Last Updated on December 2, 2025 by Bilal Hasdemir
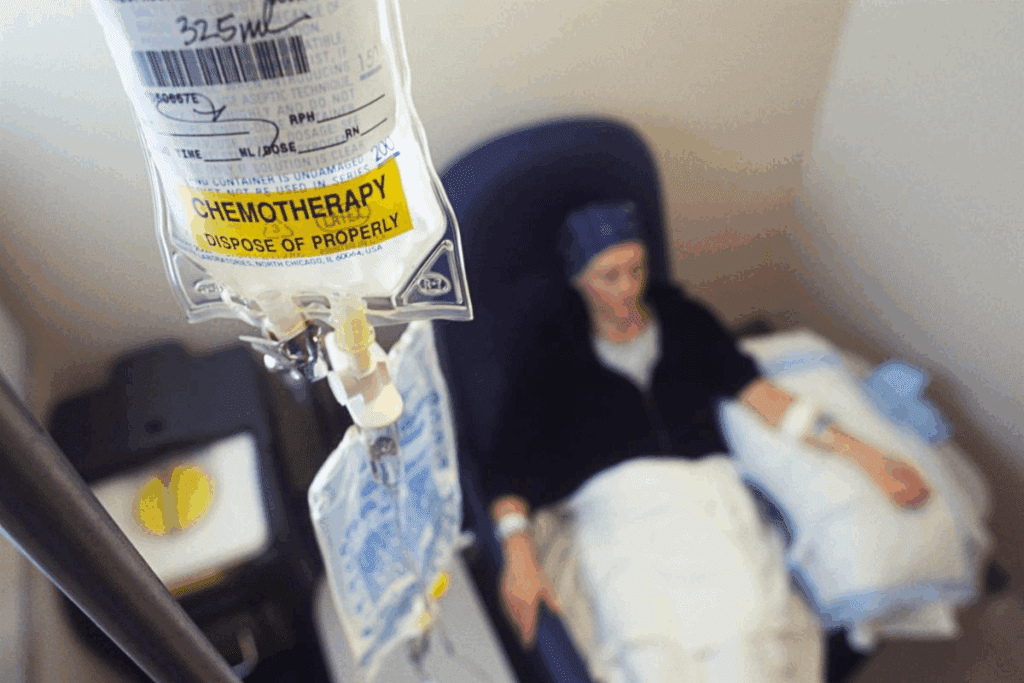
Nearly 70% of patients getting Hematopoietic Stem Cell Transplantation (HSCT) need blood transfusions. This is because their treatment is very intense, as shown in a study in JAMA Network Open. This shows how closely chemotherapy and blood transfusions are linked in cancer treatment. Explaining how chemotherapy-induced bone marrow suppression creates the common need for Chemotherapy and blood transfusions.
Chemotherapy can really hurt the body’s ability to make healthy blood cells. This can lead to problems that might need transfusions. So, it’s very important for patients to know the good and bad sides of these treatments.
Key Takeaways
- Patients undergoing HSCT are at a high risk for BSIs and associated morbidity and mortality.
- Chemotherapy can lead to a significant need for blood transfusions due to its impact on blood cell production.
- Understanding the connection between chemotherapy and blood transfusions is important for cancer patients.
- Transfusions are often needed to fix problems caused by chemotherapy.
- Knowing the risks and benefits helps patients make better choices about their care.
What is Chemotherapy?
Chemotherapy is a treatment that uses strong drugs to fight cancer cells. It’s a common treatment for many cancers, including lung cancer.
Definition and Purpose
Chemotherapy uses drugs to kill or slow down cancer cells. Its main goal is to shrink tumors, ease symptoms, and stop cancer from spreading.
Chemotherapy can be used alone or with other treatments like surgery or radiation. The choice depends on the cancer type, its stage, and the patient’s health.
