Last Updated on December 1, 2025 by Bilal Hasdemir

Neurosurgery is a delicate field with high risks. It worries both patients and doctors. The surgical procedures and the patient’s neurological condition are key to the success of these operations. Is neurosurgery a high-risk surgery? Get the essential facts on neurosurgery operation risk and discover the critical factors that determine success.
Dealing with neurosurgery requires advanced medical skills. The complexity of the surgical procedure means doctors need special training. This highlights the importance of careful patient care and management.
Key Takeaways
- Neurosurgical procedures are complex and carry significant risks.
- The patient’s neurological condition affects the surgical outcome.
- Advanced medical intervention is critical in neurosurgery.
- Specialized expertise is needed for neurosurgical procedures.
- Careful patient care and management are essential.
Understanding Neurosurgery: Definition and Scope
Neurosurgery is a very specialized field. It deals with surgeries for the brain, spinal cord, and nerves. It needs a deep knowledge of how the nervous system works.
What Constitutes Neurosurgical Procedures
Neurosurgical procedures are varied. They include surgeries on the brain, spinal cord, and nerves. These surgeries are key for treating many nervous system problems.
Brain and Spinal Cord Interventions
Brain and spinal cord surgeries are very complex. They involve delicate operations like removing tumors and fixing aneurysms. These surgeries need precise navigation and a deep understanding of the brain and spinal cord.
Peripheral nerve surgeries are also important in neurosurgery. They fix or relieve pressure on nerves to ease pain or improve function. Surgical complexity is high, as surgeons must be very careful around nerves and tissues.
Neurosurgery covers a wide range of procedures. They all need specialized training and skill. Knowing what neurosurgery is helps us understand the challenges of these surgeries.
Common Types of Neurosurgical Procedures
Neurosurgery uses many surgical techniques, like those for brain tumor resections and spine surgeries. These treatments are key for many brain and spinal disorders. They need a lot of precision and skill.
Brain Tumor Resections
Brain tumor resections aim to remove tumors in the brain. The surgery method changes based on the tumor type.
Benign vs. Malignant Tumor Approaches
It’s important to know if a tumor is benign or malignant. Benign tumors are less aggressive and might need less removal. Malignant tumors, being cancerous, often require more extensive surgery.
- Benign tumor surgeries aim to remove the tumor while keeping brain function intact.
- Malignant tumor surgeries might remove more tissue to get rid of all cancer cells.
Spine Surgeries
Spine surgeries treat different spinal issues, like disc herniation and the need for spinal fusion. These surgeries aim to ease pain, stabilize the spine, and improve function.
Disc Herniation and Spinal Fusion
Disc herniation happens when the spinal disc’s soft center leaks out, pressing on nerves and causing pain. Spinal fusion joins vertebrae together to stabilize the spine and reduce pain.
| Condition | Surgical Procedure | Goal |
| Disc Herniation | Discectomy | Relieve nerve compression |
| Spinal Instability | Spinal Fusion | Stabilize the spine |
These neurosurgical procedures show the complexity and variety of treatments for neurological issues. Knowing the different methods is vital for neurosurgeons and patients alike.
Inherent Challenges in Neurosurgery
Neurosurgery faces big challenges due to the brain and spinal cord’s complex nature. These areas have limited ability to heal themselves. Surgeons need to deeply understand the brain and spinal cord’s structures and how they work.
Anatomical Complexity of the Nervous System
The brain and spinal cord are full of critical structures and paths. These are key for controlling our movements, feelings, and thoughts.
Critical Structures and Pathways
When these areas get damaged during surgery, it can lead to serious problems. Neurosurgeons must be very precise to avoid harming these important parts. They use advanced tools and systems to help them.
Limited Regenerative Capacity
Neural tissue, like the brain and spinal cord, can’t heal well after injury. This is a big challenge for neurosurgeons.
Consequences of Neural Tissue Damage
Damage to neural tissue can cause lasting problems. Neural tissue damage can lead to issues with thinking, moving, and feeling. So, neurosurgeons must be very careful during surgery.
