Last Updated on December 2, 2025 by Bilal Hasdemir

Every year, over 50,000 stem cell transplants are done worldwide. They give hope to those with certain cancers and other serious diseases. Explaining the BMT steps and discussing What are the odds of bone marrow transplant process
Starting a stem cell transplant journey can feel scary. As a top healthcare provider, we’re here to help you through it all.
A stem cell transplant, or bone marrow transplant, is a detailed medical process. It replaces bad stem cells with good ones. Our team is ready to offer full care and support during the transplant process.
Key Takeaways
- A stem cell transplant is a life-saving treatment for certain cancers and diseases.
- The transplant process involves replacing damaged stem cells with healthy ones.
- Our healthcare team provides complete care and support throughout the journey.
- Understanding the transplant process can help ease worries and fears.
- We are committed to guiding you every step of the way.
What is a Bone Marrow Transplant?

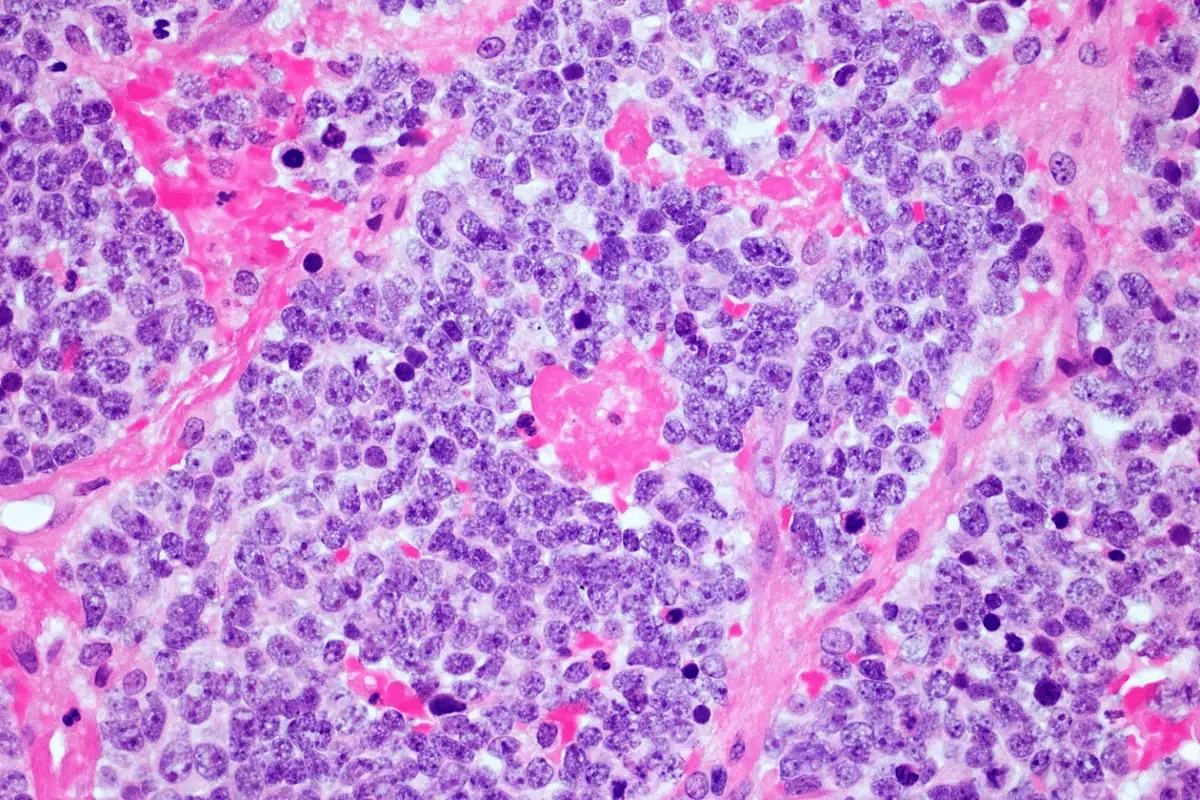
A bone marrow transplant is a complex medical procedure. It replaces damaged or diseased bone marrow with healthy marrow. This treatment is used for patients with cancers and blood disorders. We will look at what it is, why it’s done, its types, and why it’s necessary.
