Last Updated on December 2, 2025 by Bilal Hasdemir
Many think that nursing professionals working with children avoid the tough parts of medical care. But, the truth is, pediatric nursing often includes blood draws and transfusions. This is a big part of their job. Discussing the common clinical responsibilities of a Pediatric nurse, including starting IVs, handling blood, and administering transfusions.
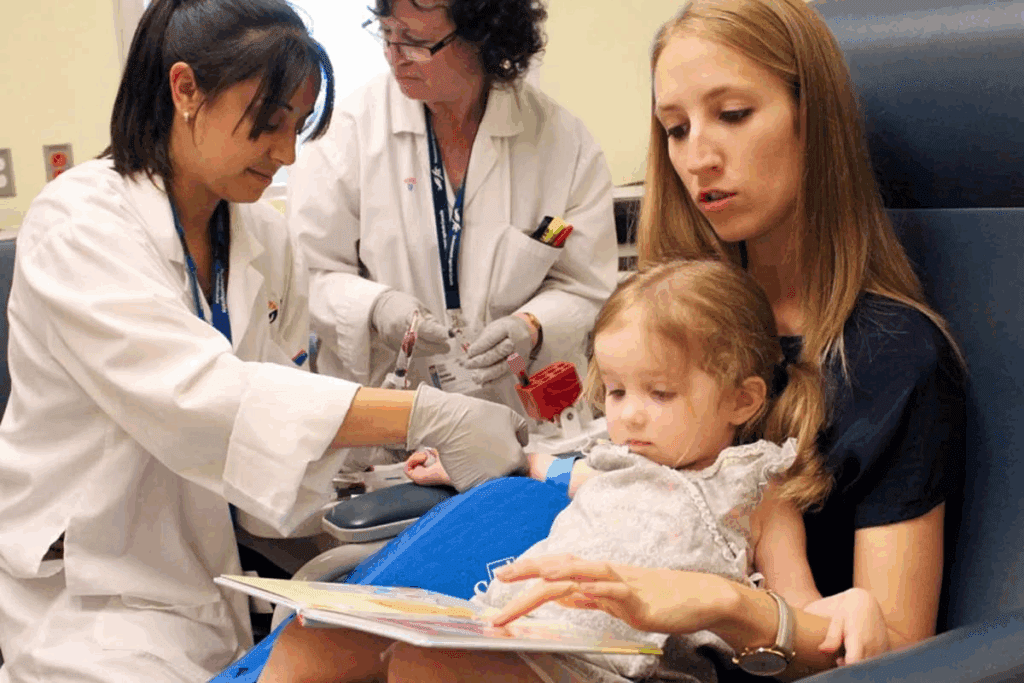
These healthcare providers do more than just medical tasks. They also focus on making their young patients feel comfortable and cared for. Their work is complex, covering many areas of care and support.
Key Takeaways
- Pediatric nurses are involved in various blood-related procedures.
- Their role is not limited to medical procedures but also includes patient comfort and care.
- Understanding the full scope of their duties is essential to appreciating their contributions.
- These healthcare professionals require a unique blend of medical skill and emotional support.
- Their work is critical in providing complete care to children.
Understanding the Role of Pediatric Nurses
Pediatric nurses play a key role in children’s health. They care for kids from birth to teens. Their work is vital for kids’ well-being.
Overview of Pediatric Nursing
Pediatric nursing is a special field. It needs a deep understanding of child growth and health. Pediatric nurses give care like giving medicine and teaching families about health.
They teach families about health, which helps them care for their children more effectively.
Responsibilities of Pediatric Nurses
Pediatric nurses do many things. They give medicine and check on patients. They also do tests and help families feel better.
- Administering medications and treatments as prescribed by physicians.
- Monitoring patients’ conditions and reporting any changes to the healthcare team.
- Performing various medical procedures, such as blood tests and vaccinations.
- Providing emotional support and comfort to children and their families during stressful times.
- Educating families on childcare practices, disease prevention, and management of health conditions.
They need medical knowledge and good communication skills.
Pediatric Nursing Specializations
Pediatric nursing has many special areas. Each one focuses on different parts of child health. Some include:
- Neonatal nursing, focusing on the care of newborns, especially premature or critically ill.
- Pediatric oncology nursing, dedicated to the care of children with cancer.
- Pediatric critical care nursing, involving the care of children who are critically ill or injured.
Each area needs special skills and knowledge. This shows how diverse and complex pediatric nursing is.
