Last Updated on December 2, 2025 by Bilal Hasdemir

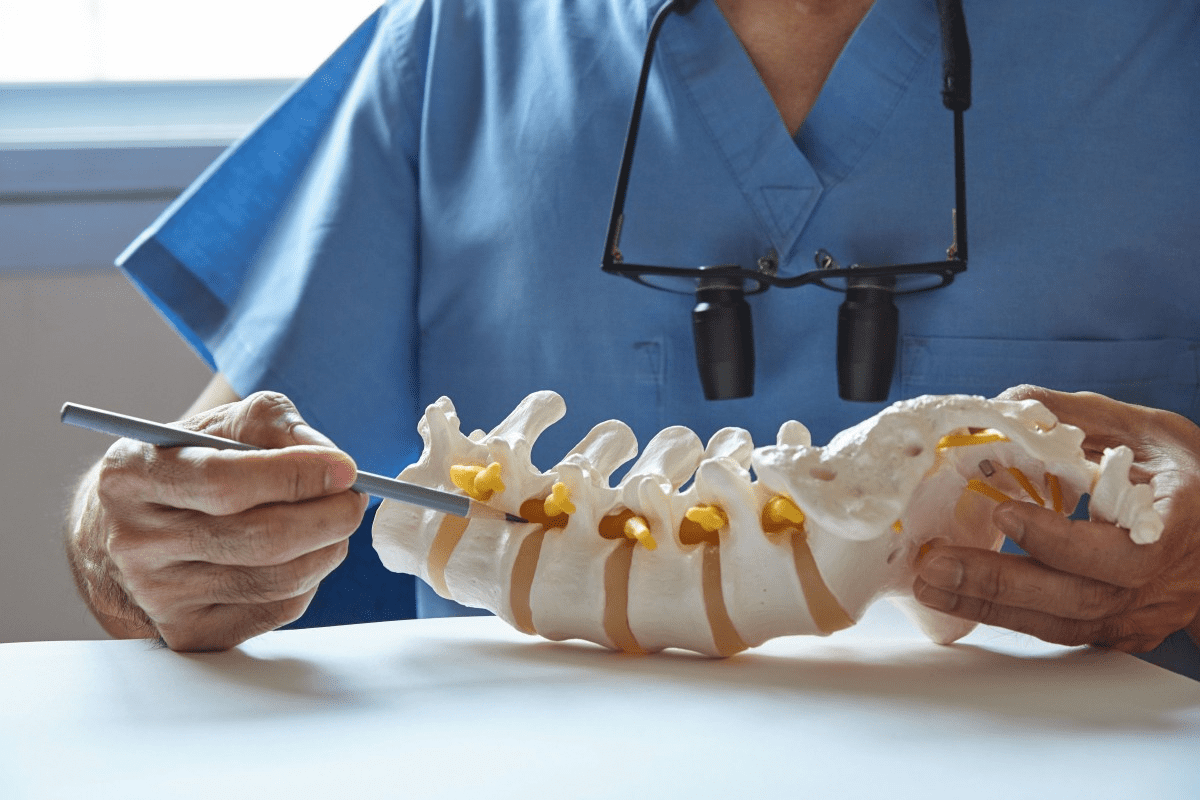
Surgical approach optimization is critical. Discover the amazing and essential positions used in neurosurgery to ensure patient safety. Neurosurgical procedures need precise patient positioning for the best results. The way a patient is positioned during surgery is key. It affects how well the surgeon can access the brain or spine.
The supine position is most often used in neurosurgery. It gives the best access to different parts of the brain. are made as needed during the surgery.
The role of patient positioning is very important. It plays a big part in the success of the surgery and how well the patient recovers.
Key Takeaways
- The supine position is the most commonly used in neurosurgery.
- Proper patient positioning is key for the success of neurosurgical procedures.
- Patient positioning affects both surgical access and patient recovery.
- Neurosurgeons must carefully plan and execute patient positioning.
- Optimal patient positioning can vary depending on the specific neurosurgical procedure.
Overview of Neurosurgical Positioning Fundamentals
Neurosurgical positioning has grown a lot. It’s key for the success of brain surgeries. The right position of a patient is very important.
Historical Evolution of Neurosurgical Positioning
The history of neurosurgical positioning goes back a long way. Early methods were simple but sometimes caused problems.
