Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, thousands of children worldwide die from sickle cell disease. This condition greatly affects their life quality and how long they live. In sub-Saharan Africa, the disease is even more common, making it a big health issue.Analyzing the current statistics and major causes contributing to Pediatric sickle cell mortality rates and risks.
We know that understanding how the disease progresses is key. It helps us tackle the advanced medical challenges these kids face. By knowing the risks and using specialized pediatric assessment strategies, we can lower the death rates from this disease.
Key Takeaways
- Understanding the disease’s progression is vital in managing sickle cell disease.
- Advanced medical challenges need specialized pediatric assessment and care.
- Lowering death rates in children with sickle cell disease is a global health priority.
- Early intervention and complete care can greatly improve life quality for these kids.
- Specialized care strategies are key in meeting the unique needs of these children.
Understanding Sickle Cell Disease and Its Impact

Sickle Cell Disease is a big public health problem. We need to understand and manage it well. We will look at what it is, how common it is in kids, and why it happens.
Definition of Sickle Cell Disease
Sickle Cell Disease comes from a change in the HBB gene. This change makes red blood cells sickle under certain conditions. This leads to many health problems.
Prevalence Among Children
SCD mainly hits kids, mostly those of African descent. But it also affects other ethnic groups. It’s a big worry in pediatric hematology because it harms kids’ lives and can be deadly.
Genetic Causes and Inheritance
The disease is caused by getting two bad hemoglobin genes, one from each parent. Genetic counseling is key for families with SCD history. It helps them know the risks and how to manage them.
Knowing the genetic reasons helps find and treat the disease early. This improves the lives of kids with SCD.
The Role of Viruses in Sickle Cell Disease

Viral infections are a big worry for kids with SCD. They can cause acute chest syndrome and other serious problems. We must know which viruses affect these kids and how they make the disease worse.
Common Viral Infections in Affected Children
Children with Sickle Cell Disease get sick more easily because their immune systems are weak. Common viruses include influenza, respiratory syncytial virus (RSV), and parvovirus B19. These viruses can cause serious issues like advanced respiratory complications and severe infection complications. This means they need comprehensive health monitoring.
- Influenza can cause severe respiratory illness.
- RSV is associated with severe bronchiolitis and pneumonia.
- Parvovirus B19 can trigger aplastic crises.
Association Between Viruses and Disease Severity
There’s a clear link between viral infections and how bad Sickle Cell Disease can get. Viral infections can lead to acute chest syndrome, a major cause of sickness and death in SCD patients. Quickly finding and treating viral infections is key to avoiding serious problems. We stress the need for thorough health checks to spot and treat viruses fast.
Some important things to remember:
- Viral infections can make SCD symptoms worse.
- Advanced respiratory complications can come from viral infections.
- Severe infection complications need quick medical help.
Key Complications of Sickle Cell Disease
Sickle Cell Disease can lead to serious problems, like acute chest syndrome, sepsis, and stroke. These issues are very dangerous for kids. They can make life much harder and even lead to death.
Acute Chest Syndrome
Acute Chest Syndrome (ACS) is a big problem for people with Sickle Cell Disease. It shows up as a new spot on a chest X-ray, often with fever or pain. We know how serious ACS is and how fast we need to act.
To treat ACS, we use oxygen, manage pain, and give antibiotics. Sometimes, we need to give blood transfusions to prevent more harm.
Sepsis and Infections
Kids with Sickle Cell Disease get sick easily because their immune system is weak. Sepsis, a very dangerous condition, can happen from these infections. We stress the importance of getting vaccines and taking antibiotics to prevent infections.
Regular doctor visits and keeping clean are also key. These steps help a lot in avoiding sepsis and other infections in kids with SCD.
Stroke Risk in Pediatric Patients
Children with Sickle Cell Disease are at high risk for stroke. This happens when sickled red blood cells block blood vessels. We work hard to find out who is at risk and monitor them closely.
For those at high risk, we use blood transfusions to help prevent stroke. Our team works with families to create care plans that meet each child’s needs.