Definition and Purpose
A bone marrow transplant, also known as a stem cell transplant, uses stem cells to help the body make healthy blood cells. It aims to treat diseases by replacing the patient’s bone marrow with healthy marrow. This can come from the patient themselves or a donor.
The transplant starts with conditioning. The patient gets treatment to destroy their bone marrow. Then, stem cells are infused. These cells migrate to the bone marrow and start producing new blood cells.
Types of Transplants
There are several types of bone marrow transplants:
- Autologous transplants: Using the patient’s own stem cells.
- Allogeneic transplants: Using stem cells from a donor.
- Syngeneic transplants: Using stem cells from an identical twin.
Each type has its own uses and benefits. For example, autologous transplants are often used for certain lymphomas and myelomas. Allogeneic transplants are used for a wider range of conditions, including leukemia.
Who Needs a Transplant?
Bone marrow transplants are considered for patients with:
| Condition | Description |
| Leukemia | A cancer of the blood or bone marrow. |
| Lymphoma | A cancer of the immune system. |
| Myeloma | A cancer of plasma cells in the bone marrow. |
| Aplastic Anemia | A condition where the bone marrow fails to produce blood cells. |
These conditions can greatly benefit from a bone marrow transplant. It can potentially cure the disease or give a longer disease-free survival.
The Preparation Phase of Transplant
Before a bone marrow transplant, patients go through a detailed evaluation. This step is key to see if they can get the transplant. It also gets them ready for the procedure.
Medical Evaluation Process
We start with a detailed medical check-up. This helps us see if the patient is healthy enough for the transplant. Our team of doctors and nurses do many tests and talks.
We look at the patient’s health history and current status. We also do tests to check the heart, lungs, and liver. This is to make sure everything is okay for the transplant.
| Test Type | Purpose |
| Cardiac Evaluation | Check if the heart can handle the transplant. |
| Pulmonary Function Tests | Make sure the lungs are ready for the transplant. |
| Liver Function Tests | Check the liver’s health for after the transplant. |
Necessary Tests and Procedures
During preparation, we do many tests and procedures. These help make sure the patient is ready for the transplant. We do blood tests, imaging, and other checks.
- Blood tests to check blood chemistry and count
- Imaging studies like X-rays and CT scans to check organs
- Dental check to prevent infections
We explain each test and procedure to the patient. This helps them understand and get ready.
“The preparation phase is a critical period that requires careful planning and coordination. It’s a time when patients must be thoroughly evaluated and prepared for the transplant process.”
Expert in Bone Marrow Transplantation
Finding a Donor
Finding the right donor is very important. We use national and international registries to find donors. We match the donor and recipient through HLA typing.
After finding a donor, we do more tests to confirm the match. This is key for a successful transplant.
We keep in touch with the patient during this time. We offer support and answer their questions. Our goal is to make sure the patient is ready, both physically and emotionally.
The Stem Cell Collection Process
Learning about the stem cell collection process can ease worries for those getting a bone marrow transplant. We’ll explain where stem cells come from, how they’re collected, and what to do to prepare.
Sources of Stem Cells
Stem cells can be found in different places. The main sources are bone marrow, blood, and umbilical cord blood. Each has its own way of being collected and benefits.
Collection Methods
The way stem cells are collected depends on where they come from.
Bone Marrow Harvesting
Harvesting bone marrow means taking stem cells straight from the bone marrow. This is done under general anesthesia to make it less painful.
Peripheral Blood Stem Cell Collection
For peripheral blood, stem cells are first made to move into the blood. Then, a process called apheresis separates them from other blood parts.
Umbilical Cord Blood Collection
Umbilical cord blood collection gets stem cells from the umbilical cord and placenta after birth. It’s a gentle method and a good alternative.
Preparing for Collection
Getting ready for stem cell collection includes a medical check-up and instructions from your healthcare team. They’ll tell you how to get ready for a smooth process.
