Essential guide to Stem Cell Recovery and Follow-up, including strict infection control, lifestyle changes, and long-term screening to prevent complications and recurrence.
Send us all your questions or requests, and our expert team will assist you.

Regenerative medicine is fundamentally different from surgery or pharmaceuticals. When you take a painkiller, the effect is immediate but temporary. When you have surgery, the structural fix is instant, but the trauma is high.
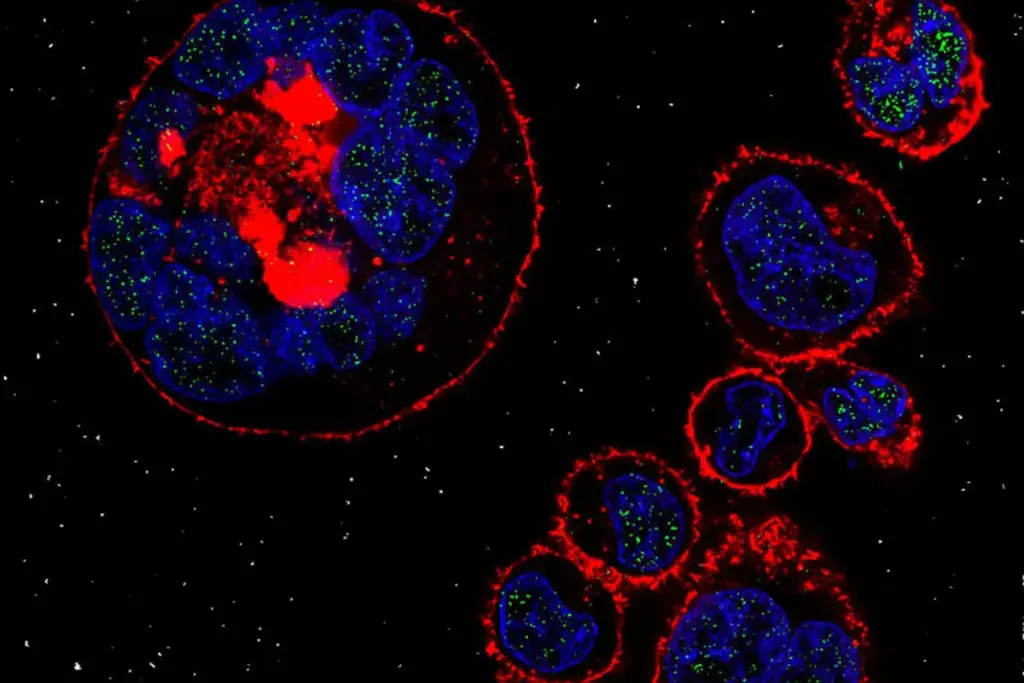
Stem Cell Therapy is a biological signal. The injection itself is merely the “start button.” The actual work—the migration of cells, the release of growth factors, and the rebuilding of tissue—happens over the weeks and months after you leave Liv Hospital.
Therefore, Recovery is not a passive waiting game; it is an active phase of cultivation. You have planted the seeds; now you must water the soil. At Liv Hospital, we guide you through this delicate period with precise protocols on nutrition, movement, and medication management to ensure the cells survive and thrive.
Contrary to popular belief, you may actually feel more pain for the first few days after the procedure. This is normal and even desirable.

This is the most critical instruction we give.

Send us all your questions or requests, and our expert team will assist you.
For knee, hip, or shoulder injections, the goal is to move the fluid around without crushing the new cells.
For facial rejuvenation and hair restoration, the recovery is visual.
For autoimmune disease or wellness infusions, there is no localized pain.
You have expensive cells in your body; don’t feed them junk food.
Patients often ask: “It’s been 2 weeks, why does my knee still hurt?” Biology is slow.
Since you likely live abroad, we use technology to bridge the gap.
Regenerative medicine is not always “one and done.”
Complications are rare, but safety is paramount. Contact us immediately via the 24/7 International Line if:
You invested in your body. Protect the investment.
Sedation: We recommend waiting 24–48 hours before a long-haul flight to reduce the risk of DVT (blood clots) and allow any immediate swelling to subside.
Alcohol suppresses bone marrow function and dehydrates the body. We strongly recommend avoiding alcohol for 1 week before and 2 weeks after the procedure to give the cells the best chance of survival.
Biological therapy has a “non-responder” rate (approx. 10–15%). If you see no improvement by Month 6, we re-evaluate.
Cryopreservation (Banking) is a great “insurance policy.” While we have your fat in the lab, we can store the extra cells for up to 20 years. As you age, your stem cells get older too. Having “younger” cells (harvested today) stored for future use (10 years from now) is a smart biological investment.
No. Avoid deep tissue massage on the treated area (knee, hip, face) for 4 weeks. You want the cells to settle and attach to the scaffold, not be pushed around by mechanical pressure.