It’s important to know about the main problems caused by Sickle Cell Disease to give good care. Below is a table that lists the main complications and how to manage them.
| Complication | Description | Management Strategy |
| Acute Chest Syndrome | New pulmonary infiltrate on chest radiograph, often with fever or respiratory symptoms | Oxygen therapy, pain management, broad-spectrum antibiotics, possible blood transfusions |
| Sepsis and Infections | Life-threatening condition arising from infections, to which SCD patients are highly susceptible | Vaccinations, prophylactic antibiotics, regular health check-ups, good hygiene practices |
| Stroke | Obstruction of blood vessels by sickled red blood cells | Regular screening, blood transfusions for high-risk patients, personalized care plans |
Pediatric Sickle Cell Mortality Statistics
Recent advances in medical care have led to a decline in pediatric sickle cell mortality rates. We have seen big improvements in managing sickle cell disease (SCD) over the last decade. This is thanks to better strategies for preventing death and new ways to diagnose the disease.
The latest statistics show a big drop in death rates among kids with SCD. This shows how well tracking and managing the disease works.
Trends Over the Last Decade
Looking at the last decade, we see a steady drop in SCD deaths in kids. This is due to better healthcare access, more complete care plans, and early detection through advanced tests.
Places with strong disease tracking systems have seen lower death rates. This shows how key a good healthcare setup is in fighting SCD.
| Year | Mortality Rate (per 100,000) | Change from Previous Year |
| 2013 | 2.5 | – |
| 2018 | 1.8 | -28% |
| 2022 | 1.2 | -33% |
Comparison with Other Hemoglobinopathies
When we compare SCD mortality rates with other hemoglobinopathies, SCD is a big worry. But, SCD death rates are falling faster. This is thanks to focused efforts and complete care plans.
Our study shows the need to keep investing in preventing SCD deaths and improving diagnosis. By using these strategies, we can help kids with SCD have even better outcomes.
Risk Factors Affecting Pediatric Mortality
It’s important to know what risks lead to death in kids with Sickle Cell Disease (SCD). Many factors play a role in how likely a child is to die from SCD.
Socioeconomic Status
Socioeconomic status (SES) greatly affects health in kids with SCD. Families with less money struggle to get good healthcare. Financial problems make it hard to pay for treatments and hospital visits.
A study shows a link between SES and health in SCD patients.
| Socioeconomic Status | Hospitalization Rate | Mortality Rate |
| Low | High | Higher |
| Middle | Moderate | Lower |
| High | Low | Lowest |
Access to Healthcare
Getting good healthcare is key for managing SCD. Kids with SCD need regular check-ups and quick treatment for problems. Not having access to healthcare can make things worse.
“Access to care is a critical issue for children with Sickle Cell Disease. Ensuring that these children receive timely and appropriate medical interventions can significantly improve their outcomes.”
We need to focus on comprehensive patient support. This means medical care, but also help for the family’s mental and social health.
Comorbid Conditions
Having other health problems can raise the risk of death in kids with SCD. Issues like asthma, infections, and other chronic diseases make SCD harder to manage.
To lower death rates in SCD, we must tackle these risks. We need to improve money situations, get better healthcare access, and handle other health issues well.
Prevention Strategies for Viral Infections
For kids with SCD, stopping viral infections is key. We, as caregivers and doctors, must teach ways to keep them safe from infections. These infections can cause big problems.
Vaccinations and Immunizations
Vaccines are very important for kids with SCD. We suggest following the usual vaccine schedule. This includes extra shots like the pneumococcal conjugate vaccine (PCV) and the flu vaccine.
“Vaccination is one of the most effective ways to prevent infections in children with Sickle Cell Disease,” say pediatric hematologists. It’s vital for parents to know about the latest vaccines.
We help families understand why and when to get vaccines. We make sure the advice fits their child’s needs.
Regular Health Check-Ups
Regular health checks are key for kids with SCD. We check their health, look at their vaccine records, and give advice on managing their condition.
These visits are also a chance to teach families about viral infections. We teach them to know when to get help fast. This helps avoid serious problems.