The collected stem cells will be given through your central venous catheter, like a blood transfusion. Knowing this helps patients understand how the stem cells will be given after collection.
| Source | Collection Method | Advantages |
| Bone Marrow | Harvesting under anesthesia | Rich source of stem cells |
| Peripheral Blood | Apheresis after stimulation | Less invasive than bone marrow harvesting |
| Umbilical Cord Blood | Collection after childbirth | Non-invasive, readily available |
Pre-Transplant Conditioning
Pre-transplant conditioning is a key step before a bone marrow transplant. It gets the body ready to accept new stem cells. This is vital for the transplant’s success.
What is Conditioning?
Conditioning in bone marrow transplantation means treatments before the transplant. Its main goals are to kill any cancer cells left, weaken the immune system, and clear space in the bone marrow for new stem cells.
“The conditioning regimen is a critical component of the transplant process, as it helps to eradicate malignant cells and prevent graft rejection.”
Types of Conditioning Regimens
There are various conditioning regimens based on the patient’s health and the transplant type. They mainly fall into two categories: myeloablative and non-myeloablative conditioning.
- Myeloablative conditioning uses strong chemotherapy and/or radiation to wipe out the bone marrow. It’s more intense and suited for some cancer patients.
- Non-myeloablative conditioning, by contrast, employs lower doses of chemotherapy and/or radiation. It’s gentler and better for older patients or those with health problems.
| Type of Conditioning | Description | Typical Use |
| Myeloablative | High doses of chemotherapy and/or radiation to eradicate bone marrow | Patients with certain cancers |
| Non-myeloablative | Lower doses of chemotherapy and/or radiation | Older patients or those with other health issues |
Importance of Conditioning
The conditioning regimen is essential for a successful bone marrow transplant. It kills cancer cells and weakens the immune system. This reduces the chance of the body rejecting the transplant. It also prepares the bone marrow for the new stem cells to grow and produce healthy blood cells.
In summary, pre-transplant conditioning is a critical process for bone marrow transplants. Knowing about the different conditioning regimens and their role helps patients understand their treatment better.
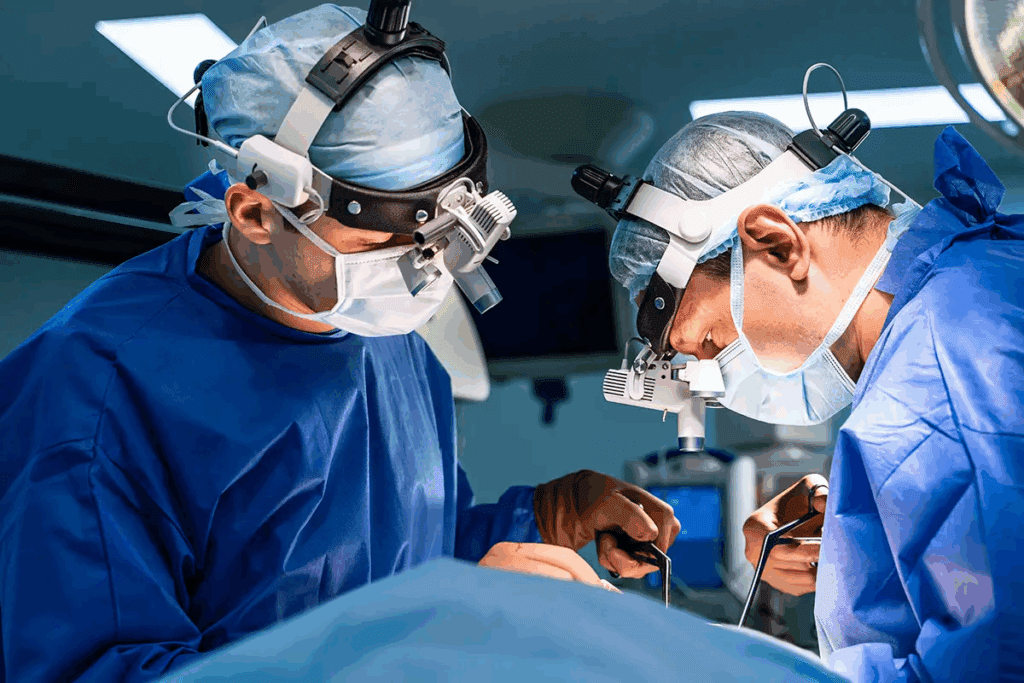
The Transplant Day: What to Expect
The day of the bone marrow transplant is a big moment. It brings hope and excitement for patients and their families.