Common Chemotherapy Drugs
Many drugs are used in chemotherapy, each working in its own way. Some well-known drugs include:
| Drug Name | Cancer Type | Mechanism of Action |
| Cisplatin | Testicular, ovarian, lung, bladder cancer | Interferes with DNA replication PageAnalysis td> |
| Doxor PageAnalysis ubin | Breast, bladder, lymphoma, leukemia | Intercal PageAnalysis ates DNA strands, inhibiting macromolecular biosynthesis |
| 5-Fluorouracil (5-FU) | Colon PageAnalysis , breast, skin cancer | Inhibits thymidylate synth Page PageAnalysis ase PageAnalysis , disrupting DNA synthesis |
Administration Methods
Chemotherapy can be given in different ways, based on the drug and the patient. Common ways include:
- Oral Administration: Some drugs are taken as pills or liquids.
- Intravenous (IV) Administration: Many drugs are given through an IV line.
- Intra-arterial Administration: In some cases, drugs are given directly into an artery.
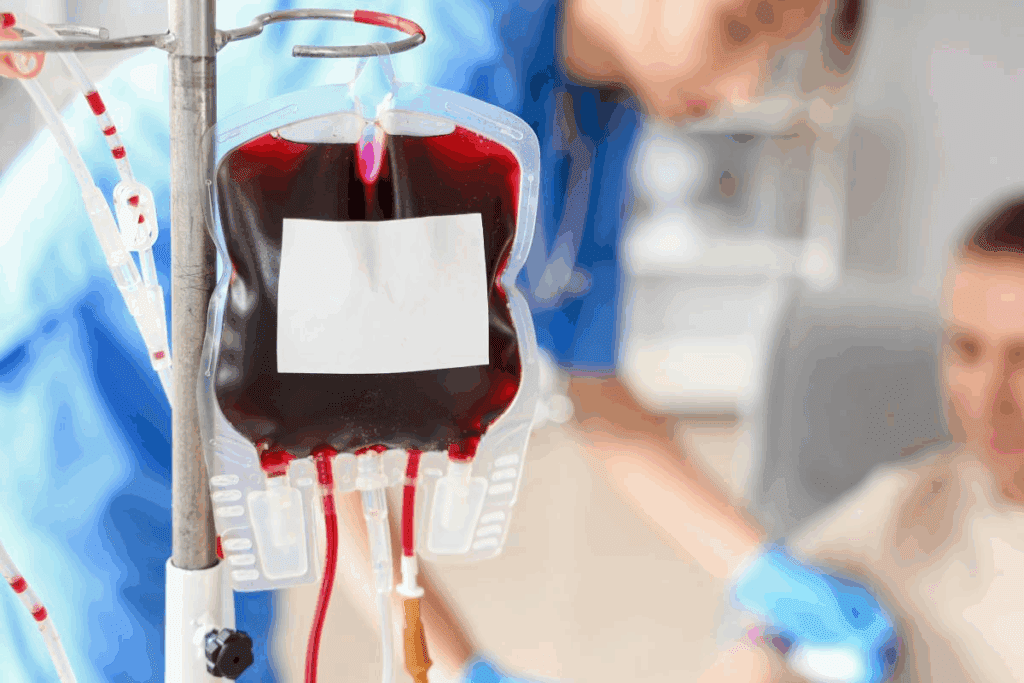
The Role of Blood Transfusions in Cancer Treatment

Blood transfusions are key in cancer treatment, mainly for those getting chemotherapy. Chemotherapy fights cancer well but can cause side effects like anemia. Blood transfusions help manage these issues and keep patients healthy.
Why Transfusions Are Needed
Chemotherapy can harm the bone marrow, reducing red and white blood cells and platelets. This can lead to anemia, infections, or bleeding problems. Blood transfusions help by adding to the patient’s blood cell count. For example, red blood cell transfusions treat anemia, helping tissues get enough oxygen and reducing tiredness.
The need for blood transfusions changes based on the cancer type, chemotherapy strength, and patient health. Yet, in many cases, transfusions are vital for supportive care. They help patients handle their treatment better.
Types of Blood Products Used
Many blood products are used in cancer treatment, each for a different reason.
- Red blood cells: To improve oxygen delivery and alleviate anemia.
- Platelets: To prevent or treat thrombocytopenia and associated bleeding risks.
- Granulocytes: To support patients with life-threatening infections.
- Plas Page Page>Fresh frozen plasma: To correct coagulopathy or provide clotting factors.
Healthcare providers use these blood components to customize transfusion therapy. This improves patient care and outcomes.
