Did you know that over 1.9 million new cancer cases are diagnosed annually in the United States alone? Positron Emission Tomography (PET) scans are key in finding cancer. But, they can’t always give a clear answer. They show where cancer might be by looking at how active cells are.
Biopsies are needed to confirm cancer. They take tissue samples from the suspected area. These samples are then checked under a microscope. When Biopsy is Needed After PET Scan. This confirms cancer and helps figure out what type and stage it is, guiding treatment.
Key Takeaways
- PET scans are vital for detecting cancer but may not always provide a definitive diagnosis.
- Biopsies are often necessary after a PET scan to confirm the presence and type of cancer.
- Tissue confirmation through biopsy is essential for accurate cancer diagnosis and treatment planning.
- PET scans and biopsies complement each other in the cancer diagnosis process.
- A PET positive result may require a biopsy to rule out false positives.
Understanding PET Scans in Cancer Diagnosis
PET scans are a key tool in finding and checking how far cancer has spread. They show where cells are working hard, which is a sign of cancer. This is because cancer cells use more energy than regular cells.
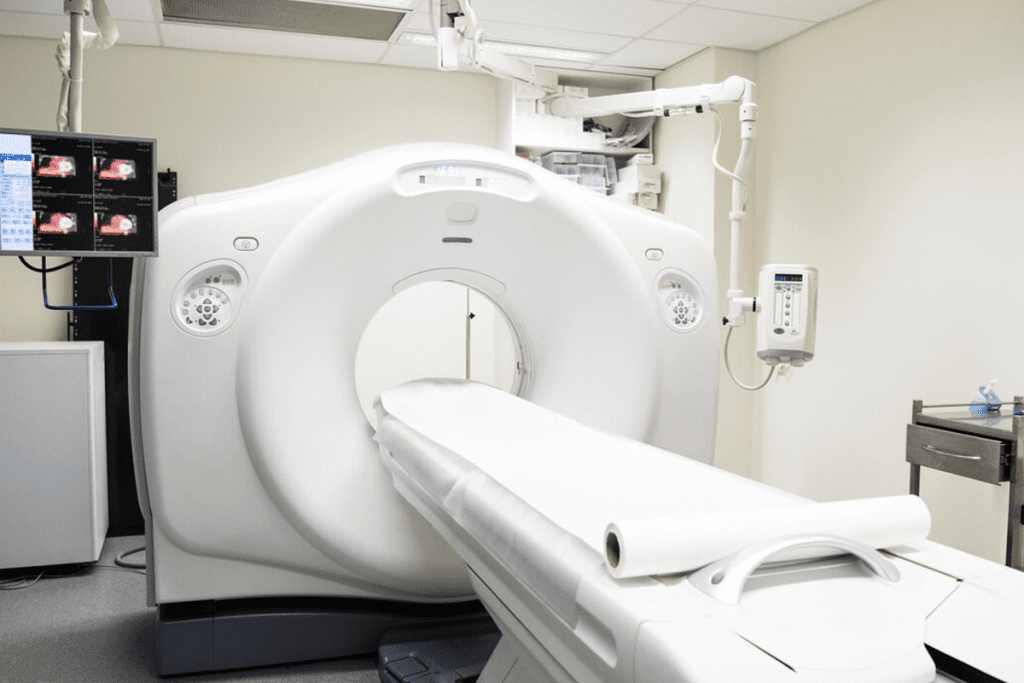
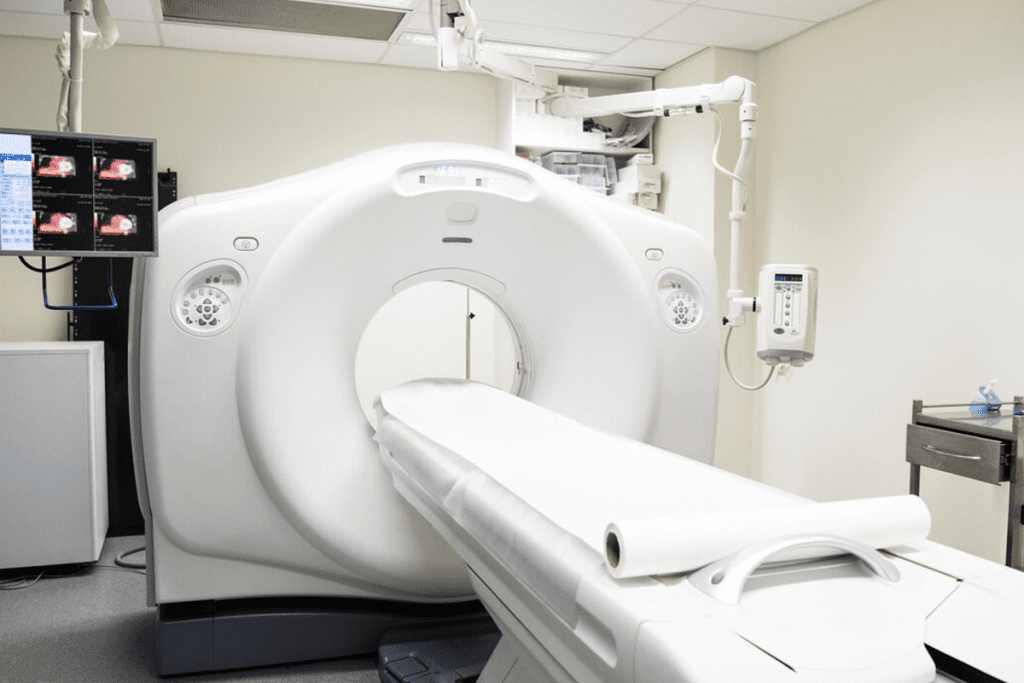
How PET Scans Work and What They Detect
PET scans use a tiny bit of radioactive sugar to spot cancer cells. Cancer cells eat more sugar because they grow fast. This makes them show up bright on the scan.
First, a radioactive sugar is injected into your blood. Then, cells all over your body soak it up. Cancer cells, being more active, take in more sugar. This makes them glow on the scan.
Advantages and Limitations of PET Imaging
PET scans are great for finding cancer because they can see how active cells are. They can scan your whole body and show how tumors are working. But, they’re not perfect.
Key Advantages:
- High sensitivity to metabolic changes