Common Medical Procedures Involving Blood
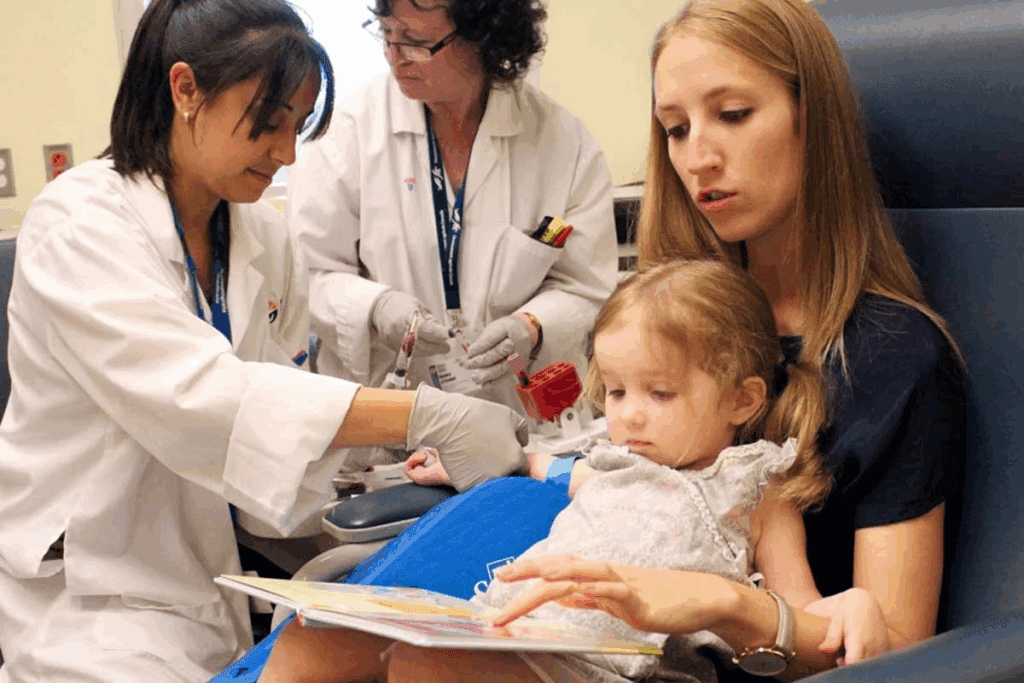
In pediatric care, blood-related medical procedures are common. They need careful handling. Pediatric nurses are key to these procedures, making sure they are done right and safely.
Blood Tests in Pediatric Care
Blood tests are key for diagnosing health issues in kids. Pediatric nurses help kids understand blood tests by explaining them clearly. They also help collect blood samples, making it as comfortable as possible for the kids.
Thanks to pulse oximetry, blood tests are more accurate. This technology checks blood oxygen levels without needing to draw blood, helping doctors make better diagnoses.
Blood Transfusions in Children
Blood transfusions are needed for some health issues or during surgeries. Pediatric nurses give these transfusions, watching the child’s health closely.
It’s very important to keep blood transfusions safe. Nurses check the blood type and make sure it’s compatible before giving it, to avoid bad reactions.
Managing Blood Samples
Handling blood samples is a big job for pediatric nurses. They make sure samples are labeled right and stored safely to avoid mistakes.
Handling blood samples correctly is vital for getting accurate lab results. These results help doctors figure out what’s wrong and how to treat it. Nurses follow strict rules to keep samples safe.
In summary, pediatric nurses are vital in managing blood-related medical procedures. Their skill and care help make these procedures safe and effective for kids.
Safety Protocols for Handling Blood
In pediatric care, handling blood is a big deal. We must follow strict safety rules to avoid infections. Pediatric nurses are trained to keep both patients and healthcare workers safe.
Infection Control Measures
Keeping blood handling safe is key in pediatric care. We follow strict infection control rules. This includes using sterile tools and keeping areas clean.
- Proper hand hygiene before and after handling blood samples
- Using sterile needles and equipment for blood draws
- Ensuring that all surfaces are cleaned and disinfected regularly
The Centers for Disease Control and Prevention (CDC) says following these rules is vital. It helps prevent the spread of bloodborne pathogens.
“The prevention of bloodborne pathogen transmission in healthcare settings relies heavily on adherence to standard precautions, including the use of personal protective equipment and safe injection practices.”