Increased Risk of Blood Transfusion Reactions in Oncology Patients
Oncology patients getting chemotherapy face a higher risk of bad reactions to blood transfusions. It’s key to know why this risk is higher.
What Are Transfusion Reactions?
Transfusion reactions happen when the body doesn’t take well to the blood it’s given. This can be due to the blood not matching the patient’s immune system. These reactions can be mild or very serious, even life-threatening. Healthcare providers must watch patients closely during and after transfusions to spot and handle any bad reactions fast.
The signs of transfusion reactions vary but often include fever, chills, and a rash. Severe cases can cause breathing problems, heart issues, or anaphylactic shock. Quick action is vital to avoid serious problems.
Factors Page Contributing to Increased Risk
Several things make oncology patients more likely to have bad reactions to blood transfusions. First, chemotherapy weakens the immune system, making patients more at risk. Also, these patients often need blood transfusions more often, which raises the chance of a bad reaction.
- Chemotherapy-induced immunosuppression
- Frequent blood Page transfusions
- Underlying health Page conditions
Knowing these factors helps us find ways to lower the risk. We need to carefully decide when blood transfusions are needed and take steps to reduce risks. This way, we can make sure oncology patients get the care they need without exposing them to too many risks.
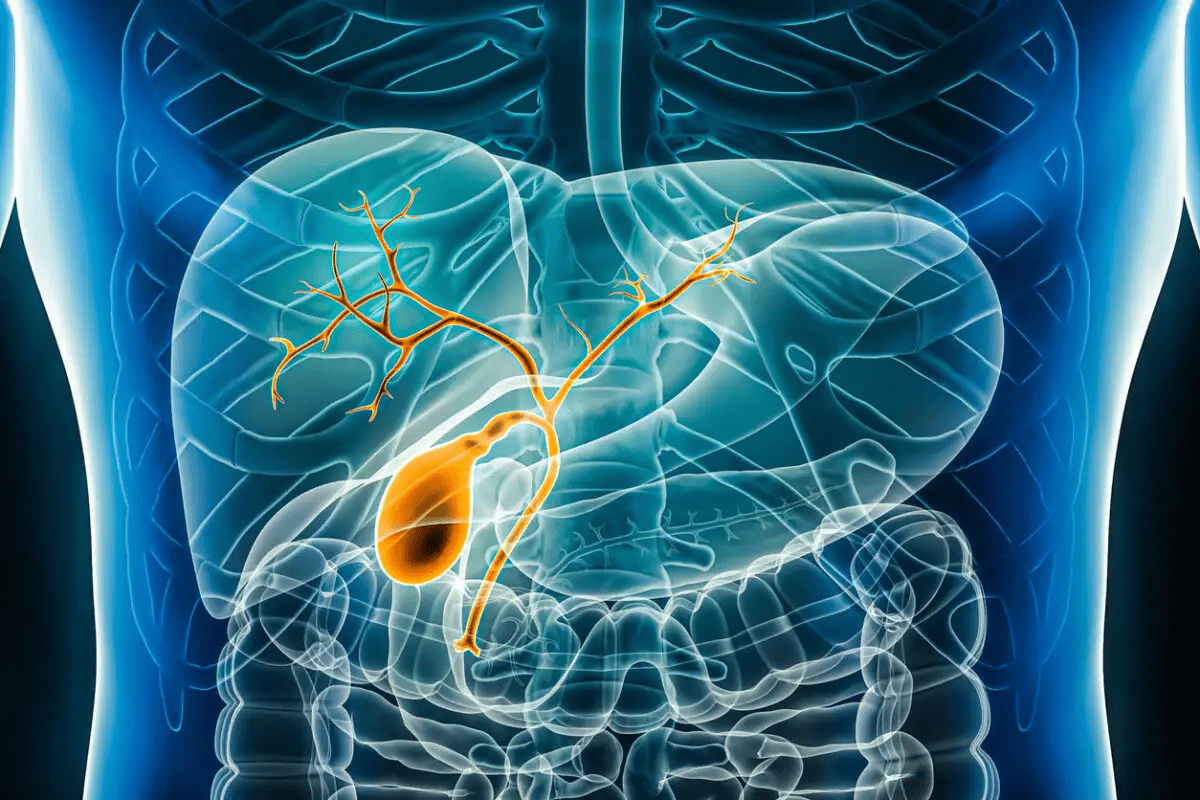
The Mechanism Behind Chemotherapy-Induced Anemia
It’s important to know how chemotherapy causes anemia in cancer patients. Chemotherapy is a term for many drugs used to fight cancer. These drugs target fast-growing cancer cells but can harm other fast-growing cells too, like those in the bone marrow.
