Last Updated on October 20, 2025 by
Hepatoblastoma is a rare liver cancer that mainly affects young kids. We aim to give top-notch healthcare and support to patients worldwide.
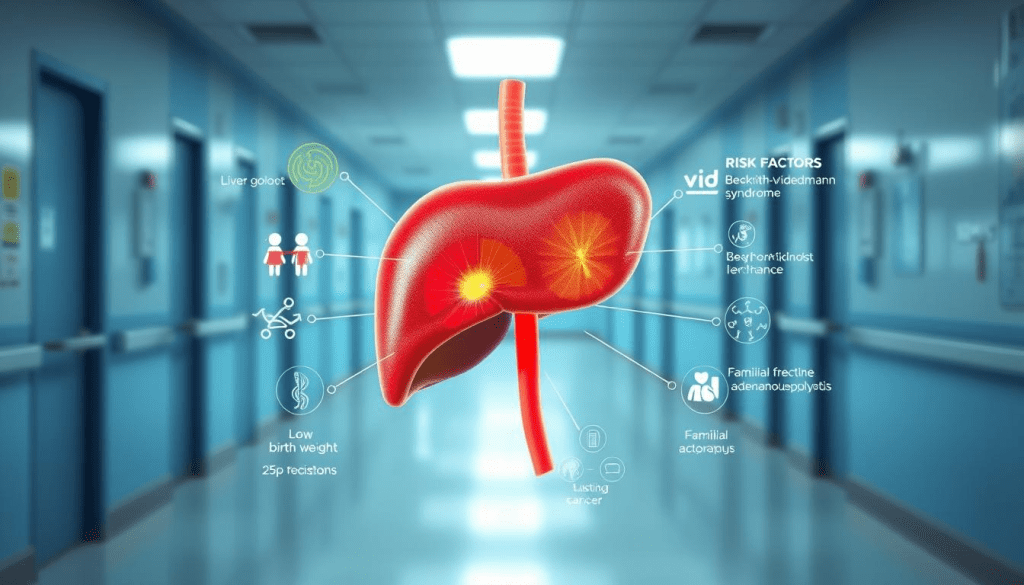
Knowing the risk factors is key for catching it early and treating it well. This rare cancer strikes about 1.5 cases per million kids each year. Most cases are found in kids under 4, with half diagnosed in their first year.
We focus on spotting risk factors at our place. Kids born very light are at a higher risk. This shows why we need to watch them closely.
Key Takeaways
- Liver cancer in children is extremely rare, with hepatoblastoma being the most common type.
- The majority of hepatoblastoma cases are diagnosed in children under the age of 4.
- Very low birth weight is a significant risk factor for hepatoblastoma.
- Early detection is critical for improving liver cancer survival rates.
- Understanding risk factors is essential for effective treatment and care.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
Hepatoblastoma is a rare liver cancer that mainly affects young kids. It’s a serious concern for families and doctors. This cancer needs special care.
This liver cancer is very rare and needs quick diagnosis and treatment. Getting this diagnosis can be tough. We’re here to help and support you every step of the way.

Liver tumors like hepatoblastoma are rare in kids. They make up a small part of all childhood cancers. But, it’s very important to have a team of experts for these cases. Our team is ready to give your child the best care.
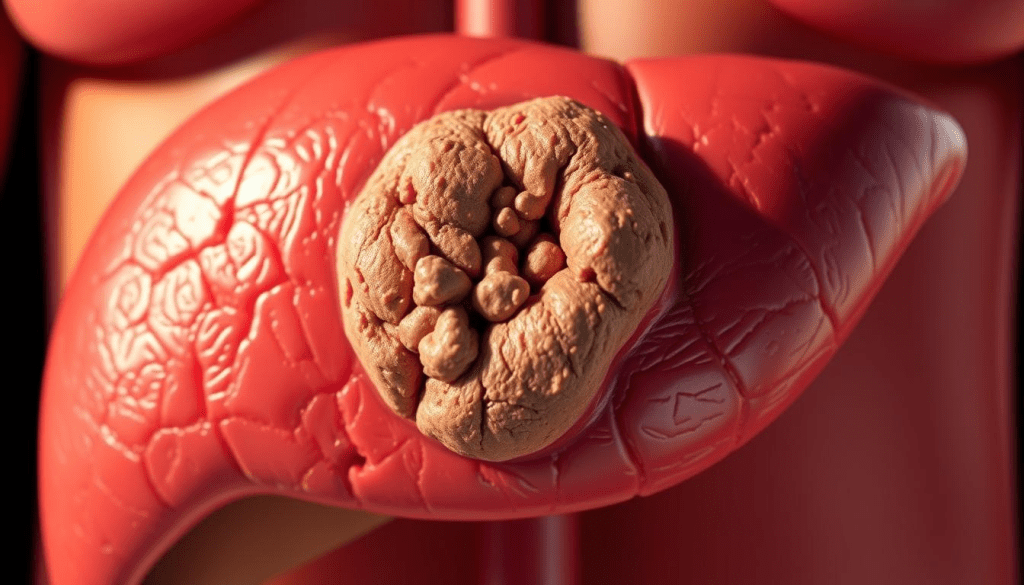
Hepatoblastoma can look different, but doctors find it with scans and biopsies. Knowing what it looks like helps doctors plan the best treatment. We make sure families are part of every decision.
