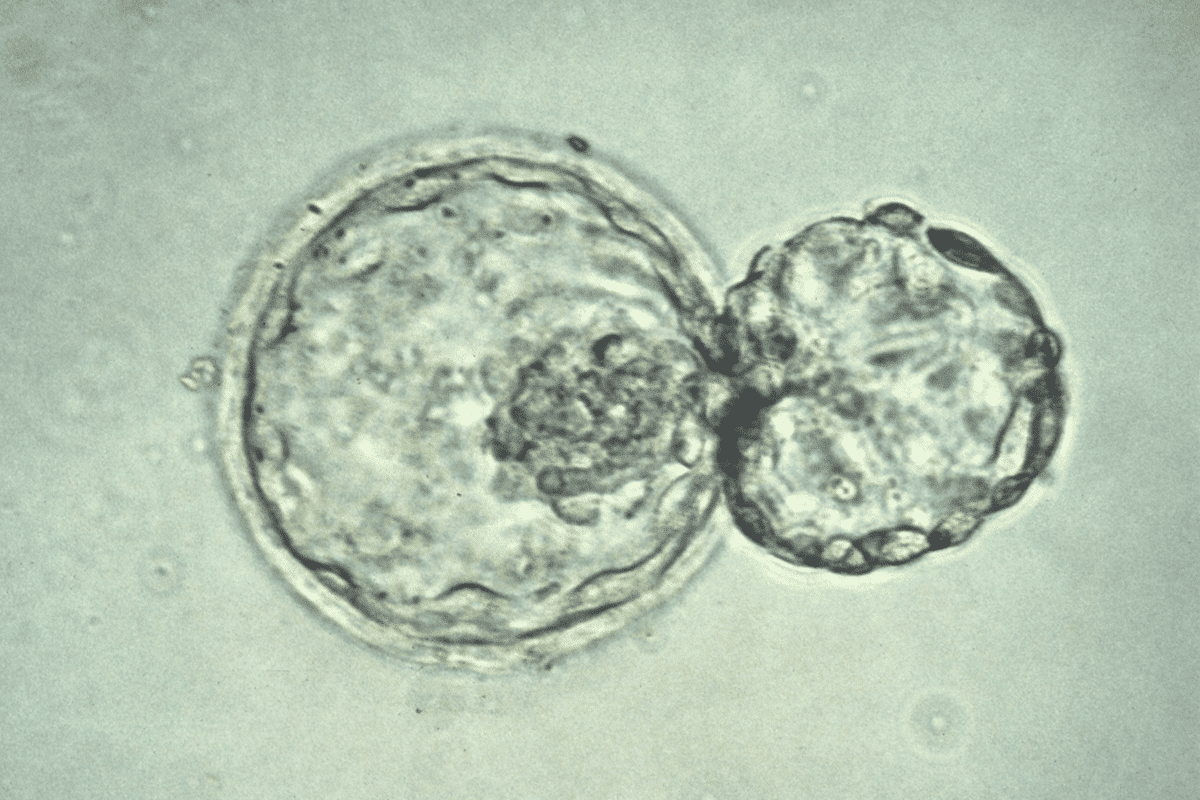
Expansion and Hatching Processes
As the blastocyst grows, it expands and the cells differentiate. The final step before implantation is hatching. This is when the blastocyst comes out of the zona pellucida, a protein layer around it.
Hatching is a critical step for implantation. The embryo’s quality and the zona pellucida’s thickness affect hatching.
Many factors influence blastocyst formation. These include egg and sperm quality, IVF lab conditions, and the embryo’s genetic health.
Factors Influencing Blastocyst Formation | Description | Impact on Success Rate |
Egg Quality | The quality of the egg is key for fertilization and growth. | High-quality eggs boost the chance of successful blastocyst formation. |
Sperm Quality | Sperm quality affects fertilization and embryo growth. | Good sperm quality leads to higher success rates in blastocyst formation. |
Laboratory Conditions | The environment for embryo culture impacts development. | Best lab conditions increase the chance of successful blastocyst formation. |
Age-Related Factors Affecting Blastocyst Development
Maternal age is key in IVF success, mainly in blastocyst development. As women get older, their egg quality and quantity drop. This affects IVF success chances.
Maternal Age Impact on Embryo Quality
Embryo quality depends on the mother’s age. Women under 35 usually have better eggs, leading to higher quality embryos and better IVF success. Older women face more chromosomal issues in embryos, lowering IVF success.
Success Rates by Age Brackets
IVF success rates change with age. Younger women tend to have higher success rates because of better egg quality. Here are common age brackets for IVF success rates:
- Under 35 years: High success rates due to better egg quality.