- Whole-body scanning capability
- Assessment of tumor metabolic activity
Limitations:
- Potential for false positives
- Potential for false negatives
- Limited anatomical detail
| Characteristics | PET Scan |
| Sensitivity to Metabolic Changes | High |
| Whole-Body Scanning | Yes |
| Anatomical Detail | Limited |
The Relationship Between PET Scans and Biopsies
Understanding how PET scans and biopsies work together is key for accurate cancer diagnosis. We’ll look at how these tools help each other in finding cancer.
Complementary Roles in Cancer Diagnosis
PET scans and biopsies have different but important roles in cancer diagnosis. PET scans show how active tumors are, helping spot possible cancer areas. But, a biopsy is needed to get a clear diagnosis through histological confirmation and tissue analysis.
Biopsies take tissue samples for detailed checks. This lets pathologists look at the tumor’s cells and find key details. These details are vital for treatment planning.
The Diagnostic Pathway: From Imaging to Tissue Sampling
The cancer diagnosis journey often starts with imaging, like PET scans. If a PET scan finds suspicious spots, a biopsy follows to get tissue for study. This two-step process makes sure the diagnosis is solid, based on both imaging and tissue evidence.
The table below shows how PET scans and biopsies work together in diagnosis:
| Diagnostic Tool | Purpose | Information Provided |
| PET Scan | Identify metabolically active areas | Functional information about tumor activity |
| Biopsy | Obtain tissue for histological examination | Definitive diagnosis through tissue analysis |
By using PET scan and biopsy results together, doctors can get a full picture of the cancer. This helps plan better treatments.
When Biopsy is Needed After PET Scan
PET scans give us important information. But, sometimes, we need a biopsy for a clear cancer diagnosis. The choice to do a biopsy depends on the PET scan results, medical history, and how the patient feels.