On this day, called Day 0, patients get their stem cell infusion. This is like a blood transfusion. Stem cell infusion is a simple process. It involves putting the stem cells into the patient’s blood through a special line.
The Procedure Explained
The stem cell infusion takes a few hours. During this time, the patient is watched closely for any bad reactions. Our medical team is skilled in these procedures. They make sure the patient is safe and comfortable.
Monitoring During the Transplant
While the infusion happens, patients are checked for important signs and side effects. This close watch lets our team act fast if needed. It helps make sure the transplant goes well.
- Vital sign monitoring
- Observation for infusion reactions
- Supportive care as needed
Post-Transplant Care
After the transplant, patients go to a recovery area. They are watched for any quick problems. Post-transplant care is key for recovery. A team of healthcare workers helps with care, side effects, and watching for GVHD.
The time after the transplant can be tough. It’s hard both physically and emotionally. Our team works hard to give full care. This includes food support, pain help, and emotional support. We aim to help patients get through this important time.
Managing Side Effects After the Transplant
Managing side effects is key after a bone marrow transplant. It’s important to know the possible side effects and how to handle them. This knowledge is vital for a smooth recovery.
Common Side Effects
Patients may face many side effects after a transplant. These include full-body flushing, itching, and hives. They might also have trouble breathing, chest pain, and stomach cramps.
Nausea, vomiting, and feeling lightheaded are also common. Every person reacts differently, so knowing these side effects is the first step.
Mitigating Discomfort
To ease discomfort, we suggest a few strategies. Following your doctor’s medication plan is important. Eating well, drinking plenty of water, and resting enough also help.
Meditation and deep breathing can reduce stress. These practices improve overall well-being.
Importance of Communication
Talking to your healthcare team is essential. We urge patients to share any side effects, no matter how small. This way, doctors can adjust your care plan as needed.
Working together, patients get the support they need. This teamwork helps them through the recovery process.
Understanding Smell Changes Post-Transplant
One of the lesser-known side effects of bone marrow transplantation is a change in a patient’s sense of smell. Some patients notice a big change in their sense of smell after the procedure.
Reasons Behind Smell Alterations
The exact reasons for smell changes after a transplant are not fully understood. But several factors are believed to play a role. The conditioning regimen, which includes chemotherapy and/or radiation, can damage the olfactory epithelium. This leads to changes in smell perception.
Also, certain medications used during and after the transplant can affect the sense of smell. Some patients report a strong taste or smell during the infusion of stem cells. This is often described as similar to garlic or creamed corn. This unusual sensation is usually temporary and goes away once the infusion is complete.
Duration and Variability of Smell Changes
The time it takes for smell changes to go away can vary a lot. Some people may get back to their normal sense of smell within a few weeks or months after the transplant. But others may have persistent changes that last longer.
Several factors can influence how long smell changes last. These include the type of conditioning regimen used, the presence of graft-versus-host disease (GVHD), and individual differences in recovery and healing.
| Factor | Influence on Smell Changes |
| Conditioning Regimen | Chemotherapy and/or radiation can damage olfactory epithelium. |
| Medications | Certain drugs used during and after transplant can affect smell. |
| GVHD Presence | Graft-versus-host disease can impact recovery and healing. |
Coping with Smell Changes
Dealing with smell changes can be tough, but there are ways to cope. We suggest trying different flavors and aromas to find what you like best. Using herbs and spices can make food taste better and be more enjoyable.
Good oral hygiene is also important. Avoiding strong smells can help too. Keeping a food diary can help you understand your preferences and make meal times easier.
