The journey toward autologous stem cell transplant or therapy begins with a comprehensive consultation.
Send us all your questions or requests, and our expert team will assist you.

Regenerative medicine is powerful, but it is not a magic wand that works for everyone. The success of Stem Cell Therapy depends 50% on the quality of the cells and 50% on the Selection of the Patient.
At Liv Hospital, we operate on a principle of “Radical Honesty.” We do not offer stem cell therapy to patients whose conditions are too advanced to respond, or whose underlying health would prevent the cells from working. Before a single cell is harvested, you undergo a comprehensive “Regenerative Potential” Assessment.
This diagnostic phase is designed to answer three critical questions:
By using advanced imaging, functional testing, and biomarkers, we create a personalized roadmap. If we believe standard surgery (like a knee replacement) would give you a better result, we will tell you. We measure our success by your outcome, not by the number of procedures we perform.
For joint pain, an X-ray is often insufficient. It shows bones, but it misses the soft tissues—cartilage, meniscus, and ligaments—that stem cells target.

We use 3-Tesla MRI scanners to grade your injury with precision.

Sometimes the MRI looks bad, but the patient walks fine. Sometimes the MRI looks okay, but the patient limps severely.
Stem cells are the “seeds.” Your body is the “soil.” If the soil is toxic (high inflammation, uncontrolled sugar), the seeds won’t grow.
Before therapy, we check specific biomarkers:
We screen every patient for blood-borne viruses (HIV, Hepatitis B/C, Syphilis).

Send us all your questions or requests, and our expert team will assist you.
For anti-aging and hair loss, we move beyond “mirror checks” to digital quantification.
For hair loss patients.
For facial rejuvenation.
One of the biggest differences between Liv Hospital and a standard clinic is that we count your cells. Diagnosis determines the dose.
After harvesting your tissue (fat or marrow), we take a sample to our GMP Lab.
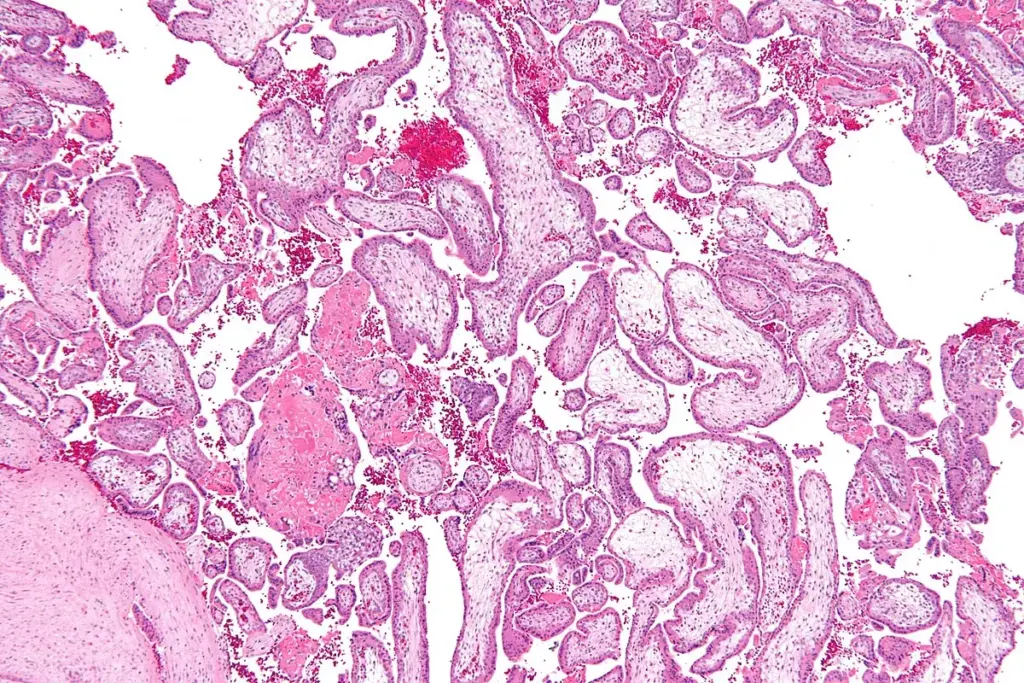
Stem cells release Growth Factors. These are powerful stimulants. If there is a hidden cancer in the body, growth factors could theoretically make it grow faster.
For complex cases, the decision is not made by a single doctor. It is a team effort.
We know you have limited time. We streamline the “Go/No-Go” process.
No. For orthopedic or aesthetic conditions, we rely on non-invasive imaging (MRI, Ultrasound) and blood tests. A biopsy is only needed if we suspect a suspicious lesion (like a tumor) that needs to be ruled out before treatment.
For a preliminary opinion, yes. But for a final decision, an MRI is usually required. An X-ray only shows bone. Stem cell therapy targets cartilage, tendons, and ligaments—tissues that are invisible on X-ray. If you don’t have a recent MRI (within 6 months), we will perform one at Liv Hospital.
We pride ourselves on ethical practice. If your knee is “bone-on-bone,” we will recommend Robotic Knee Replacement. If your hair follicles are dead, we will recommend a Hair Transplant. We will always offer the treatment that has the highest statistical chance of success for your specific anatomy.
Stem cells are very sensitive to their environment. High blood sugar (Hyperglycemia) creates a toxic, inflammatory environment that can kill the injected stem cells or make them dormant. Controlling your sugar before the procedure protects your investment.
Most private insurance companies cover the diagnostic portion (MRI, Doctor Consultation, Blood Tests) as standard medical care. However, the stem cell therapy itself is often considered “experimental” or “aesthetic” and is usually self-pay. Our international team can help clarify your coverage.

Key Takeaways The Life and Career of Kamar de los Reyes Kamar de los Reyes built a dynamic career across television, film, and video games.
Celebrities often shape public conversations far beyond entertainment. Some use their visibility to spotlight important medical conditions and encourage broader awareness. Turner Syndrome, a genetic

Welcome to our article on Jamie Lee Curtis and Androgen Insensitivity Syndrome (AIS), a rare genetic intersex condition. In this piece, we explore AIS, its

Over the years, speculation has surrounded this talented actress and her alleged facial scar. In this piece, we aim to separate fact from fiction and

Discover inspiring stories of public figures and individuals associated with Noonan Syndrome awareness. At Liv Hospital, we believe that a diagnosis does not define a

Moises Arias: Advocacy in Cystic Fibrosis Awareness Moises Arias has been widely recognized for his work in film and television. In recent years, discussions have

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)