Clinical Scenarios Requiring Tissue Confirmation
Some PET scan results mean we need a biopsy to confirm tissue. These include:
- Suspicious lesions or masses
- Abnormal uptake patterns
- Lesions in critical or hard-to-reach areas
For example, a PET scan might show a lung nodule that looks like cancer. In such cases, a biopsy is key to confirm the diagnosis and plan treatment.
Medical Guidelines and Standard Protocols
Medical societies and guidelines help decide when a biopsy is needed after a PET scan. For example, the National Comprehensive Cancer Network (NCCN) has guidelines for diagnosing and treating different cancers. These include when to do a biopsy.
| Cancer Type | PET Scan Findings | Biopsy Recommendation |
| Lung Cancer | Suspicious nodule | Yes, for tissue confirmation |
| Lymphoma | Abnormal lymph node uptake | Yes, for histological diagnosis |
| Colorectal Cancer | Metastatic lesions | Yes, if primary tumor unknown |
Interpreting PET Scan Results: What the Numbers Mean
When we look at PET scans, we check SUV values and patterns to see how active lesions are. This helps us decide if we need to do a biopsy.
Understanding SUV Values and Uptake Patterns
SUV stands for Standardized Uptake Value. It shows how much tracer a tumor or lesion takes in. A higher SUV value often means the tumor is more active, which could be cancerous. But, SUV values alone aren’t enough. We need to look at other signs and symptoms too.
Patterns of uptake are also important. For example, a tumor that takes in the tracer unevenly might be more suspicious than one that takes it evenly. The way and how much the tumor takes in the tracer can tell us a lot about it.
What Constitutes a “Suspicious” Finding Requiring Biopsy
A suspicious PET scan finding usually has high SUV values and odd uptake patterns. But, whether to do a biopsy depends on many things. This includes the patient’s history, where and how big the tumor is, and what other tests show.
For instance, a small tumor with a high SUV value in a hard-to-reach spot might not get biopsied. But, a bigger tumor with a lower SUV value in an easier spot might get checked.
“The integration of PET scan results with clinical judgment is key for deciding on a biopsy. It’s not just the numbers; it’s how we understand them in context.”A nuclear Medicine Specialist
Getting the most out of PET scan results means looking at SUV values, patterns, and the bigger picture. This careful look is vital for deciding if a biopsy is needed.
Limitations of PET Scans That Necessitate Biopsies
PET scans are a key tool in finding cancer. But, they’re not perfect and sometimes need a biopsy for more info. They show how active tissues are, helping spot cancer. Yet, they can give wrong results sometimes.
PET scans can say there’s cancer when there isn’t, or miss it. This happens for many reasons. It depends on the cancer type, the scan tech, and the patient’s health.
Non-Malignant Causes of Increased Uptake
False positives can happen when PET scans show cancer where there isn’t any. This can be because of inflammation or infection. For example, pneumonia can make lung tissue look like cancer on a scan.
- Inflammatory Conditions: Sarcoidosis or rheumatoid arthritis can cause false positives.
- Infections: Bacterial, viral, or fungal infections can also lead to false positives.
- Other Causes: Recent surgery, trauma, or benign tumors can cause increased uptake.
When Cancer Evades Detection
False negatives happen when cancer isn’t seen because it doesn’t show up well on scans. This is often with slow-growing tumors or cancers that don’t use much glucose.
The ability of PET scans to find cancer depends on several things. The tumor size, type, and the patient’s health all play a role. Small tumors or those with low activity might not show up.
- Tumors with low glucose metabolism may not be visible on PET scans.
- Small tumors can be missed due to limitations in PET scan resolution.
- Certain cancer types may not exhibit high enough metabolic activity to be detected.
The Critical Role of Histological Confirmation in Cancer Diagnosis
Getting a cancer diagnosis through histological confirmation is very important. It gives us the detailed molecular and genetic info needed for targeted treatments. This process involves looking at tissue samples from biopsies to find out if there’s cancer, what type it is, and its characteristics.