- 35-37 years: Success rates start to drop as egg quality decreases.
- 38-40 years: Success rates fall further due to lower egg quality and quantity.
- 41-42 years: Success rates drop even more as egg quality and quantity worsen.
- Over 42 years: Success rates are much lower due to poor egg quality.
Advanced Maternal Age Considerations
Women over 35 face unique challenges in IVF. They might need donor eggs or other technologies for better success. Advanced age also raises pregnancy risks, making close monitoring and care vital.
We know age affects IVF success a lot. It’s important for people to understand this when thinking about fertility treatments. Knowing how age impacts embryo quality and IVF success helps patients make better choices for their fertility journey.
Male Factor Influence on Blastocyst Formation
The quality of sperm is key in making embryos into blastocysts during IVF. While female factors get a lot of attention, male factors are just as important for fertility treatment success.
Looking at the male factor’s role, we see several important points. These include sperm quality, DNA damage, and the effect of age.
Sperm Quality Parameters
Sperm quality is checked by count, motility, and shape. Good sperm quality is essential for fertilization and embryo growth. We look at these to see if blastocyst formation is likely.
Having a normal sperm count, good motility, and shape boosts fertilization and embryo growth chances. Studies show men with high-quality sperm do better in IVF, including more blastocysts.
DNA Fragmentation Impact
DNA fragmentation means sperm DNA is broken. High DNA fragmentation can lower IVF success by making fertilization and embryo growth harder.
Research links high DNA fragmentation to lower blastocyst rates and IVF success. We check DNA fragmentation to understand the male factor’s role in IVF.
Paternal Age Considerations
Like maternal age, paternal age is key in IVF success. Older paternal age can lead to lower fertility and more genetic issues in kids.
While studying paternal age’s effect on blastocysts is ongoing, early findings suggest older age may lower IVF success, mainly in high-quality blastocysts.
In summary, the male factor greatly affects blastocyst formation in IVF. By focusing on sperm quality, DNA damage, and age, we can improve IVF success. This helps us give better care to those trying fertility treatments.
Laboratory Conditions and Their Impact on Development
The lab environment is key for embryo growth in IVF. The conditions affect how well embryos grow and survive.
Culture Media Advancements
Culture media is vital in the IVF lab. It gives embryos the nutrients and environment they need. Improved culture media now better mimic the body’s natural environment. This helps embryos grow and survive better.
- Sequential media systems that change composition to meet the evolving needs of the developing embryo
- Addition of antioxidants and other supplements to enhance embryo health
- Development of media that support extended culture to the blastocyst stage
These improvements have led to better IVF success rates. They help create the best conditions for embryo growth.
Oxygen Tension and Temperature Control
Oxygen levels and temperature are key in the lab. Research shows embryos are sensitive to oxygen. Lower oxygen levels (5-7%) are closer to natural conditions and support better growth.
Keeping the temperature around 37°C is also important. But exact temperature control is needed to avoid harm to the embryos.
Laboratory Quality Control Measures
IVF labs follow strict quality control to care for embryos. These include:
- Regular calibration and maintenance of equipment
- Strict protocols for handling and processing embryos
- Continuous monitoring of laboratory conditions, including temperature, oxygen levels, and air quality
By controlling the lab environment, we can increase the chances of successful embryo development. This improves IVF outcomes.
Genetic Factors in Embryo Attrition
Understanding the genetic factors that affect embryo development is key to better IVF results. Embryo attrition, or when embryos fail to develop, is a big challenge in fertility treatments. Genetic factors are a big part of this issue.
Chromosomal Abnormalities and Development
Chromosomal abnormalities are a major genetic factor in embryo attrition. These happen when there are errors in the number or structure of chromosomes. Such errors can cause developmental problems, as the embryo may not have the right genetic blueprint for growth.
Studies show that many embryos have chromosomal abnormalities. This can lead to failed implantation or miscarriage. The most common issue is aneuploidy, where an embryo has the wrong number of chromosomes.
Mosaicism in Early Embryos
Mosaicism is when an embryo has both normal and abnormal cells. This can happen due to errors in cell division early in development. Mosaicism can affect the viability of the embryo, depending on the number and spread of abnormal cells.
Research shows mosaicism is common in early embryos. It makes it hard to assess embryo viability during IVF, as not all abnormal cells can be detected by standard tests.
The Role of PGT-A Testing
Preimplantation Genetic Testing for Aneuploidy (PGT-A) is a tool used to find chromosomal abnormalities in embryos before transfer. PGT-A tests a small sample of cells from the embryo to check its chromosomal status.