How Chemotherapy Affects Blood Cell Production
Chemotherapy can slow down the bone marrow. This means fewer red blood cells, white blood cells, and platelets are made. Red blood cells carry oxygen, and without enough, anemia can occur.
The severity of this effect varies. It depends on the type of chemotherapy, the dose, and how the patient reacts.
Chemotherapy can also cause myelosuppression. This is when blood cell production drops. It makes patients more likely to get anemia, infections, and bleeding problems. The biggest issue is the drop in red blood cells, which directly causes anemia.
Symptoms of Anemia in Cancer Patients
Anemia can show in many ways, affecting a patient’s life quality. Common symptoms include fatigue, . These happen because the body’s tissues and organs don’t get enough oxygen.
In cancer patients on chemotherapy, spotting anemia symptoms early is key. Managing anemia well can help patients handle chemotherapy better. This might include blood transfusions, iron supplements, or treatments to boost red blood cell production.
Identifying Signs of Transfusion Reactions
When someone gets a blood transfusion, it’s key to know the signs of a reaction. These can happen during or right after the transfusion. We stress the need to watch closely for these signs to act fast if needed.
Immediate Symptoms to Watch For
Transfusion reactions show up in different ways. Knowing the early signs is important. Here are some common ones:
- Fever: A high body temperature can signal a reaction.
- Chills: Feeling cold or shaking can be a sign.
- Rash or Hives: Skin issues like rashes or hives might mean an allergic reaction.
- Shortness of Breath: Trouble breathing or feeling like you can’t catch your breath is serious.
If you notice any of these symptoms during or after a transfusion, tell your healthcare team right away.
Long-term Monitoring and Follow-up
Reactions can happen right away or later, even weeks after. It’s important to watch your health closely. If you notice anything odd, tell yourhealthcare provider.
Regular check-ups are key to tracking how your body reacts to the transfusion. These visits help catch any problems early. Blood tests might be part of this monitoring to check on your blood cells and overall health.
Keeping a symptom journal is helpful. This way, you can talk about any changes with your healthcare team. Being aware and proactive helps manage your health better. As your healthcare team, we’re here to support you every step of the way.
Best Practices for Safe Blood Transfusion in Chemotherapy
Blood transfusions are key in chemotherapy care, needing strict safety steps. We’ll look at the top ways to keep blood transfusions safe during chemotherapy. This includes pre-transfusion checks and watching the patient during the transfusion.
Pre-Transfusion Screening Procedures
Checking the blood before transfusion is very important. It makes sure the blood is safe for the patient. Here are the main steps:
- Patient Identification: Making sure the right patient gets the blood.
- Blood Typing: Matching the donor’s blood type with the patient’s.
- Cross-Matching: Testing the patient’s blood against the donor’s to avoid bad reactions.
These steps help lower the chance of bad reactions from the blood.
Monitoring During Transfusion
Watching the patient closely during transfusion is also key. We need to look out for signs of bad reactions, like fever or rash. Here’s what to watch for and what to do:
| Monitoring Parameter | Action |
| Fever | Stop transfusion, tell the doctor |
| Chills or Rigors | Slow down the transfusion, check for reaction |
| Rash or Hives | Stop transfusion, give antihistamines if needed |
By sticking to these practices, we can greatly lower the risks of safe blood transfusion in chemotherapy patients. This ensures they get the care they need.
In summary, safe blood transfusion practices are critical in chemotherapy care. By focusing on pre-transfusion checks and careful monitoring, we can keep our patients safe during chemo and blood transfusions.
Importance of Matching Blood Types and Compatibility
Blood type matching is vital to prevent bad reactions during blood transfusions. This is common for cancer patients. The process of blood transfusion is complex and has many steps to keep patients safe.