Early Positioning Techniques
At first, positioning was basic and often made patients uncomfortable. These methods were later improved.
Modern Advancements in Patient Positioning
Today, neurosurgery has made big steps forward. New tools and methods help doctors get better access and improve results.
Importance of Proper Positioning in Neurosurgery
Getting the position right is very important in neurosurgery. It affects how well doctors can see and work. The right position can greatly improve results.
Impact on Surgical Access and Visualization
Good positioning lets surgeons have the best access and view. This is key for successful brain surgeries.
Effect on Patient Outcomes
The right positioning greatly affects how well patients do. It lowers the chance of problems and helps patients recover faster.
Supine Position: The Gold Standard in Neurosurgery
In neurosurgery, the supine position is often chosen for many operations. This is because it offers hemodynamic stability and makes airway management easier. It gives the best access to the front and middle parts of the brain, making it perfect for many neurosurgical procedures.
Anatomical Considerations and Applications
The supine position is great for surgeries on the front and middle parts of the brain. Anterior cranial fossa approaches benefit a lot from this position. It allows for direct access to the frontal lobe and nearby structures.
Anterior Cranial Fossa Approaches
Surgeons often use the supine position to reach tumors or lesions in the front part of the brain. This approach helps use minimally invasive techniques and lowers the risk of problems.
Middle Cranial Fossa Access
For surgeries on the middle part of the brain, the supine position with a slight head turn is used. This method lets surgeons reach important structures like the trigeminal nerve.
Advantages for Anterior and Midline Approaches
The supine position has many benefits for surgeries on the front and middle parts of the brain. It ensures hemodynamic stability and better airway management. These advantages make the surgery safer.
Hemodynamic Stability Benefits
Keeping blood pressure stable is key during brain surgeries. The supine position helps keep blood pressure steady, reducing the chance of problems during the surgery.
Airway Management Advantages
Managing the airway is easier in the supine position. Anesthesiologists can secure the airway and manage breathing well during the surgery.
Modifications and Variations of the Supine Position
To meet different surgical needs, the supine position can be changed. Techniques like head rotation and elevation and shoulder roll placement are used.
Head Rotation and Elevation Techniques
Changing the head’s position can improve access during surgery. Head rotation helps reach structures on the sides, while elevation can reduce bleeding from veins.
Shoulder Roll Placement Strategies
Placing a shoulder roll under the patient’s shoulders can improve cervical exposure. It also lowers the risk of position-related injuries.
| Positioning Technique | Benefits | Applications |
| Head Rotation | Improved lateral access | Middle cranial fossa surgery |
| Head Elevation | Reduced venous bleeding | Anterior cranial fossa surgery |
| Shoulder Roll | Enhanced cervical exposure | Various neurosurgical procedures |
Prone Position: Essential for Posterior Fossa Access
Neurosurgery in the posterior fossa needs the prone position. This setup is key for surgeries in this area. It gives surgeons the best access to this complex region.
Technical Setup and Patient Preparation
Setting up the prone position is detailed. It involves specialized frame and support systems. These systems keep the patient stable and reduce pressure points.
Frame and Support Systems
Frames and support systems are vital. They spread the patient’s weight evenly. This lowers the risk of sores and nerve damage.
Patient Transfer Protocols
Safe transfer protocols are key for the prone position. The surgical team works together. They move the patient safely and quickly.
Physiological Challenges and Management
The prone position has its challenges. Risks include abdominal compression and facial pressure. Effective management strategies are needed to address these risks.
Abdominal Compression Mitigation
Teams use various methods to avoid abdominal compression. They adjust support systems for better abdominal movement.
Facial Pressure Point Protection
Protecting facial points is critical. Careful padding and positioning prevent injuries.
Optimal Procedures for Prone Positioning
The prone position is great for posterior fossa tumor resections and spinal cord interventions. It offers the best access for these procedures.
Posterior Fossa Tumor Resections
In tumor resections, the prone position is essential. It allows for precise access to the delicate area.
Spinal Cord Interventions
For spinal cord procedures, the prone position is ideal. It provides a stable environment for complex surgeries.
Lateral Positions: Techniques and Applications
Neurosurgeons often use lateral positions for cranial procedures. These positions offer flexibility and access to the brain. They are key in neurosurgery.