Why Tissue Analysis Remains the Gold Standard
Biopsy remains the top choice for cancer diagnosis because it gives a clear diagnosis. Biopsies not only tell us if there’s cancer but also about its biology, like genetic mutations and molecular traits. This info is key for making effective treatment plans.
A study in a Journal of says, “examining tumor tissue is key for finding genetic changes that therapies can target.”
“The mix of histological and molecular analysis in clinical practice has changed oncology. It’s led to personalized medicine that boosts patient results.”
Molecular and Genetic Information Only Biopsies Can Provide
Biopsies are special because they give us molecular and genetic info about tumors. This info is vital for picking the right treatments, like targeted therapies and immunotherapies. The molecular traits of a tumor greatly affect treatment choices, making biopsies essential in today’s oncology.
| Information Type | Description | Clinical Significance |
| Genetic Mutations | Specific DNA changes in cancer cells | Helps find therapy targets |
| Molecular Characteristics | Presence of certain proteins or genes in cancer cells | Helps decide treatment and predict outcomes |
| Tumor Biomarkers | Substances made by tumors or in response to them | Used for diagnosis, tracking treatment, and finding recurrence |
As we move forward in oncology, the role of histological confirmation through biopsy will stay vital. It’s key for getting the accurate and detailed info needed for effective cancer treatment.
Types of Biopsies Performed After Suspicious PET Findings
After a PET scan finds something that might be cancer, doctors might suggest several biopsies to be sure. The type of biopsy depends on where and what the suspicious spot looks like.
Fine Needle Aspiration (FNA) Procedures
Fine Needle Aspiration (FNA) is a small procedure. It uses a thin needle to take cells from the area in question. It’s good for spots that are easy to get to or near the skin’s surface.
FNA is often guided by ultrasound or CT scan to place the needle right. It can give a quick answer, but might not always have enough tissue for a full look.
Core Needle Biopsy Techniques
Core Needle Biopsy uses a bigger needle than FNA to get a piece of tissue. This gives more tissue for detailed study. It’s great for looking at things like lymphoma or when you need to see the tissue’s structure.
Core needle biopsy is also guided by imaging to make sure it’s done right. It’s useful for getting a closer look at the tissue.
Surgical Biopsy Options
Surgical biopsy means taking out a bigger piece of tissue or the whole spot. This can be done with a big cut or a small, laparoscopic way.
Surgical biopsy gives the most tissue for study. It’s best when other methods don’t work or when the spot is hard to reach with a needle.
PET-Guided Biopsy Approaches
PET-guided biopsy uses PET scans to guide the biopsy. It targets the most active parts of a tumor. This makes sure the biopsy gets the most important tissue.
PET-guided biopsy is good for spots that are hard to get to or when there are many areas to check. It makes the biopsy more accurate by focusing on the right areas.
Cancer-Specific Considerations for Post-PET Biopsies
Different cancers need different approaches for diagnosis. The type of cancer suspected is key in deciding if a biopsy is needed after a PET scan. We’ll look at the specific needs for various common cancers.
Lung Cancer and Pulmonary Nodules
Lung cancer is a big problem worldwide, and PET scans help diagnose it. If a PET scan shows a suspicious nodule, several things are considered. Fine-needle aspiration (FNA) is often used for peripheral nodules, while central lesions might need a core needle biopsy or surgery.
Lymphoma and Lymph Node Assessment
Diagnosing lymphoma involves checking lymph nodes, which can be tricky. PET scans help find active nodes, but a biopsy is needed for a precise diagnosis. Excisional biopsy is usually the best choice for lymphoma diagnosis to get enough tissue for tests.
Colorectal Cancer and Metastatic Disease
PET scans are key in finding metastatic disease in colorectal cancer, which affects treatment plans. If metastatic lesions are found, a biopsy might be needed to confirm the diagnosis. The choice between percutaneous biopsy and surgical biopsy depends on the lesion’s location and the patient’s condition.