Overview of Blood Type Systems
The human blood type is mainly split into four groups: A, B, AB, and O. Each group can be either Rh positive or Rh negative. Knowing these blood types is key for safe transfusions. The ABO and Rh blood group systems are the most important in transfusion medicine.
| Blood Type | Antigens Present | Can Receive Blood From |
| A+ | A and RhD | A+, A-, O+, O- |
| O- | None | O- |
| AB+ | A, B, and RhD | AB+, AB-, A+, A-, B+, B-, O+, O- |
| B- | B | B-, O- |
Page 1>
Crossmatching Procedures
Crossmatching is a test to check if the patient’s blood and the donor’s blood are compatible. It mixes the patient’s blood with the donor’s to look for bad reactions. We are very careful with crossmatching to lower risks.
- Pre-transfusion testing checks the patient’s blood type and looks for antibodies.
- The crossmatch test confirms if the blood is compatible.
- Then, the blood is given for transfusion with careful checks of patient and donor details.
By focusing on blood type compatibility and strict crossmatching, we can greatly reduce transfusion risks. Our goal is to give safe and effective care to all patients getting blood transfusions.
Patient Education on Risks and Benefits of Transfusions
It’s important for patients to know about the risks and benefits of blood transfusions, mainly when they’re getting chemotherapy. We, as healthcare providers, have a big role in teaching them. We explain why transfusions are needed, the risks, and the good they can do.
Teaching patients well helps them make better choices about their health. When they know what’s going on, they’re more likely to stick to their treatment plans. This helps them manage their health better.
Discussing Transfusion Necessity with Patients
Talking to patients about blood transfusions means explaining why they’re needed. We tell them what the process is and how it will help their treatment. It’s key to make sure they understand why they need a transfusion.
For example, chemotherapy can cause anemia, which means not enough red blood cells. A transfusion can help by increasing red blood cells. This improves oxygen delivery and can reduce symptoms like tiredness and shortness of breath.
| Benefits of Blood Transfusions | Risks Associated with Blood Transfusions |
| Increased red blood cell count | Transfusion reactions |
| Improved oxygen delivery | Infection transmission |
| Reduced fatigue and weakness | Allergic reactions |
Empowering Patients to Ask Questions
It’s important to let patients ask questions about blood transfusions. We encourage them to ask about risks, benefits, the process, and if there are other options. This helps them feel more in control of their care.
By talking openly, we can clear up any worries they have. We make sure they feel supported during their treatment.
Key Questions Patients May Ask:
- Why do I need a blood transfusion?
- What are the risks associated with blood transfusions?
- How will a blood transfusion benefit my treatment?
- Are there any alternatives to blood transfusions?
By answering these questions, we give our patients the care they need. We meet their physical and emotional needs.
Emotional and Psychological Aspects of Blood Transfusions
Getting a blood transfusion can be tough for patients with cancer. It’s not just about the physical side. It also affects their emotions and minds. We focus on these areas to give full care.
Coping with Anxiety Related to TreatmentPageSpeed>3>
Patients might worry about the blood transfusion. They might fear reactions or how it will affect their cancer treatment. Healthcare providers need to listen and support them.
Here are ways to deal with this worry:
- Talking openly with doctors
- Learning about the transfusion
- Getting help from loved ones and groups
Support Resources for Patients
Having the right support can really help patients. We make sure they know where to find help.
| Resource | Description | Benefit |
| Support Groups | Connects patients with others who have gone through similar things | Emotional support and a sense of community |
| Counseling Services | Offers professional help to manage anxiety and emotional challenges | Personalized support |
| Educational Materials | Provides info on the transfusion process and its effects | Helps patients understand and feel empowered |
Advances in Blood Safety and Technology
Medical technology has changed transfusion medicine a lot. Now, healthcare providers can give safer treatments. We see big improvements in blood safety thanks to new screening methods and blood products.
Enhanced Screening Techniques
New screening methods have cut down the risk of infections from blood transfusions. Advanced nucleic acid testing (NAT) is key in finding viruses like Hepatitis B, C, and HIV. It spots viral genetic material early, before antibodies show up.
“The use of NAT has changed blood safety a lot,” experts say. “It lets us find viruses sooner, lowering the risk of passing them on.”