Park Bench Position Methodology
The park bench position is used for surgeries on the cerebellum and posterior fossa. It provides great exposure and reduces risks.
Arm and Shoulder Placement
Correct arm and shoulder placement is vital in the park bench position. The arm on the bottom is supported to avoid injury.
Head Fixation Techniques
Head fixation in the park bench position secures the head for surgery. It uses specialized systems to keep the head steady and safe.
Lateral Decubitus Configuration
The lateral decubitus configuration places the patient on their side. It’s great for surgeries on the brain’s lateral aspects.
Body Alignment Principles
Proper body alignment is key in the lateral decubitus position. It prevents strain and ensures good surgical access.
Support System Requirements
Support systems are needed to keep the patient comfortable and in position. Pillows, straps, and other devices are used.
Temporal and Parietal Lobe Access Optimization
Lateral positions are best for the temporal and parietal lobes. The approach is tailored for better exposure and less brain retraction.
Approach Angles and Considerations
The approach angle is critical in lateral positioning. Surgeons must think about the lesion’s location, the patient’s anatomy, and the surgical path.
Surgical Corridor Enhancement
Improving the surgical corridor is essential for success. It involves planning and executing the approach for better exposure and less tissue damage.
| Lateral Position | Key Features | Applications |
| Park Bench Position | Arm and shoulder support, head fixation | Cerebellum and posterior fossa surgeries |
| Lateral Decubitus Configuration | Body alignment, support systems | Lateral aspect brain surgeries |
Sitting Position: Controversies and Considerations
The sitting position is a valuable technique in some neurosurgical cases. It’s used for specific procedures, bringing benefits but also challenges.
Air Embolism Risks and Prevention Strategies
The sitting position raises the risk of air embolism, a serious issue. Prevention strategies are key. They include choosing the right patients, precise surgical methods, and using precordial Doppler monitoring to spot air in veins.
Detection Methods and Monitoring
Tools like precordial Doppler, transesophageal echocardiography, and end-tidal CO2 monitoring are vital. They help find air embolism early, allowing quick action.
Emergency Management Protocols
When an air embolism happens, emergency management protocols kick in. This includes alerting the surgical team, removing air through central venous catheters, and supporting blood flow.
Hemodynamic Challenges in Upright Positioning
The sitting position brings hemodynamic challenges like low blood pressure and reduced venous return. Managing these needs careful blood pressure management and keeping cerebral perfusion up.
Modern Applications and Safety Protocols
Today, the sitting position is used in posterior fossa procedures, where it has benefits. Patient selection criteria are key to reduce risks. This involves a detailed preoperative check and considering each patient’s unique factors.
Surgical Approach Optimization for Complex Cranial Procedures
To improve surgical outcomes for complex cranial procedures, understanding positioning strategies is key. Neurosurgeons need this knowledge to succeed in detailed surgeries.
Skull Base Surgery Positioning Strategies
Skull base surgery needs precise positioning to reach complex areas. The right approach depends on the specific surgery needed.
Petroclival Approach Positioning
The petroclival approach requires careful positioning to access the petroclival region. Careful patient positioning is vital to prevent complications.
Orbital and Parasellar Region Access
Accessing the orbital and parasellar regions needs precise positioning. Advanced imaging helps navigate complex anatomy.
Vascular Neurosurgery Approach Considerations
Vascular neurosurgery involves delicate procedures. Optimal positioning is essential for success.
Aneurysm Clipping Position Requirements
Aneurysm clipping requires strategic positioning to safely access the aneurysm. The chosen position must allow for clear visualization and manipulation.
AVM Resection Approach Optimization
AVM resection needs careful planning and positioning. This ensures complete removal with minimal risk.
| Procedure | Positioning Requirement | Key Considerations |
| Petroclival Approach | Lateral or supine with head rotation | Avoiding excessive head rotation |
| Aneurysm Clipping | Supine or park bench | Optimal visualization of the aneurysm |
| AVM Resection | Prone or lateral | Access to the AVM nidus |
Tumor Resection Positioning Techniques
Tumor resection positioning varies based on the tumor’s location and the surgical approach.
Deep-Seated Lesion Access
Accessing deep-seated lesions requires meticulous planning and precise positioning. This ensures safe removal.
Ventricular Tumor Approach Strategies
Ventricular tumor approaches need careful positioning to access the ventricular system. The position must allow for optimal visualization and tumor removal.