By understanding why smell changes happen and using effective coping strategies, patients can better manage this part of their recovery after a transplant.
Nutrition and Diet Post-Transplant
Eating well is key to getting better after a bone marrow transplant. Everyone’s needs are different, but a good diet helps you get strong again.
Importance of Nutrition
Good food is very important after a transplant. It helps your body heal, boosts your immune system, and helps with side effects. Eating a balanced diet is a must.
Nutrition is vital for:
- Supporting the immune system
- Aiding in the recovery of cells and tissues
- Managing side effects and complications
- Enhancing overall well-being and energy levels
Recommended Foods
After a transplant, eat foods that are full of nutrients and easy to digest. Good choices include:
- Fresh fruits and vegetables
- Lean proteins like chicken, fish, and eggs
- Whole grains such as brown rice, quinoa, and whole-wheat bread
- Low-fat dairy and foods rich in calcium
Adding foods high in antioxidants, like berries and leafy greens, can also help.
Foods to Avoid
Some foods can be risky or mess with your meds. It’s best to avoid them while you’re recovering. Foods to limit or avoid include:
- Raw or undercooked meats, eggs, and seafood
- Unpasteurized dairy products and juices
- Raw sprouts and unwashed fruits and vegetables
- High-risk foods that may contain harmful bacteria
Stick to food safety tips and talk to your healthcare team about what’s best for you.
By eating well, you can help your body heal and feel better after a bone marrow transplant.
Emotional and Psychological Considerations
Going through a bone marrow transplant is tough, both physically and emotionally. It’s a journey that needs a lot of emotional strength and support.
The transplant experience can touch patients in many ways. That’s why it’s key to focus on the emotional and psychological sides of care. Mental health support is a big part of getting better.
Mental Health Support
Patients going through a bone marrow transplant need a lot of mental health help. This help can be counseling, therapy, or joining support groups. We urge patients to look for these resources to deal with the emotional ups and downs of the transplant.
Some important parts of mental health support include:
- Access to professional counseling
- Support groups for patients and families
- Mindfulness and relaxation techniques
Coping with Anxiety and Stress
Handling anxiety and stress is a big part of the transplant journey. Things like meditation, deep breathing, and yoga can help. We suggest patients try these to see what works for them.
Talking openly with healthcare providers about anxiety and stress is also important. It helps get the right support and advice.
Resources for Patients
There are many resources to help patients emotionally and psychologically during and after the transplant. These include:
- Mental health professionals specializing in transplant care
- Online resources and forums
- Local support groups
We encourage patients to use these resources to improve their emotional and psychological health during this tough time.
The Recovery Process
After a bone marrow transplant, patients face a tough but rewarding recovery. It’s a gradual process, and knowing what to expect is key.
Timeline for Recovery
The bone marrow transplant recovery timeline varies a lot. It can take months to a year or more to feel fully recovered. The first few weeks are very risky, with high chances of infections and other problems.
As patients get better, they start to see improvements. But how fast they recover depends on several things. These include the type of transplant, the patient’s health, and how well the treatment worked.
Follow-Up Care and Check-Ups
Follow-up care after transplant is vital. It helps keep an eye on the patient’s health and catches any issues early. Regular visits with the healthcare team are important for this.
At these visits, patients have tests like blood work and bone marrow biopsies. These check how well the new bone marrow is working.
Living Life After Transplant
Living after transplant means ongoing care and changes in lifestyle. Patients should eat well, exercise, and avoid infections.
It’s also important to stay in touch with the healthcare team and get support when needed. Many find support groups helpful for sharing experiences and learning from others.
By understanding the recovery process and following recommended care, patients can have a better outcome. This improves their quality of life after the transplant.
Long-Term Outlook and Survival Rates
For many patients, a bone marrow transplant offers a chance at a cure or a longer disease-free period. Understanding the long-term outlook after such a procedure is essential for managing expectations and making informed decisions about their care.