Other Common Malignancies
Other cancers, like breast, melanoma, and prostate, also have specific biopsy needs after a PET scan. For example, in breast cancer, a biopsy might be needed to check PET-avid lesions. In melanoma, it helps confirm metastatic disease. The biopsy approach varies based on the cancer type and the patient’s situation.
In conclusion, whether to do a biopsy after a PET scan depends on the cancer type and its characteristics. Knowing these specific considerations is key for accurate diagnosis and effective treatment.
Scenarios Where Biopsy May Be Deferred Despite Positive PET Results
For patients with a history of cancer, a positive PET scan doesn’t always mean they need a biopsy. The decision depends on the cancer’s typical spread patterns. We’ll look at when skipping a biopsy is considered, based on certain factors.
Known Cancer with Characteristic Metastatic Patterns
When a patient has a known cancer, metastasis often follows certain paths. For example, lung cancer often spreads to the brain, liver, or adrenal glands. If a PET scan shows this, doctors might not always need to do a biopsy, depending on the patient’s health.
Anatomically Challenging or High-Risk Biopsy Locations
Biopsies can be risky in hard-to-reach or sensitive areas. For instance, tumors near major blood vessels or nerves are tricky to biopsy. Doctors must weigh the benefits against the risks of complications.
| Clinical Scenario | Considerations for Deferring Biopsy | Potential Risks of Biopsy |
| Known cancer with typical metastatic patterns | Clinical diagnosis based on imaging and history | Risk of unnecessary procedure |
| Anatomically challenging biopsy locations | Risk of complications, difficulty in accessing the site | Bleeding, infection, damage to surrounding structures |
In conclusion, deciding to skip a biopsy after a positive PET scan is complex. It depends on the patient’s situation, like known cancer and where the tumor is. Doctors aim to balance benefits and risks for the best care.
Risks and Complications of Post-PET Biopsies
Deciding on a biopsy after a PET scan is a big choice. It’s important to know the risks and benefits. This helps patients make smart decisions about their health.
Common Side Effects and Possible Complications
Biopsies can have risks, like pain or swelling at the site. Serious problems, though rare, can happen. These might include infection or damage to nearby areas.
For example, lung biopsies might cause a collapsed lung. It’s key for patients to talk about these risks with their doctors.
“The chance of problems from a biopsy is small, but it’s there,” an expert in radiology. “We do everything we can to avoid risks. But patients should know what might happen.”
Risk-Benefit Analysis for Different Patient Populations
The risks of biopsies differ for each person. Those with bleeding issues or on blood thinners face higher bleeding risks. People with weak immune systems are more likely to get infections. These factors are important when deciding if a biopsy is needed.
We look at many things when weighing risks and benefits. This includes the patient’s health, the suspected condition, and how the biopsy results will affect treatment. Often, getting a clear diagnosis is worth the risks of the biopsy.
For cancer patients, a biopsy can be key in choosing the right treatment. Knowing the cancer’s details can lead to better treatment plans.
In summary, biopsies have risks, but careful analysis helps us make good choices. By understanding the risks for different people and the benefits of getting a diagnosis, we can handle post-PET biopsies better.
The Patient Experience: Preparing for a Biopsy After PET
Thinking about a biopsy after a PET scan can be scary. But, knowing what to expect can help. Preparing for a biopsy involves several steps to make the process smoother. This knowledge can help you feel less anxious and more in control.
Before the Procedure: Preparation and Expectations
Your healthcare team will give you specific instructions before the biopsy. These might include:
- Fasting or dietary restrictions for a certain period before the procedure.
- Medication management, including whether to continue or stop certain medications.
- Arranging for transportation home after the procedure, as you may be advised not to drive.
- Signing consent forms after discussing the procedure’s risks and benefits with your doctor.
It’s important to follow these instructions carefully and ask any questions you may have. Being well-prepared can significantly reduce your stress levels.
During the Biopsy: What Actually Happens
During the biopsy, you’ll be positioned to make it easy to access the site. The area will be cleaned and sterilized, and local anesthesia will be given to numb it. You might be awake or sedated, depending on the type of biopsy. Our medical team will watch over you to ensure your comfort and safety.