Key Facts About Hepatoblastoma:
- Rare form of liver cancer in children
- Typically diagnosed in children under the age of 3
- Requires specialized care and treatment
- Prognosis improves with early detection and intervention
Let’s look at some important stats about hepatoblastoma:
| Age Group | Incidence Rate | Survival Rate with Treatment |
| 0-3 years | 1 in 100,000 | 80% |
| 4-6 years | 0.5 in 100,000 | 70% |
| 7+ years | Rare | Varies |
Understanding hepatoblastoma helps us improve care for kids with this rare cancer. We’re here to offer caring and complete care. We support families every step of the way.
Age as a Primary Risk Factor for Hepatoblastoma
Hepatoblastoma is a rare liver cancer that mainly hits young kids. Most cases are found before a child turns 4. Knowing this is key for parents and doctors to spot it early.
Hepatoblastoma often shows up as a mass on the liver or lump on liver in very young kids. Finding it early is very important. It can really change how well a child can be treated.
Predominance in Children Under 4 Years
About 95% of hepatoblastoma cases happen in kids under 4. This makes it very important for parents and caregivers to watch for signs. A big belly could be a sign of a tumor growing.
Let’s look at some data to understand more about hepatoblastoma and its risk factors:
| Age Group | Percentage of Hepatoblastoma Cases | Common Symptoms |
| 0-1 year | 50% | Abdominal swelling, loss of appetite |
| 1-2 years | 30% | Visible mass on the liver, jaundice |
| 2-4 years | 15% | Weight loss, fatigue, abdominal pain |
The table shows most cases are found in the first two years. This highlights the need for constant monitoring during this time.
It’s vital to have regular check-ups for young kids, even more so for those at risk. Spotting hepatoblastoma early can greatly improve treatment chances. So, parents and doctors need to watch for any signs of a mass on the liver or other symptoms.
Birth Weight and Prematurity Connections
Research shows that very low birth weight kids face a higher risk of getting hepatoblastoma. This is why it’s key to watch the health of premature and low birth weight babies closely.
Premature birth can lead to many health problems, including a higher chance of getting cancer. The liver is a vital organ that’s extra vulnerable in premature babies.
Premature Birth and Associated Complications
Premature birth can cause a lot of health issues, like breathing problems and a higher risk of infections. Also, premature babies often have organs that aren’t fully developed. This can impact their health and growth.
Our studies show that kids born too early or with very low birth weight are more likely to get a tumor in the liver. This shows we need to keep a close eye on them and find problems early.
The link between prematurity, low birth weight, and liver tumor risk comes from genetics and the environment.
| Birth Weight Category | Relative Risk of Hepatoblastoma | Associated Complications |
| Very Low Birth Weight (<1500g) | Higher | Respiratory issues, infections |
| Low Birth Weight (1500g-2500g) | Moderate | Developmental delays, health vulnerabilities |
| Normal Birth Weight (>2500g) | Lower | Fewer complications |
It’s important to understand these links to create better screening and watch plans for high-risk groups. This can help improve the lives of kids at risk of hepatoblastoma.
Genetic Predispositions and Hereditary Syndromes
Hepatoblastoma is linked to genetic factors and certain hereditary syndromes. It’s key to grasp these genetic predispositions. This helps us offer the best care for children at risk.
Familial Adenomatous Polyposis (FAP)
Familial Adenomatous Polyposis (FAP) causes many polyps in the colon. Kids with FAP face a higher risk of getting hepatoblastoma. We stress the importance of early screening and watching for lesions on the liver in these kids.
Beckwith-Wiedemann Syndrome
Beckwith-Wiedemann Syndrome raises the risk of tumors, including hepatoblastoma, in children. It’s marked by overgrowth and a higher chance of childhood tumors. We keep a close eye on families with this syndrome for any hepatic lesions.
Other Genetic Conditions Associated with Hepatoblastoma
Conditions like Glycogen Storage Disease and certain chromosomal issues also up the risk of hepatoblastoma. We look at these factors when figuring out a child’s risk for tumors on the liver.