Patient Safety Protocols in Neurosurgical Positioning
Neurosurgical positioning needs careful attention to ensure patient safety. The right position is key for successful neurosurgical procedures. It directly affects patient outcomes. Good patient safety protocols cover many areas of neurosurgical positioning.
Pressure Point Protection Methodologies
Protecting pressure points is vital in neurosurgical positioning. It requires understanding the patient’s anatomy and using the right support materials.
Padding and Support Materials
Padding and support materials are key for even pressure distribution and avoiding tissue damage. Gel pads, foam padding, and inflatable pillows are often used.
Pressure Redistribution Techniques
Pressure redistribution techniques involve changing the patient’s position to avoid pressure on sensitive areas. This can be done with automated systems or manual adjustments by the surgical team.
Peripheral Nerve Injury Prevention
Preventing peripheral nerve injury is critical in patient safety protocols for neurosurgical positioning. Nerve injuries from improper positioning can cause serious harm.
Ulnar and Brachial Plexus Protection
The ulnar nerve and brachial plexus are at high risk of injury. Proper arm positioning and using supportive devices can reduce this risk.
Lower Extremity Nerve Safeguarding
Lower extremity nerves are also at risk during neurosurgical procedures. Proper leg and foot positioning, along with padding, can prevent nerve damage.
Positioning-Related Complication Management
Despite efforts, positioning-related complications can happen. It’s important to have effective management strategies to lessen their impact.
Early Detection Strategies
Early detection of positioning-related complications is key. This means constant monitoring of the patient’s status and making necessary position adjustments.
Intraoperative Position Adjustments
The ability to make intraoperative position adjustments is essential for responding to patient condition changes. This requires teamwork from the surgical team.
Physiological Considerations During Prolonged Procedure
Prolonged neurosurgical procedures need careful attention to keep patients safe and healthy. These complex operations face many physiological challenges. Understanding these challenges is key to success.
Cardiovascular System Support Strategies
Keeping the heart stable is vital during long neurosurgery. It’s important to improve blood flow and keep the heart pumping well.
Venous Return Optimization
To improve blood flow, patients should be positioned correctly. Leg elevation is also helpful.
Cardiac Output Maintenance
Keeping the heart pumping right involves managing fluids and watching the patient’s blood pressure.
Respiratory Function Optimization
Respiratory health is critical during long surgeries. Adjusting breathing settings and managing lung function are key.
Ventilation Parameter Adjustments
Adjusting breathing settings means changing the rate and volume of breaths to fit the patient’s needs.
Pulmonary Compliance Management
Managing lung function means watching how the patient breathes and making changes as needed.
Intracranial Pressure Management Techniques
Keeping the brain pressure in check is essential during neurosurgery. Techniques include raising the head and draining cerebrospinal fluid.
Head Elevation Effects
Raising the head of the bed can lower brain pressure by helping blood flow better.
CSF Drainage Considerations
Draining cerebrospinal fluid is a key strategy for managing high brain pressure, important during long surgeries.
Specialized Equipment for Optimal Neurosurgical Positioning
Specialized equipment is key for the best neurosurgical positioning. The safety and precision of these surgeries depend on it.
Head Fixation Systems and Applications
Head fixation systems keep the patient’s head stable during surgery. The Mayfield clamp and the horseshoe headrest are two main types.
Mayfield Clamp Techniques
The Mayfield clamp gives strong fixation for precise head control. It’s great for surgeries needing detailed cranial access.
Horseshoe Headrest Applications
The horseshoe headrest is a flexible option. It supports the head without being too rigid. It’s best for less invasive surgeries.
Body Support Devices and Frameworks
Body support devices are also vital for the right patient position. The Wilson frame and gel positioning systems are examples.
Wilson Frame Utilization
The Wilson frame supports the body, making adjustments for better surgical access.
Gel Positioning Systems
Gel systems offer cushioning and support. They help prevent pressure injuries during long surgeries.
Technological Advancements in Positioning Equipment
New tech has greatly improved neurosurgical positioning. Computer-assisted systems and pressure monitoring lead these advancements.
Computer-Assisted Positioning Systems
These systems offer precise adjustments. They improve the accuracy of neurosurgical procedures.
Pressure Monitoring Technologies
These technologies detect and prevent pressure injuries early. They make surgeries safer for patients.