CDC Guidelines
Personal Protective Equipment (PPE)
Using Personal Protective Equipment (PPE) is essential for safe blood handling. PPE like gloves, masks, and gowns protects against pathogens. We make sure to:
| PPE Component | Purpose |
| Gloves | Prevent skin contact with blood |
| Masks | Reduce the transmission of airborne pathogens |
| Gowns | Protect clothing from contamination |
Safe Disposal of Blood Waste
Disposing of blood waste safely is also critical. We have strict rules for disposing of blood samples and materials. This includes:
- Using biohazard containers for disposing of blood-contaminated materials
- Ensuring that all waste is properly labeled and segregated
- Adhering to local regulations and guidelines for biohazard waste disposal
By sticking to these safety steps, we lower the risk of infection. This ensures a safe place for our young patients.
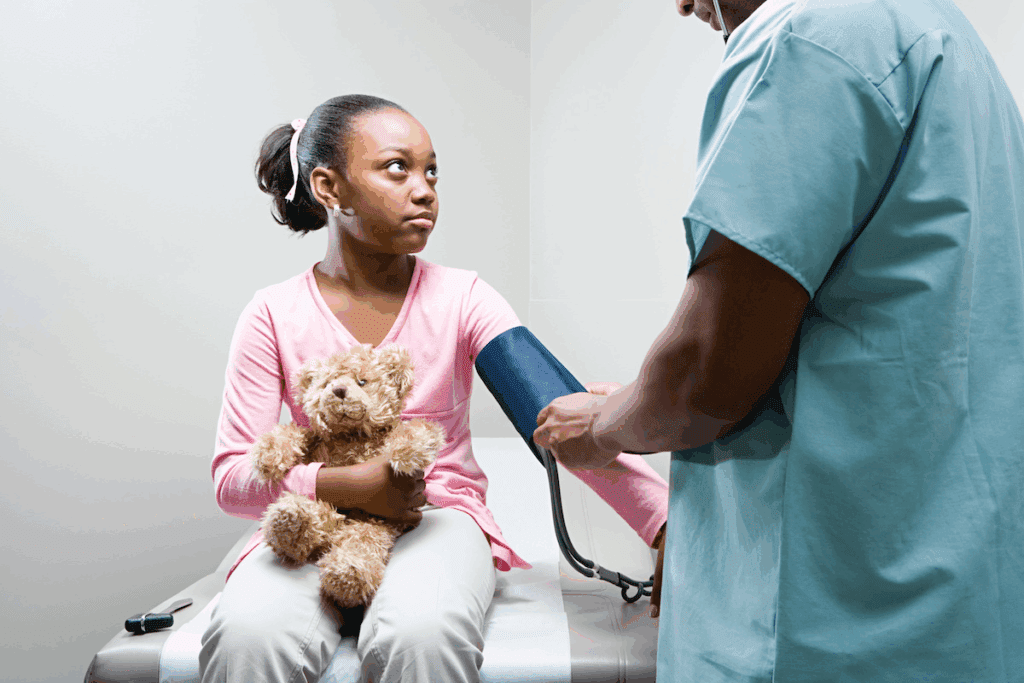
Emotional Support for Young Patients
When kids have blood-related medical procedures, pediatric nurses play a big role in their emotional support. These procedures can be scary for young patients. It’s our job to make them feel supported and comforted.
Preparing Children for Blood-Related Procedures
Preparing kids for blood-related medical procedures is a delicate task. It needs empathy, clear explanations, and a child-friendly approach. We use simple language to explain the procedure and its importance for their health.
For younger kids, we use visual aids and simple explanations. Older kids and teens get more detailed information. We encourage them to ask questions, helping them feel in control.
Coping Strategies for Pediatric Patients
Teaching coping strategies is key to our emotional support. We help kids manage their anxiety and discomfort. Techniques include deep breathing, visualization, and distraction, like watching a favorite movie.
| Coping Strategy | Age Group | Description |
| Deep Breathing | 4-12 years | Encourages slow, deep breaths to calm the child. |
| Visualization | 6-18 years | Guides the child to imagine a happy, safe place. |
| Distraction | 3-16 years | Uses activities or media to divert the child’s attention. |
Communicating Effectively with Families
Communicating well with families is also important. We keep parents and guardians updated on the child’s procedures and condition. This helps reduce their anxiety and prepares them to support their child.
By working with families, we create a better support system for the child. We address both their medical and emotional needs.
Training and Education for Pediatric Nurses
Effective pediatric nursing needs a mix of training and education. It includes both book knowledge and hands-on skills. Pediatric nurses must be ready to handle the challenges of caring for children, including blood procedures.
Certifications and Licenses
Pediatric nurses need the right certifications and licenses to work. They start with a nursing degree, pass the NCLEX-RN exam, and get extra certifications like the Certified Pediatric Nurse (CPN) credential.