PGT-A testing can boost IVF success rates. It lets us choose embryos with the best chance of successful implantation and development. It’s very helpful for those with a history of miscarriage or failed IVF cycles.
Key benefits of PGT-A testing include:
- Improved selection of viable embryos
- Reduced risk of chromosomal abnormalities
- Enhanced IVF success rates
By tackling genetic factors in embryo attrition, we can make fertility treatments more effective. This helps more people achieve their dream of having a healthy family.
Managing Expectations: What IVF Patients Should Know
IVF patients often feel unsure about their treatment outcomes. It’s key to set realistic expectations. We guide patients through their IVF journey, focusing on what affects success rates.
Realistic Outcomes Based on Starting Numbers
The number of eggs retrieved in an IVF cycle is a big factor in success. More eggs mean better chances of healthy embryos. But, not all eggs will turn into viable embryos.
Key statistics to consider:
- Women under 35 usually have higher success rates because of better egg quality.
- The average number of eggs retrieved is between 10 to 20, but it can vary.
- About 30-50% of fertilized eggs become blastocysts.
Emotional Preparation for Attrition
The IVF process can be emotionally tough, mainly due to embryo attrition. It’s important for patients to prepare emotionally for the possibility of embryo loss.
Coping strategies include:
- Seeking support from counseling services or support groups.
- Maintaining open communication with your fertility specialist.
- Focusing on the steps you can control, such as lifestyle adjustments and adherence to treatment plans.
Decision-Making Around Day 3 vs. Day 5 Transfers
Choosing between a Day 3 or Day 5 embryo transfer is a big decision. It depends on the number and quality of embryos.
Transfer Day | Advantages | Considerations |
Day 3 | Less time in culture, potentially more embryos available for transfer. | May not accurately reflect embryo viability. |
Day 5 | Allows for better selection of viable embryos, potentially higher success rates. | Fewer embryos may be available due to attrition. |
Understanding these factors and keeping expectations realistic helps IVF patients navigate their journey better.
Conclusion: The Blastocyst Milestone in Fertility Treatment
Reaching the blastocyst stage is key in fertility treatment, like IVF. It shows a big step towards a successful pregnancy. We’ve talked about how embryos grow from fertilization to the blastocyst stage and what affects this journey.
The blastocyst stage is important because it means an embryo has passed early challenges. It has a better chance of implanting. Knowing what affects blastocyst formation, like age and sperm quality, helps improve IVF success.
Understanding the blastocyst stage and its factors helps both patients and doctors make better IVF choices. This knowledge leads to more effective treatments and better fertility care results.
FAQ
What percentage of fertilized eggs make it to the blastocyst stage?
About 30-50% of fertilized eggs turn into blastocysts.
How many fertilized eggs make it to day 5?
By day 5, around 30-50% of fertilized eggs have reached the blastocyst stage.
What is the IVF fertilization rate?
IVF fertilization rates are usually 70-80%. This means 70-80% of eggs are fertilized during IVF.
What is IVF attrition?
IVF attrition is when embryos are lost during IVF. This can happen for many reasons, like genetic issues or lab conditions.
How many blastocysts are normal for IVF?
For IVF, having 2-5 high-quality blastocysts is considered good.
How many embryos make it to day 5?
The number of embryos to day 5 varies. It depends on how many eggs were fertilized and retrieved. But usually, 30-50% make it.
What percent of fertilized eggs make it to blastocyst?
About 30-50% of fertilized eggs become blastocysts.
How many fertilized eggs make it to blastocyst?
Around 30-50% of fertilized eggs become blastocysts.
What is the attrition rate in IVF?
The attrition rate in IVF is the percentage of embryos lost. It changes based on age, embryo quality, and lab conditions.
How does maternal age affect blastocyst development?
Maternal age greatly affects blastocyst development. Success rates drop after 35.
What is the impact of male factors on blastocyst formation?
Male factors like sperm quality and DNA fragmentation affect blastocyst formation and IVF success.
How do laboratory conditions affect embryo development?
Lab conditions, like culture media and temperature, are key for embryo development and IVF success.
What is the role of PGT-A testing in IVF?
PGT-A testing finds genetic issues in embryos. It helps choose healthy embryos for transfer, boosting IVF success.
How many eggs are typically retrieved during IVF?
IVF usually retrieves 8-12 eggs. But numbers can vary.
What are the success rates for IVF with different numbers of eggs retrieved?
IVF success rates change with egg numbers. More eggs often mean higher success rates. But age and embryo quality also play a part.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8236141/).