As neurosurgery grows, so does the need for better equipment. This is key for better outcomes and care for patients.
Intraoperative Neurophysiological Monitoring Considerations
Intraoperative neurophysiological monitoring has changed neurosurgery. It gives real-time feedback on how well nerves are working.
Electrode Placement and Positioning Compatibility
Getting electrodes in the right spot is key for good monitoring. SSEP (Somatosensory Evoked Potentials) monitoring setup uses scalp and limb electrodes. This checks the sensory pathways.
SSEP Monitoring Setup
SSEP checks if sensory pathways are okay during surgery. It stimulates nerves and records responses from the scalp.
Motor Evoked Potentials Recording
Motor evoked potentials (MEPs) record how muscles react to brain signals. This monitors motor pathways during surgery.
Monitoring Strategies for Different Surgical Positions
Each surgical position has its own monitoring challenges. Prone position monitoring challenges include keeping electrodes in place and signal quality.
Prone Position Monitoring Challenges
In the prone position, electrodes must be placed securely. This prevents them from moving during surgery.
Sitting Position Signal Acquisition
The sitting position needs careful electrode placement and signal techniques. This ensures top-quality recordings.
Position-Related Signal Changes and Interpretation
It’s vital to understand signal changes related to position. Baseline alterations with position changes can happen. This is due to how the patient is positioned and the anesthesia used.
Baseline Alterations with Position Changes
Position changes can alter signal baselines. It’s important to know these changes from surgical effects.
Distinguishing Positioning vs. Surgical Effects
It’s important to tell apart signal changes from positioning and those from surgery. Accurate interpretation is key.
Minimally Invasive Neurosurgery Positioning Techniques
Minimally invasive neurosurgery needs precise positioning for complex procedures. This method is key in modern neurosurgery. It helps reduce recovery time and tissue damage.
Endoscopic Procedure Positioning Requirements
Endoscopic neurosurgery needs exact positioning for clear views and access. Two main methods are used:
Endonasal Approach Positioning
The endonasal approach uses the nasal passage to reach the cranial base. The head and neck are adjusted carefully for the endoscope’s path.
Intraventricular Endoscopy Setup
Intraventricular procedures position the head for ventricular system access. The neck may be flexed or extended, depending on the procedure.
Stereotactic Surgery Approach Optimization
Stereotactic surgery uses frames or frameless navigation for precise location. Positioning is key for accuracy.
Frame-Based Stereotaxy Positioning
Frame-based stereotaxy fixes the head rigidly for precise alignment with the frame.
Frameless Navigation Considerations
Frameless navigation systems need precise patient anatomy registration for accurate localization. Positioning must match the navigation system’s needs.
Robotic-Assisted Neurosurgery Positioning Considerations
Robotic-assisted neurosurgery offers precision and dexterity. Positioning is critical for the robot’s optimal workspace.
Robot-Patient Registration Optimization
Aligning the robot with the patient is essential for accurate robotic assistance.
Workspace Configuration Requirements
The workspace must allow robotic arm movement without risking patient safety.
| Technique | Positioning Requirements | Key Considerations |
| Endoscopic | Precise head and neck positioning | Optimal visualization and access |
| Stereotactic | Rigid head fixation or precise registration | Accuracy and compatibility with navigation system |
| Robotic-Assisted | Optimized workspace configuration | Unobstructed robotic arm movement and patient safety |
Pediatric and Geriatric Neurosurgical Positioning Adaptations
Neurosurgery for kids and older adults needs a deep understanding of their unique needs. These patients have special requirements for the best surgical results.
Age-Specific Anatomical Considerations
The body shapes of kids and older adults affect how they are positioned for surgery. Kids have bigger heads compared to their bodies.
Pediatric Head-to-Body Proportions
Kids have bigger heads compared to their bodies, which changes how they are positioned for surgery. Specialized equipment and methods are needed for these kids.
Older adults, on the other hand, have bones that are more fragile.
Geriatric Skeletal Fragility Management
Older adults need to be handled carefully to avoid injuries during positioning. Supportive devices and gentle handling are key.
Physiological Vulnerabilities and Mitigation Strategies
Both kids and older adults face special challenges during neurosurgery.
Thermoregulation in Pediatric Patients
Kids are more at risk of getting too cold because of their body size. Keeping them warm is very important.