“The importance of certification cannot be overstated,” says a leading nursing expert. “It shows a nurse’s skill and commitment to quality care.” As noted in a recent nursing journal,
“Certification is a critical component of professional development, improving patient care and advancing nursing.”
Clinical Training in Blood Procedures
Clinical training is key for pediatric nurses, focusing on blood procedures. They learn blood sampling techniques, transfusion procedures, and how to handle problems.
- Venipuncture and blood sampling
- Blood transfusion administration
- Monitoring for adverse reactions
Through practical training and simulations, nurses become confident and skilled in these procedures.
Continuing Education Opportunities
The field of pediatric nursing keeps changing, with new methods and practices. Continuing education is vital for nurses to keep up and offer top care.
There are many ways to keep learning, like workshops, conferences, and online courses. Topics include pediatric hematology, nursing innovations, and family-centered care. Ongoing education helps nurses improve their skills, knowledge, and patient care.
We understand that pediatric nursing is always evolving. It’s our goal to support nurses with thorough training and education.
Challenges Pediatric Nurses Face
Pediatric nurses face many challenges in their work. They must handle emergencies, manage anxiety, and support families. Their role is critical in healthcare, needing a mix of medical skills, emotional understanding, and communication abilities.
Dealing with Emergencies Involving Blood
Handling blood emergencies is tough for pediatric nurses. They need to act fast, make smart decisions, and stay calm. They handle blood transfusions, manage bleeding, and respond to injuries, all while keeping the child and family calm.
Quick decision-making is key in these situations. Nurses must assess fast, decide quickly, and act swiftly. They need strong pediatric care skills and the ability to stay focused under pressure.
Key Strategies for Managing Emergencies:
- Staying calm and composed under pressure
- Rapid assessment and decision-making
- Effective communication with the child and their family
- Collaboration with the healthcare team
Balancing Care and Anxiety Management
Pediatric nurses must provide top-notch care while managing anxiety in children. They create a supportive environment, explain things in a way kids can understand, and use strategies to reduce stress.
“The art of pediatric nursing lies not just in the technical skills, but in the ability to connect with children and their families, to understand their fears, and to alleviate their anxieties.”
— Pediatric Nursing Expert
Managing anxiety is vital in pediatric care. High anxiety can harm a child’s experience and outcome. Nurses use distraction, relaxation, and education to help children deal with anxiety.
| Anxiety Management Techniques | Description | Age Group |
| Distraction | Using toys or activities to divert attention from the procedure | 2-6 years |
| Relaxation Techniques | Teaching deep breathing or progressive muscle relaxation | 6-12 years |
| Education | Explaining the procedure in a clear, age-appropriate manner | All ages |
Addressing Familial Concerns
Supporting families is a big part of pediatric nursing. Families are stressed and anxious when their child is sick. Nurses provide emotional support and clear information.
Nurses must understand families’ worries, give accurate info, and involve them in care. This helps reduce anxiety and improves care for the child.
Effective Communication Strategies:
- Listening actively to the family’s concerns
- Providing clear, concise information about the child’s condition and treatment
- Involving families in care decisions and planning
- Offering emotional support and reassurance
The Importance of Pediatric Blood Donor Programs
Blood donor programs for kids are key to their health. They make sure children get the right blood for their needs. This is vital for kids with medical conditions.
Benefits of Pediatric Blood Donations
Pediatric blood donations are very helpful. They provide blood that matches a child’s type, which is hard to find. This blood is needed for surgeries and treating diseases like leukemia.
These donations also lower the risk of bad reactions from blood transfusions. This is because the blood is safe and right for young patients. Pediatric nurses work hard to make sure kids get the best care.
How Pediatric Nurses Promote Donor Awareness
Pediatric nurses lead in spreading the word about blood donation. They teach families and the community about its importance. They clear up any wrong ideas about giving blood.
We use many ways to get the message out. We hold events, use social media, and work with schools. Our goal is to get more people to donate blood.
Case Studies of Successful Initiatives
Pediatric nurses have started many successful programs. For example, a hospital in the U.S. ran a campaign. It led to more blood donations for kids. They used social media, events, and partnerships to help.
Another program educated families about blood donation during visits. It not only increased donations but also brought families together. They all supported the same cause.
Advances in Technology Impacting Blood Handling
Medical technology is changing how pediatric nurses handle blood tests and transfusions. These new tools make blood handling safer and more accurate. They also help improve patient care and experiences.