The biopsy involves using a needle or surgical instrument to collect tissue or cell samples. The procedure’s duration can vary depending on the complexity and location of the biopsy site.
After the Procedure: Recovery and Results
After the biopsy, you’ll be taken to a recovery area for monitoring. You might feel some discomfort or soreness at the biopsy site, which can be managed with over-the-counter pain relievers. Your healthcare team will give you specific post-procedure care instructions, including:
- Wound care to prevent infection.
- Activity level restrictions to avoid complications.
- Follow-up appointments to check on your recovery and discuss the biopsy results.
The biopsy results usually take a few days to a week to process. Your healthcare provider will talk to you about the results, explaining what they mean for your diagnosis and treatment plan. Receiving your results can be a significant moment, and we’re here to support you through it.
Understanding what to expect during the biopsy process can help you prepare better. Our team is committed to providing you with the care and support you need every step of the way.
Emerging Technologies Changing the PET-Biopsy Paradigm
Looking ahead, new technologies will greatly change how we diagnose cancer. These tools are not just better for patients. They are also changing how we see cancer diagnosis.
Advances in PET Technology and Diagnostic Accuracy
New PET technology has made it more accurate. High-resolution PET scanners can spot smaller tumors and give detailed info on tumor activity. This helps in finding and staging cancer early, sometimes avoiding the need for biopsies.
New tracers are also being developed. These go beyond the usual FDG tracer. They can target specific cancer cells, giving a deeper look into tumor biology.
- Improved spatial resolution
- Enhanced sensitivity to metabolic changes
- Expanded tracer options for specific cancer types
Liquid Biopsies and Other Non-Invasive Alternatives
Liquid biopsies are a big step forward in cancer diagnosis. They check for cancer or track its growth by looking at DNA in the blood. This method could replace or add to traditional biopsies, making it easier for patients.
“Liquid biopsies represent a significant shift in our approach to cancer diagnosis, enabling earlier detection and more precise monitoring of treatment response.”
Oncologist
Other non-invasive methods are also being looked into. This includes new imaging and checking other body fluids. These new tools could make diagnosing cancer less invasive.
- Liquid biopsies for early cancer detection
- Advanced imaging modalities
- Analysis of biomarkers in bodily fluids
As these technologies get better, they will change how we use PET-biopsies. This means patients will get more accurate and less invasive tests. It could also lead to better cancer care outcomes.
Insurance Coverage and Costs for Post-PET Biopsies in the US
When it comes to biopsies after PET scans, patients face many financial hurdles. They must think about insurance coverage and what they’ll have to pay out of pocket. Knowing these costs is key to handling the financial side of medical care.
Medicare and Private Insurance Policies
Insurance for biopsies after PET scans differs a lot between Medicare and private insurance. Medicare usually covers biopsies if they’re medically needed. But, patients might have to pay for things like deductibles and copays.
Private insurance also covers biopsies, but how much depends on the plan. Some plans might need you to get approval first or have certain rules. It’s important to check your policy to see what’s covered.
- Review your insurance policy to understand biopsy coverage.
- Check if pre-authorization is required for the biopsy.
- Understand your out-of-pocket expenses, including deductibles and copays.
Managing Out-of-Pocket Expenses and Financial Resources
Handling the costs of biopsies can be tough. There are ways to help with these expenses. Financial counseling services are found in many hospitals to help with insurance and finding financial help.
Also, some groups help patients with cancer treatment costs, including biopsies. You can look up these groups and see if you qualify for help.
- Seek financial counseling services at your healthcare provider.
- Research organizations that offer financial assistance for cancer patients.
- Apply for financial assistance programs if you are eligible.
By knowing about insurance and looking into financial help, patients can handle the costs of biopsies after PET scans better.
Conclusion: Navigating Decisions About Post-PET Biopsies
Deciding on a biopsy after a PET scan is a big choice. We’ve looked at how PET scans help find cancer and how biopsies confirm it. This helps us understand the importance of each step.
Every patient’s situation is different. So, deciding on a biopsy needs a personal touch. Knowing the cancer’s details is key to planning the right treatment.