By knowing the challenges of neurosurgery, like the brain’s complexity and healing limits, surgeons can improve care for their patients.
Neurosurgery Operation Risk: A Detailed Look
Neurosurgery comes with many risks, changing with each procedure. These surgeries are lifesaving but carry risks that must be understood and managed well.
Mortality Statistics Across Procedure Types
Mortality rates in neurosurgery show the risks involved. These rates change based on the procedure, the patient’s health, and the surgeon’s skill.
High-Risk vs. Low-Risk Procedures
Neurosurgery procedures are split into high-risk and low-risk types. High-risk surgeries, like some brain tumor removals, have higher death rates. Low-risk surgeries, like some spine operations, have lower rates.
High-Risk vs. Low-Risk Procedures
- High-risk surgeries deal with complex areas and vital structures.
- Low-risk surgeries are complex but have simpler approaches.
Morbidity Considerations
Morbidity is a big worry in neurosurgery, too. It’s about complications and lasting damage from surgery.
Temporary vs. Permanent Deficits
Neurological problems from surgery can last or go away. Knowing this helps with patient consent and care after surgery.
- Temporary issues might get better with time and therapy.
- Permanent issues can greatly affect a patient’s life quality.
It’s key to carefully manage risks in neurosurgery. This means looking at the patient, the surgery, and the team’s skills.
Patient-Specific Risk Factors
Patient-specific risk factors are key in neurosurgery success and safety. Each person’s unique factors can greatly affect surgery results.
Age and General Health Assessment
A patient’s age and health are very important. Older patients or those with health issues might face more risks. This is because they have less physical strength and may have other health problems.
Pediatric vs. Geriatric Considerations
Pediatric and geriatric patients have different risks. Pediatric neurosurgery looks at the growing brain and long-term effects. Geriatric neurosurgery deals with managing health issues and less physical strength.
Pre-existing Neurological Conditions
Neurological conditions before surgery can make things harder. Conditions like epilepsy, multiple sclerosis, or previous strokes can change how surgery is planned and how risks are seen.
Impact on Surgical Planning
Neurosurgeons need to plan surgery carefully when there are pre-existing conditions. They must think about these conditions to lower risks and get better results.
Understanding and assessing these risk factors helps neurosurgeons plan better surgeries. This leads to better outcomes for patients.
Procedure-Specific Risk Considerations
Neurosurgery is complex and delicate. It requires a deep understanding of the risks involved. These risks vary based on the type of surgery and where it’s done.
Emergency vs. Elective Neurosurgery
Emergency and elective neurosurgery have different risks. Emergency surgeries are urgent and can be riskier because of the time pressure.
Time Constraints and Decision-Making
Emergency surgeries have less time for planning. This can raise the risk of problems. On the other hand, elective surgeries have more time for planning, which lowers the risk.
Location and Accessibility of Target Areas
The location of the target area affects the risk. Areas that are hard to reach or in eloquent brain regions are riskier.
Eloquent vs. Non-Eloquent Brain Regions
Surgeries in areas that control important functions like speech and movement are riskier. These areas are called eloquent brain regions. Surgeries in other areas are generally safer.
| Procedure Type | Risk Factors | Potential Complications |
| Emergency Neurosurgery | Time constraints, urgency | Increased risk of bleeding, infection |
| Elective Neurosurgery | Preoperative planning, patient optimization | Lower risk of immediate complications |
| Surgery in Eloquent Brain Regions | Location, functional importance | Neurological deficits, speech or motor issues |
Understanding these risks helps neurosurgeons and patients. It leads to better outcomes in neurosurgery.
Common Complications in Neurosurgical Procedures
Neurosurgical procedures are complex and can lead to various complications. These risks can affect how well a patient does after surgery. It’s important to manage these complications carefully.
Hemorrhage and Bleeding Disorders
Hemorrhage is a big risk in neurosurgery and can cause serious problems. If a patient has bleeding disorders, it makes surgery even riskier. Doctors need to check patients carefully before surgery.