Innovations in Blood Test Techniques
New tech has made blood tests better. Micro-sampling techniques take smaller blood samples, making tests less painful for kids. Point-of-care testing lets nurses test blood right at the bedside. This means quicker results and faster medical actions.
| Innovation | Description | Benefit |
| Micro-sampling | Collection of smaller blood samples | Reduced patient discomfort |
| Point-of-care testing | Bedside blood testing | Immediate results for timely decisions |
Telemedicine and Remote Monitoring
Telemedicine and remote monitoring are changing pediatric care. Virtual consultations let nurses check on patients without them having to go to the hospital. This cuts down on hospital visits and lowers infection risks. Remote monitoring keeps an eye on patients’ health 24/7, catching problems early.
- Virtual consultations reduce hospital visits
- Remote monitoring enables continuous patient tracking
- Early intervention through real-time data analysis
Future Trends in Pediatric Nursing
We’re expecting more use of artificial intelligence (AI) and machine learning (ML) in pediatric nursing. These tools can predict patient needs and make care more personalized. Nanotechnology might also make blood tests easier and less invasive.
As tech keeps getting better, pediatric nurses need to keep up. By using these new tools, we can make care safer, better, and more caring. This is key for improving patient outcomes and experiences.
Recognizing and Managing Blood Disorders in Children
It’s key for nurses to spot and handle blood disorders in kids. They need to be very careful and caring. Nurses play a big role in treating these issues, which greatly affect a child’s life.
Common Blood Disorders in Pediatrics
Kids can have different blood disorders, from mild to serious. Anemia is when there’s not enough red blood cells, causing tiredness. Hemophilia makes it hard for blood to clot, leading to ongoing bleeding.
Knowing about these conditions helps nurses give the right care. We’ll look into these disorders and how they’re treated in kids.
Symptoms and Diagnosis
Doctors use physical checks, medical history, and lab tests to find blood disorders in kids. Signs include fatigue, pale skin, and often getting sick. Tests like blood smears and bone marrow biopsies help pinpoint the exact issue.
Finding the problem early is key to better treatment and results for kids with blood disorders.
Treatment Options and Support
Treatment for blood disorders in kids varies based on the condition and how bad it is. It might include medication, blood transfusions, or even bone marrow transplants. It’s also important to offer support like nutrition advice and emotional help.
We stress the need for a full care plan. It should cover both the medical and emotional needs of kids with blood disorders.
Conclusion: The Vital Role of Pediatric Nurses in Blood Management
Pediatric nurses are key in managing blood, from tests to transfusions. They also offer emotional support to kids. Their work helps promote healthy living and supports young patients.
Impactful Experiences
Pediatric nurses are dedicated to top-notch care. They handle blood tests and transfusions with care. This shows their commitment to better patient results.
Shaping the Future
The future of pediatric nursing looks bright. New tech and education will help them manage blood procedures better. Pediatric nurses will keep shaping pediatric care’s future.
Continuing Advocacy
We must keep pushing for young patients’ needs. Raising awareness about pediatric blood donor programs is key. This way, pediatric nurses can give the best care to their patients.
FAQ
What does a pediatric nurse do?
Pediatric nurses care for kids from birth to teens. They give medicine, do tests, and teach families about health. This helps kids stay healthy.
What kind of medical procedures do pediatric nurses perform involving blood?
They do blood tests and transfusions. These are key for diagnosing and treating kids’ health issues.
How do pediatric nurses ensure Page safety when handling Prospective blood?
They follow strict safety rules. This includes infection control, wearing PPE, and disposing of blood safely.
What kind of emotional support do pediatric nurses provide to young patients undergoing blood-related procedures?
They prepare kids for procedures, teach them how to cope, and support families. This helps kids feel better.
What kind of training and education do pediatric nurses require to perform their duties effectively?
They need special training and education. This includes getting certifications, learning about blood procedures, and staying updated through continuing education.
What kind of challenges do pediatric nurses face when dealing with blood-related procedures?
They deal with emergencies, manage anxiety, and address family concerns. It’s a tough job.
How do pediatric nurses promote pediatric blood donor programs?
They raise awareness and start successful programs. This ensures there’s enough blood for kids who need it.
What are some advances in technology that have impacted blood handling and testing techniques in pediatric care?
New tech has improved blood work. This includes better tests, telemedicine, and remote monitoring. It helps nurses care for kids better.
How do pediatric nurses recognize and manage blood disorders in children?
They are key in spotting and treating blood disorders. They know the common ones, how to diagnose, and what treatments work.
Why is continuing education important for pediatric nurses?
It keeps them up-to-date with new medical info and tech. This ensures they give the best care to their patients.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35206126/
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35206126/