Good Hygiene Practices
Good hygiene helps stop viral infections. We tell families to wash hands often, stay away from sick people, and keep things clean.
By doing these things, families can lower the chance of their kids getting sick. A parent said, “Simple habits like washing hands regularly have made a big difference in our child’s health.”
By using vaccines, regular health checks, and good hygiene, we can protect kids with SCD from viruses. Our aim is to give families the knowledge and tools to keep their kids safe and healthy.
Management of Sickle Cell Disease
Managing Sickle Cell Disease involves several strategies. These include pain management, blood transfusions, and hydroxyurea therapy. It’s key to improve patients’ lives and lower the risk of serious problems.
Pain Management Techniques
Pain management is a big part of SCD care. We use medicines, hydration, and rest to help. Sometimes, patients need to stay in the hospital for severe pain.
A leading expert says, “Pain is the main issue in sickle cell disease. We need a full plan to tackle it, using both medicines and other methods.”
“Pain management in SCD is not just about alleviating the physical discomfort; it’s also about addressing the emotional and psychological impact on the patient.”
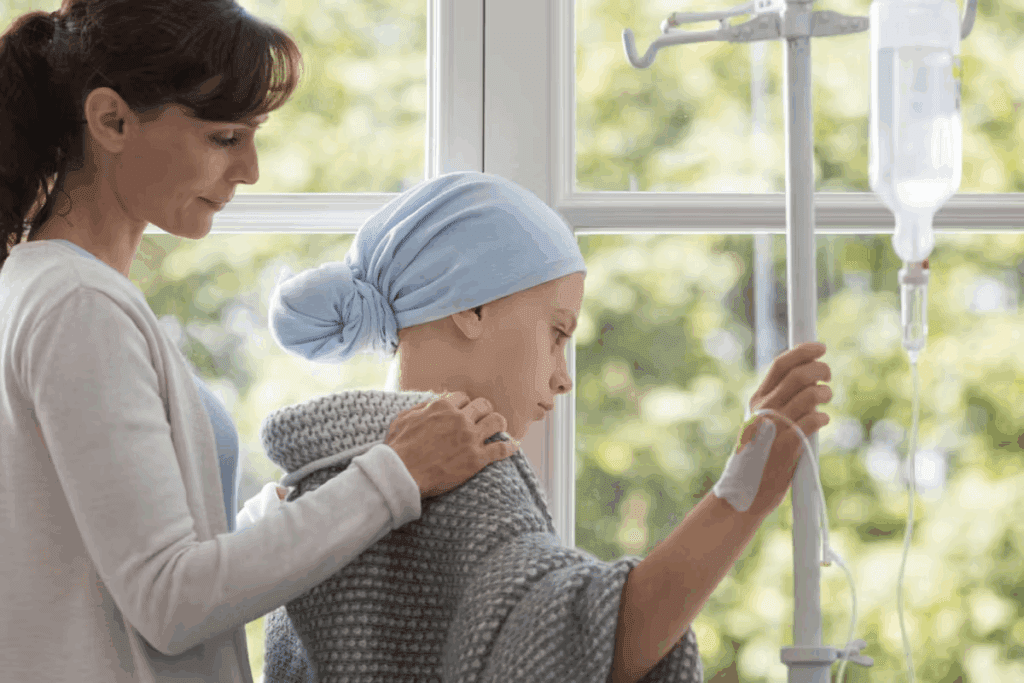
Blood Transfusions and Hydroxyurea
Blood transfusions help by lowering the risk of serious problems. They reduce the number of sickled red blood cells. Hydroxyurea can also help by making pain crises less frequent and possibly reducing the need for blood transfusions.
| Treatment | Purpose | Benefits |
| Blood Transfusions | Reduce sickling of red blood cells | Decreases risk of stroke and other complications |
| Hydroxyurea | Reduce frequency of pain crises | May reduce need for blood transfusions |
Comprehensive Care Approaches
Comprehensive care for SCD involves a team of experts. This includes hematologists, primary care doctors, nurses, and sometimes mental health professionals. We all work together to meet our patients’ complex needs.