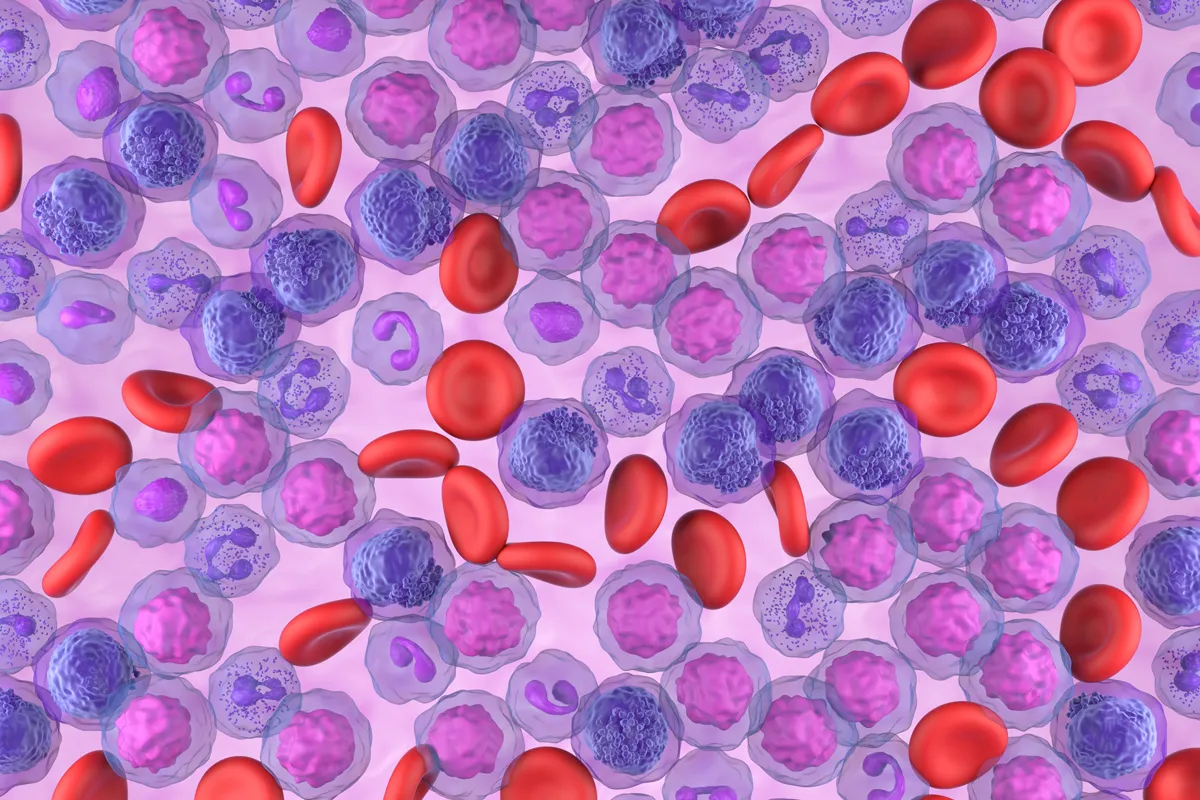
Acute Myeloid Leukemia (AML) is a serious blood cancer that needs quick and strong treatment. Chemotherapy is key in AML treatment. The number of rounds
Treating aplastic anemia during pregnancy is a big challenge. It needs careful balance to keep the mother and baby safe. Aplastic anemia is a rare

The opposite of an autologous transplant is an allogeneic transplant. This type uses stem cells or bone marrow from a donor, not the patient’s own.

The bone marrow transplant survival rate by age changes a lot. It’s very important to know who can’t get this treatment. Knowing the age limit



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)