Factors Influencing Survival
Several factors can influence the survival rates of patients after a bone marrow transplant. These include the patient’s overall health before the transplant, the type of transplant performed (autologous or allogeneic), the underlying condition being treated, and how well the patient responds to the transplant.
Age and health status are significant factors, as older patients or those with other health issues may face higher risks. The match quality between donor and recipient also plays a critical role in the success of the transplant.
Quality of Life Post-Transplant
The quality of life after a bone marrow transplant can vary significantly among patients. While some may experience a full recovery and return to their normal activities, others may face ongoing challenges.
Common issues include managing the risk of infections, dealing with graft-versus-host disease (GVHD) in allogeneic transplants, and coping with the emotional and psychological impact of the treatment. Yet, with proper care and support, many patients are able to lead active and fulfilling lives.
Life After Treatment
Life after a bone marrow transplant involves a period of recovery and adjustment. Follow-up care is critical to monitor the patient’s health and address any complications early.
Patients are advised to maintain a healthy lifestyle, including a balanced diet, regular exercise, and avoiding infections. They are also encouraged to stay in touch with their healthcare team for ongoing support and guidance.
Resources and Support Groups
After a bone marrow transplant, patients need ongoing support. This helps them manage their recovery and adjust to life after the transplant. Caregivers and friends and family play a big role in supporting them at home.
Finding Support Networks
Support groups for transplant patients offer a sense of community. They connect patients with others who face similar challenges. We help patients find these groups, which are a valuable resource during their recovery.
Educational Resources
Educational resources are key for transplant patients. They help patients understand their condition and the transplant process. We provide access to reliable information and resources to support their journey.
Professional Organizations and Assistance
Professional organizations and assistance programs offer extra support to bone marrow transplant patients. These resources help patients navigate their recovery and beyond. They provide the tools patients need to thrive.
FAQ
What is a bone marrow transplant?
A bone marrow transplant replaces a patient’s bone marrow with healthy stem cells. These can come from the patient or a donor.
What does BMT stand for in medical terms?
BMT stands for Bone Marrow Transplant.
How long does a bone marrow transplant take?
A bone marrow transplant can take weeks to months. It includes preparation, the transplant, and recovery.
What are the different types of bone marrow transplants?
There are several types. Autologous uses the patient’s own stem cells. Allogeneic uses a donor’s stem cells. Syngeneic uses stem cells from an identical twin.
Who needs a bone marrow transplant?
Patients with certain cancers or diseases may need a transplant. This includes leukemia, lymphoma, aplastic anemia, or sickle cell disease.
What is the process of bone marrow donation?
The donation process starts with registration and blood tests. If selected, the donor undergoes a procedure to extract bone marrow from their pelvic bone under anesthesia.
How long does it take to donate bone marrow?
The donation itself takes one to two hours. But the whole process, including preparation and recovery, can take several hours or days.
Is a bone marrow transplant painful?
The transplant itself is not painful, as it’s done under anesthesia. But patients might feel discomfort or pain during recovery.
What are the common side effects of a bone marrow transplant?
Side effects include fatigue, nausea, vomiting, diarrhea, and a higher risk of infections.
How can I manage side effects after a bone marrow transplant?
Managing side effects involves medication, lifestyle changes, and monitoring by healthcare providers. This helps reduce discomfort and prevent complications.
What is the importance of nutrition after a bone marrow transplant?
Nutrition is key in recovery. A healthy diet supports the body, manages side effects, and aids in healing.
What foods are recommended after a bone marrow transplant?
Recommended foods include fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoid foods that may increase infection risk or interact with medications.
How long does it take to recover from a bone marrow transplant?
Recovery time varies but can take months to a year or more. It takes time for the immune system to recover and for patients to regain strength and quality of life.
What is the long-term outlook after a bone marrow transplant?
The long-term outlook depends on several factors. These include the condition being treated, the type of transplant, and the patient’s health. Many patients achieve long-term survival and improved quality of life.
Where can I find support groups and resources after a bone marrow transplant?
Support groups and resources are available through organizations, online forums, and healthcare providers. They offer emotional support, educational resources, and practical assistance.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra052638