Cardiovascular Compensation in Elderly
Older adults have weaker hearts, making them more likely to have problems during surgery. They need close monitoring and careful fluid management.
Special Equipment Modifications for Extreme Age Groups
Special equipment is often needed for kids and older adults during neurosurgery.
Pediatric Head Fixation Alternatives
Because of their soft skulls, kids need special ways to keep their heads stable during surgery. Soft padding and careful setup are used.
Pressure Distribution for Osteoporotic Patients
Patients with weak bones need special care to avoid sores and breaks. Special mattresses and padding help spread out pressure.
Conclusion: Optimizing Neurosurgical Outcomes Through Proper Positioning
Proper positioning is key for the best neurosurgical results. Different positions, like supine and prone, have their own benefits and challenges. Making the right surgical approach is vital for patient success.
Neurosurgeons can improve care by focusing on the right positioning. Using special tools helps keep patients safe and comfortable. This focus on positioning leads to fewer complications and better care.
The success of neurosurgery depends on careful planning of positioning. By focusing on the right positioning and surgical approach, neurosurgeons can improve patient outcomes. This leads to better care for everyone.
FAQ
What is the most common position used in neurosurgical procedures?
The most common position in neurosurgery is the supine position. It’s versatile and easy to access for many surgeries.
How has neurosurgical positioning evolved over time?
Neurosurgical positioning has changed a lot. New technology, better understanding of the body, and improved surgery techniques have all played a part. These changes aim to make surgeries safer and more effective.
What are the key considerations for patient positioning in neurosurgery?
Important factors include making sure the body is aligned right, the surgery area is easy to reach, and the patient’s blood flow is stable. It’s also key to protect nerves and avoid pressure points to keep the patient safe.
What are the advantages of the supine position in neurosurgery?
The supine position is great for reaching the front and middle parts of the brain. It’s also easier to manage anesthesia and has fewer risks compared to other positions.
How is the prone position utilized in neurosurgery?
The prone position is used to access the back of the brain. It requires careful setup and preparation. Managing the patient’s body and blood flow is also important.
What are the challenges associated with the sitting position in neurosurgery?
The sitting position can be risky, like causing air bubbles in the blood or unstable blood flow. It’s only used when absolutely necessary and with strict safety measures.
How can surgical approach optimization improve outcomes in complex cranial procedures?
By choosing the right approach and positioning, surgeons can do more precise work. This can lead to fewer complications and better results for patients with complex brain surgeries.
What patient safety protocols are critical in neurosurgical positioning?
Safety is key, including protecting nerves and avoiding pressure points. These steps help prevent injuries and complications during surgery.
How do physiological considerations impact prolonged neurosurgical procedures?
Keeping the patient stable is vital during long surgeries. This includes supporting the heart and lungs and managing pressure in the brain.
What role does specialized equipment play in neurosurgical positioning?
Special tools, like head holders and body supports, are essential. They help keep the patient in the right position during surgery.
How does intraoperative neurophysiological monitoring impact neurosurgical positioning?
Monitoring the brain during surgery is critical. It requires careful placement of sensors and understanding the signals they send. This helps surgeons make precise decisions during the operation.
What are the unique considerations for minimally invasive neurosurgery positioning?
For small, less invasive surgeries, precise positioning is needed. This includes using endoscopes and robots. It’s all about getting the best view and control.
How do pediatric and geriatric populations require adapted neurosurgical positioning?
Young and older patients need special care. Their bodies are different, and they may be more vulnerable. So, the positioning must be tailored to their needs.
What is the significance of surgical ergonomic considerations in neurosurgical positioning?
Ergonomics is important for the surgeon’s comfort and the patient’s safety. It helps reduce fatigue and improves precision, leading to better outcomes.
How does neurological monitoring strategies contribute to effective neurosurgical positioning?
Monitoring the brain during surgery is essential. It helps catch any changes quickly. This allows for fast action to prevent problems.
What is the impact of intracranial pressure control on neurosurgical outcomes?
Managing brain pressure is critical. Uncontrolled pressure can cause serious issues, like brain swelling and even death. It’s a key factor in successful surgery.
How does minimally invasive positioning affect patient recovery?
Less invasive techniques can reduce damage to tissues. This means less pain and a faster recovery for the patient.