New Blood Products and Their Benefits
New blood products have given patients more options during chemotherapy. Pathogen-reduced platelet concentrates are safer against new pathogens. They’re treated to kill or remove pathogens, making transfusions safer.
- Pathogen-reduced platelet concentrates
- Cryop Page recipitate Page for fibrinogen replacement
- Advanced red blood cell products with extended storage capabilities
These advances have made treatments safer and more effective. As we keep innovating, we’ll see even better treatments for chemotherapy patients.
Regulatory Guidelines for Blood Transfusions in Oncology
Regulatory guidelines are key to safe blood transfusions in oncology. They help ensure blood transfusions are given safely and effectively. This is important for patients getting cancer treatment.
era >
FDA Regulationsera >
The FDA is vital in keeping blood transfusions safe in the U.S. They cover screening blood donations, preparing blood components, and reporting bad reactions. These rules aim to stop infectious diseases and make sure blood products are good quality.
The FDA makes sure blood donations are tested for diseases like HIV and hepatitis. They also require blood places to follow good practices to keep blood safe and pure.
Hospital Protocols
Hospitals have their own rules for blood transfusions to keep patients safe. These rules include checking patients before transfusions, watching them during, and handling any bad reactions. Hospitals must follow these rules to lower risks from blood transfusions.
Good hospital protocols need teamwork. Doctors, transfusion experts, and lab workers all play a part. Working together helps make sure blood transfusions are safe and follow the rules.
Page Structure
“The safety of blood transfusions is a multi-faceted issue that requires careful coordination among healthcare providers, regulatory agencies, and blood establishments.”
Future Research Directions in Blood Transfusions and Cancer Care
As we keep pushing forward in cancer treatment, blood transfusions play a key role. Research is ongoing to make transfusions safer and more effective. This is very important, mainly when patients are getting chemotherapy.
Ongoing Studies
Many clinical trials are looking into new ways to use blood transfusions in cancer treatment. They want to lower the chance of bad reactions and make patients do better. We’re also looking into new blood products and more focused transfusion methods.
Innovations on the Horizon
Future research will likely be influenced by new technology and our growing knowledge. We’ll see more tailored and effective transfusion treatments. This will help improve care for cancer patients.
FAQ
What is the connection between chemotherapy and blood transfusions?
Chemotherapy can cause anemia and other blood issues. This might need blood transfusions to fix. They help get oxygen to the body’s tissues.
Why do cancer patients need blood transfusions?
Cancer patients often need blood transfusions. This is because chemotherapy can cause anemia. It also helps prevent or treat bleeding problems.
What are the risks associated with blood transfusions in oncology patients?
Blood transfusions can be risky. They might cause reactions, iron overload, or infections. Cancer patients are more at risk because of their health.
Page How does chemotherapy affect blood cell production?
Chemotherapy harms the bone marrow. This leads to fewer blood cells. It causes anemia, low white blood cells, and low platelets.
What are the symptoms of anemia in Press cancer Page Page patients?
Anemia symptoms include feeling tired, weak, and short of breath. Dizziness is also common.
What are the immediate symptoms of a transfusion reaction?
Symptoms of a reaction include fever, chills, and itching. Hives and trouble breathing are also signs. Tell your doctor right away if you notice these.
How can patients minimize the risks associated with blood transfusions?
To reduce risks, understand why you need a transfusion. Ask questions and watch your body closely during and after. Make sure the blood is compatible with yours.
Why is patient education Page Page important in blood transfusions Press for on Page erafty-P zee R Pageоми sof Page Page?
Learning about blood transfusions helps patients. It lets them ask smart questions and take part in their care. This leads to better health.
What advancements have been made in blood Page safety and technology? Page H3>
New screening methods for diseases and blood products like irradiated and leukoreduced blood have been developed. These reduce risks.
What regulatory guidelines govern blood transfusions in oncology?
Page
FDA rules and hospital protocols ensure blood transfusions are safe and of high quality in oncology.Page Page
What are the future research directions in blood transfusions and cancer care?
Research aims to improve blood safety and develop new products. It also looks into alternatives to transfusions, like erythropoiesis-stimulating agents.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21261607/
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21261607/