Patients need to know the whole process from imaging to getting tissue samples. This helps decide when a biopsy is needed or if it can wait. It’s also important to think about the risks and new technologies that might change things.
By using all the data from PET scans, biopsies, and other tests, we can make better treatment plans. This approach helps give patients the best care possible for their cancer.
FAQ
Is a biopsy always necessary after a PET scan?
No, a biopsy isn’t always needed after a PET scan. We look at many things, like the PET scan results and the patient’s history. Each case is different, so we decide what’s best for each person.
What does a PET scan detect, and how does it relate to cancer diagnosis?
A PET scan finds cells that are very active, which might mean cancer. But, it’s not a sure way to say you have cancer. It shows where there might be cancer, and then a biopsy is needed to confirm it.
How do PET scans and biopsies complement each other in cancer diagnosis?
PET scans show how active tumors are. Biopsies give us the exact details of the tissue. Together, they help us find cancer, plan treatment, and track how the disease is doing.
How are PET scan results interpreted, and what do SUV values indicate?
We look at SUV values to understand how active tissues are. Higher values mean tumors might be more aggressive. But, SUV values alone can’t confirm cancer. We use them with other information to make a diagnosis.
What types of biopsies are performed after suspicious PET findings?
There are many biopsy types, like fine-needle aspiration and core needle biopsy. The choice depends on the tumor’s location and the patient’s health.
Are there scenarios where a biopsy may be deferred despite positive PET results?
Yes, sometimes we might not do a biopsy right away. This could be if the cancer is known or if getting a biopsy is very hard. We make this decision based on the patient’s situation.
What are the risks and complications associated with biopsies?
Biopsies can have risks like bleeding or infection. We weigh the risks and benefits for each patient to make sure they’re safe
How can patients prepare for a biopsy after a PET scan?
Patients should follow their doctor’s instructions, which might include stopping certain medicines or fasting. Knowing what to expect can help make the process easier.
Are there emerging technologies that may change the PET-biopsy paradigm?
Yes, new PET tech and tests like liquid biopsies are changing how we diagnose. They might make diagnosis more accurate and less invasive, improving care.
What are the financial considerations for biopsies, and how can patients navigate costs?
Biopsy costs vary based on location, insurance, and type of biopsy. Patients should talk to their doctor about costs and what’s covered by insurance. This helps understand the financial side and find help if needed.
References
- Fei, B., Wang, J., Lee, Z., et al. (2017). PET molecular imaging“directed biopsy: A review. AJR American Journal of Roentgenology, 209(5), 994“1001. https://pmc.ncbi.nlm.nih.gov/articles/PMC5669368/ PMC+1
- Wu, M., Zhou, J-G., Zhou, C., et al. (2019). PET/CT-guided versus CT-guided percutaneous core biopsies in evaluation of hypermetabolic bone lesions: diagnostic performance and safety. Cancer Imaging, 19, 65. https://cancerimagingjournal.biomedcentral.com/articles/10.1186/s40644-019-0253-1 BioMed Central
- Cerci, J. J., Furtado, C. G., de Oliveira, L. F., et al. (2021). PET/CT-guided biopsy of lung lesions requires fewer inconclusive biopsies compared to CT guidance: Results from a prospective trial. Journal of Nuclear Medicine, 62(8), 1057“1063. https://jnm.snmjournals.org/content/62/8/1057 Journal of Nuclear Medicine
- Wang, Z., Ji, L., Bai, L., et al. (2024). PET/CT-aided biopsy of lung lesions enhances diagnostic efficacy, especially for lesions > 3 cm. Frontiers in Oncology. https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1296553/full Frontiers
- Fielding, D., Waller, J., Kinsella, J., et al. (2025). Biopsy decision for intermediate“high-risk lung nodules: PET-FIRST study insights. BMJ Open Respiratory Research, 12(1), e002553. https://bmjopenrespres.bmj.com/content/12/1/e002553 BMJ Open Respiratory Research