Management and Prevention Strategies
To manage hemorrhage, surgeons use special techniques and hemostatic agents. They also keep an eye on patients after surgery. To prevent problems, doctors choose patients carefully and manage blood pressure during surgery.
| Complication | Management Strategy | Prevention Strategy |
| Hemorrhage | Meticulous surgical technique, use of hemostatic agents | Careful patient selection, optimization of coagulation profiles |
| Bleeding Disorders | Preoperative assessment, correction of coagulopathy | Avoidance of anticoagulant medications preoperatively |
Infection Risks and Surgical Complication Prevention
Infections are a big worry after neurosurgery. They can cause meningitis or wound infections. These can make patients stay in the hospital longer and affect their recovery.
Meningitis and Wound Infections
Meningitis is an inflammation of the brain and spinal cord membranes. It can happen after surgery. Wound infections are also common and need quick treatment.
Prevention measures include using antibiotics, keeping the surgery area clean, and taking care of the wound after surgery. Watching for infection signs and acting fast is key to managing these issues.
It’s vital to understand and reduce these complications to improve neurosurgery results. By using careful management and prevention, we can lower the risk of problems.
Comparing Neurosurgery Risks to Other Surgical Specialties
Looking at the risks of neurosurgery compared to other surgeries can give us important insights. Neurosurgery deals with the brain and spine, making it very risky. It’s different from other surgeries because of this.
Risk Profiles Across Different Surgical Procedures
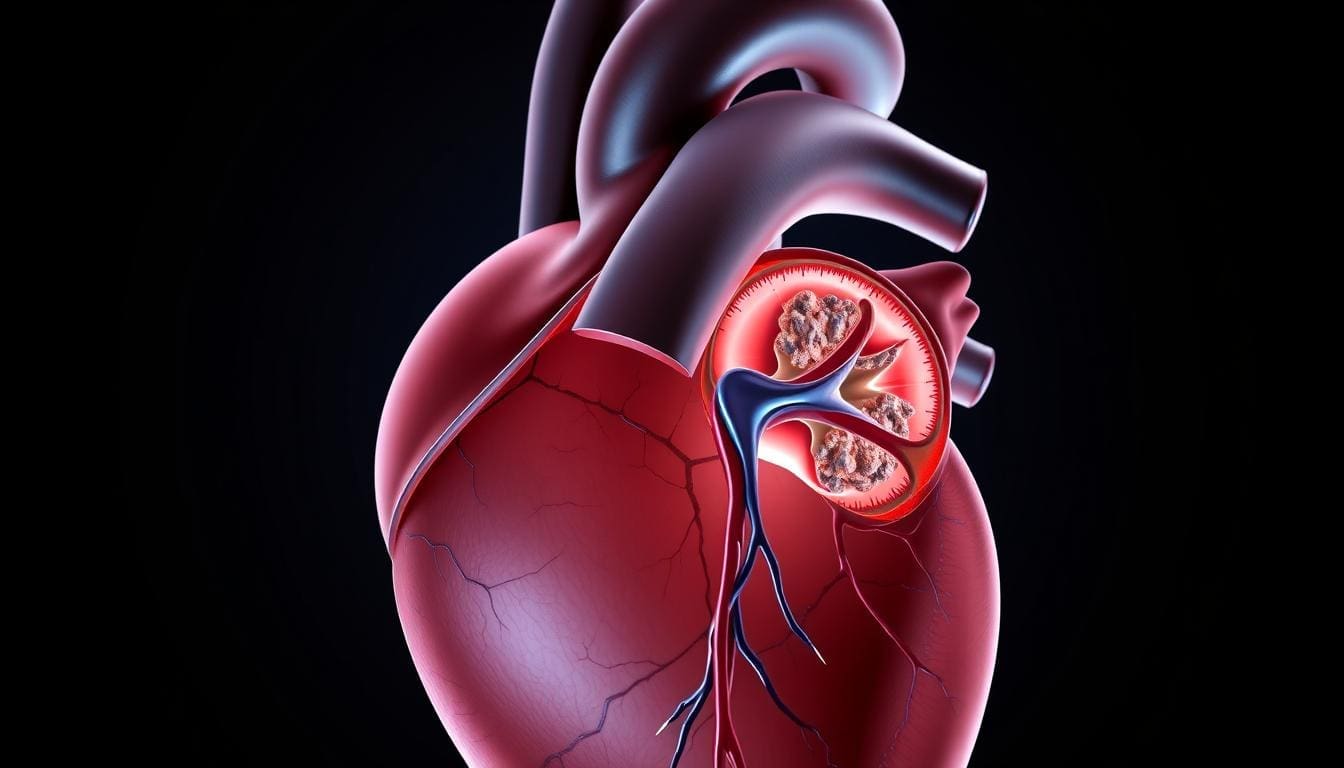
Each surgical field has its own set of risks. For example, cardiac surgery is also high-risk because it involves important organs. But, neurosurgery is even riskier because of the brain’s complexity.