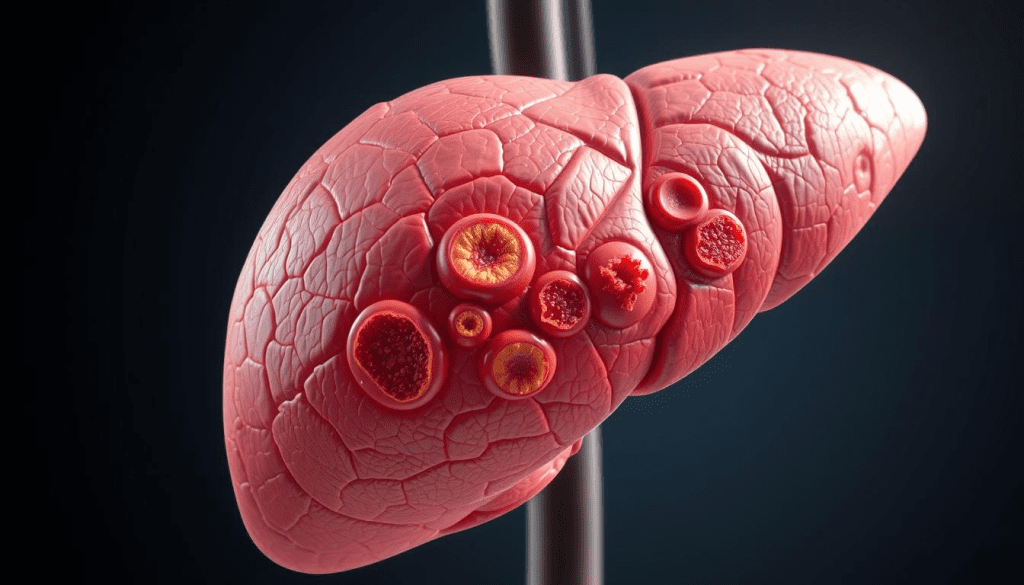
Differentiating Hepatoblastoma from Other Hepatic Lesions
Getting the right diagnosis is vital for treating liver tumors. We must tell apart hepatoblastoma from other masses on the liver using imaging and biopsies. Our advanced diagnostic methods help us accurately define the lesion on the liver. This guides the right treatment.
Screening and Surveillance for High-Risk Groups
We now have advanced screening for kids at high risk of hepatoblastoma. Our center uses detailed screening to spot at-risk kids early. This helps improve their hepatoblastoma prognosis and treatment results.
Some kids are at higher risk due to genetics or early birth. For them, regular checks are key. We use ultrasound and MRI to keep an eye on their liver. This way, we catch problems early, when they’re easier to treat.
The liver cancer survival rate by age is better if caught early. Kids under 4, who are most affected, have a better chance if found early. Our goal is to find hepatoblastoma early, boosting survival rates.
Screening might seem scary, but our team is here to help. We offer caring support during screenings. By watching high-risk kids closely, we can act fast if cancer shows up, giving them the best shot at recovery.
We’re committed to top-notch screening as part of our mission. We aim to provide world-class care and support to families from around the world. With the latest tech and caring support, we aim to help kids and families dealing with hepatoblastoma.
Diagnostic Approaches for Suspected Hepatoblastoma
When a liver tumor is suspected, our team uses many ways to confirm it’s hepatoblastoma. Imaging is key in spotting liver tumors and masses.
We use top-notch imaging like ultrasound, CT scans, and MRI to see the liver. These tests help us find the tumor’s size, location, and how it affects nearby tissues.
Biopsy procedures are also used to confirm the diagnosis. Our pathology team works with radiologists to study tissue samples. This helps us give an accurate diagnosis.
By combining imaging and biopsy results, we create a treatment plan for each patient. Our team is committed to giving the best care for children with hepatoblastoma. We aim for the best outcomes.
FAQ
What is hepatoblastoma?
Hepatoblastoma is a rare liver cancer found mainly in young children. It often affects kids under 4 years old.
What are the risk factors for developing hepatoblastoma?
Risk factors include being under 4, very low birth weight, and premature birth. Certain genetic conditions like Familial Adenomatous Polyposis (FAP) and Beckwith-Wiedemann Syndrome also increase the risk
How is hepatoblastoma diagnosed?
Doctors use imaging and biopsies to confirm liver tumors. This helps diagnose hepatoblastoma.
What is the significance of birth weight in hepatoblastoma?
Babies with very low birth weight face a higher risk of getting hepatoblastoma.
Can hepatoblastoma be detected early?
Yes, early detection is possible through screening. This is key for improving treatment results, mainly in high-risk groups
What is the difference between hepatoblastoma and other liver lesions?
Hepatoblastoma is a specific cancerous liver tumor. It’s different from other liver growths, needing accurate diagnosis.
Are there genetic conditions associated with an increased risk of hepatoblastoma?
Yes, conditions like FAP and Beckwith-Wiedemann Syndrome raise the risk of hepatoblastoma.
What are the treatment options for hepatoblastoma?
Treatment includes surgery, chemotherapy, and sometimes liver resection or transplant. The choice depends on the tumor’s size and location.
What is the prognosis for children diagnosed with hepatoblastoma?
Prognosis depends on the tumor’s stage, treatment response, and other factors. Early detection and treatment can lead to good outcomes for many children.
How does age affect the risk and prognosis of hepatoblastoma?
Age is a big risk factor, with most cases in kids under 4. Age also influences prognosis, along with other factors.
References
Centers for Disease Control and Prevention. (2024). Facts about birth defects. https://www.cdc.gov/ncbddd/birthdefects/facts.html
Hockenberry, M. J., Wilson, D., & Rodgers, C. C. (2019). Wong’s nursing care of infants and children (11th ed.). Mosby. https://www.elsevier.com/books/wongs-nursing-care-of-infants-and-children/hockenberry/978-0-323-54939-5
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). (2023). Patient information on hernia repair. https://www.sages.org/publications/patient-information/patient-information-for-hernia-repair-from-sages/