Key components of this care include:
- Regular health check-ups
- Pain management
- Blood transfusions and hydroxyurea therapy
- Psychological support
By using a complete care approach, we can greatly improve patients’ lives. Our aim is to offer care that meets their physical, emotional, and social needs.
Research and Advances in Treatment
The treatment for Sickle Cell Disease is changing fast. This is thanks to new gene therapy and clinical trials. Now, we have more personalized and effective treatments for SCD patients.
Breakthroughs in Gene Therapy
Innovations in Clinical Trials
New clinical trials are key in improving SCD treatment. They test new medicines and therapies. One exciting area is targeted therapies that could lessen painful crises and other issues.
- Trials are looking into new gene editing methods.
- Researchers are exploring combination therapies for better results.
- Studies aim to enhance patient quality of life through better disease management.
Emerging Therapies on the Horizon
New therapies are on the way, bringing hope. These include novel pharmacological agents to lessen SCD symptoms. Also, innovative transplant techniques could cure the disease.
A recent report says, “The future of Sickle Cell Disease treatment is in personalized medicine. It will be tailored to each patient’s needs.”
We’re hopeful about SCD treatment’s future. Ongoing research and progress offer new hope to patients and their families.
Advocacy and Support for Affected Families
Families dealing with sickle cell disease need a lot of help. They face many challenges. Advocacy is key to make sure they get the care and support they deserve.
Resources Available
Parents and guardians can find many resources. These include educational materials, counseling, and support hotlines. These tools help them manage their child’s condition and make smart care choices.
Community Involvement
Support groups in the community are very important. They offer a place for families to share and get emotional support. Nonprofits and medical groups also help a lot. They work to raise awareness and find new treatments.
It’s important to have a healthcare system that supports families fully. By working together, we can make a better environment for kids with sickle cell disease. This helps them grow healthy and improves their quality of life.
FAQ
What is sickle cell disease and how does it affect children?
Sickle cell disease is a genetic disorder that affects hemoglobin production. This causes red blood cells to be misshapen and break down. Children with SCD may face health issues like anemia, infections, and organ damage.
Our care aims to manage these problems effectively and improve the overall quality of life for children with SCD.
How is sickle cell disease inherited?
Sickle cell disease is inherited in an autosomal recessive pattern. A child needs two defective hemoglobin genes, one from each parent, to develop the disease. We offer genetic counseling to help families understand the risks and implications of SCD.
What are the common complications associated with sickle cell disease in children?
Common complications include acute chest syndrome, sepsis, and stroke. We work to identify and manage these complications early. This helps prevent long-term damage and improves outcomes for children with SCD.
How can viral infections impact children with sickle cell disease?
Viral infections can make SCD symptoms worse and increase the risk of complications. We stress the importance of vaccinations, regular health check-ups, and good hygiene practices. These help prevent infections and manage disease severity.
What are the current treatment options for managing sickle cell disease?
Treatment options include pain management techniques, blood transfusions, and hydroxyurea therapy. We also provide care approaches to address the overall health and well-being of children with SCD.
What advancements are being made in the treatment of sickle cell disease?
Research is ongoing, with developments in gene therapy and clinical trials. These advancements show promise. We stay at the forefront of these developments to offer the latest treatment options for children with SCD.
How can families affected by sickle cell disease access support and resources?
We provide resources for parents and guardians. This includes information on community support groups, nonprofit organizations, and medical organizations dedicated to SCD. These resources help families navigate the challenges of SCD and connect with others who understand their experiences.
What role does socioeconomic status play in pediatric sickle cell mortality?
Socioeconomic status can impact access to healthcare and the quality of care received. This affects outcomes for children with SCD. We work to address these disparities and ensure that all families have access to the care they need.
How can we prevent mortality in children with sickle cell disease?
Preventing mortality in children with SCD requires a multifaceted approach. This includes early diagnosis, complete care, and management of complications. We are committed to providing world-class healthcare to improve survival rates and quality of life for children with SCD.
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41598-024-58328-9
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/sickle-cell/data/index.html