Cardiac surgery and neurosurgery both deal with vital organs. But, the brain’s complexity makes neurosurgery more unpredictable. Cardiac surgery has more set protocols, leading to more predictable results.
Unique Aspects of Neurosurgical Procedural Risks
Neurosurgery is very risky because of the nervous system’s delicacy. Mistakes can lead to serious problems or even death.
Consequences of Adverse Events
Adverse events in neurosurgery can cause long-term brain damage. This highlights the importance of careful planning and precise surgery to avoid these risks.
Understanding neurosurgery’s risks helps doctors improve patient care. This way, they can reduce risks and get better results for their patients.
Technological Advancements Reducing Neurosurgical Risks
Neurosurgery has seen big changes thanks to new technology. This has made surgeries safer and more effective. Before, neurosurgery was very risky because of the brain’s complexity.
Advanced Diagnostic Techniques and Navigation Systems
New tools have changed neurosurgery a lot. They let surgeons see the brain and spine clearly. This helps them plan and do surgeries more accurately.
Intraoperative MRI and CT
Real-time imaging during surgery is now possible. This lets surgeons check their work and make changes. It’s very helpful for removing tumors safely.
Innovative Surgical Techniques and Minimally Invasive Approaches
New surgical methods and small incisions have made things better. These approaches cause less damage and help patients recover faster.
Endoscopic and Keyhole Procedures
Endoscopic and keyhole surgeries are becoming more common. They use small cuts and special tools. This way, surgeons can do complex jobs with less harm to the patient.
| Technological Advancement | Description | Benefits |
| Intraoperative MRI and CT | Real-time imaging during surgery | Enhanced precision, ability to make adjustments during surgery |
| Endoscopic and Keyhole Procedures | Minimally invasive techniques for complex operations | Less tissue damage, quicker recovery, reduced risk of complications |
These new technologies have greatly reduced risks in neurosurgery. They have also improved patient results and opened up new ways to treat brain problems.
The Role of Neurosurgical Expertise Evaluation
Checking a neurosurgeon’s skills is key to finding the right treatment and lowering risks. The surgeon’s experience and the number of surgeries done at a place greatly affect how well a patient does.
Volume-Outcome Relationship
Many studies have looked into how many surgeries a place does and how well patients do. It shows that places that do a lot of surgeries have better results. This is because the team there has more experience and uses better methods.
High-Volume Centers and Outcomes
Places that do a lot of surgeries have better results, fewer problems, and lower death rates. This is because the team there is more skilled and follows strict rules.
| Center Type | Complication Rate | Mortality Rate |
| High-Volume | Lower | Lower |
| Low-Volume | Higher | Higher |
Subspecialty Expertise
Having special skills in neurosurgery is very important for tricky cases. Neurosurgeons with extra training in areas like kids’ brain surgery or brain tumors are more skilled.
Fellowship Training Impact
Fellowship programs give neurosurgeons more training in certain areas. This makes them better at handling hard cases. It also means better results for patients.
It’s very important to check a neurosurgeon’s skills. Knowing what makes a surgery successful helps patients and doctors make better choices.
Preoperative Risk Assessment and Patient Medical Optimization
Effective preoperative risk assessment and patient medical optimization are key to reducing complications in neurosurgery. Neurosurgery is a high-risk field. It requires careful preoperative evaluation for the best outcomes.
Comprehensive Health Assessment Protocols
A thorough health assessment is essential to identify risks in neurosurgery. It checks the patient’s overall health status.
Cardiovascular and Pulmonary Evaluation
Cardiovascular and pulmonary evaluations are critical in the health assessment. They help find any conditions that could make surgery or recovery harder.
| Evaluation Type | Purpose | Potential Findings |
| Cardiovascular Evaluation | Assess heart health and function | Hypertension, heart disease |
| Pulmonary Evaluation | Assess lung function and health | Chronic obstructive pulmonary disease (COPD), asthma |
Advanced Treatment Planning and Risk Reduction Strategies
After identifying risks, advanced treatment planning is used to lower these risks. This includes making the patient’s medical condition better before surgery.
Medication Management
Medication management is vital in preoperative optimization. It involves changing medications that could affect surgery or increase complications.
By managing medications and improving the patient’s health, the risk of complications can be greatly reduced. This detailed approach to preoperative risk assessment and patient medical optimization is critical for successful neurosurgery outcomes.
Recovery and Rehabilitation After Neurosurgery
The journey to full recovery after neurosurgery is complex. It involves immediate care and long-term rehabilitation. Both are key for the best recovery.
Immediate Post-Operative Care and Patient Recovery Protocols
Right after surgery, care is critical to avoid problems and ensure a smooth recovery. This phase is closely watched in a specialized neuro-ICU setting.
Neuro-ICU Management
In the neuro-ICU, vital signs and brain health are closely monitored. This is to catch and prevent issues like bleeding or infection. Advanced tools and tests are used here.
The complexity of neurosurgical procedures demands a highly specialized and attentive care environment, precisely in the immediate postoperative period.
Long-Term Recovery Considerations
Recovery over time focuses on getting the patient back to normal. It aims to improve their function and quality of life.
Timeline and Milestones
Recovery times vary based on the surgery and the patient’s health. Most see big improvements in the first few months.
| Recovery Phase | Timeline | Milestones |
| Immediate Recovery | 0-2 weeks | Stabilization of vital signs, wound healing |
| Early Rehabilitation | 2-6 weeks | Improvement in mobility, reduction in pain |
| Advanced Rehabilitation | 6 weeks-6 months | Significant improvement in functional abilities |
Rehab plans are made for each patient. They often involve a team of healthcare experts.
Making Informed Decisions About Neurosurgical Treatment
For patients getting neurosurgery, making informed choices is vital. They need to understand the risks and benefits well. This helps them choose what’s best for their health and values.
Surgical Outcome Prediction and Risk-Benefit Analysis
Knowing what neurosurgery might do is important. Surgical outcome prediction looks at how well treatment might work and possible problems. A good risk-benefit analysis helps everyone see the good and bad sides.
Quality of Life Considerations
Thinking about how surgery affects life is key. Patients should think about how it might change their daily life. This includes how it might affect their body and mind.
The goal of neurosurgery is not just to save lives, but to improve the quality of life for patients.
Second Opinion Considerations
Getting a second opinion can offer new views and peace of mind. It’s a big step for those wanting to check all their options. It ensures they’re making the right choice for them.
When to Seek Additional Consultation
If you’re not sure about your diagnosis, treatment, or what might happen, get a second opinion. It can clear up any confusion. It gives a deeper look at your options for neurosurgery.
Conclusion
Neurosurgery is a complex field that requires specialized skills and careful management. The delicate nature of the nervous system makes precise risk assessment and patient care essential.
In this article, we’ve looked at the challenges and risks in neurosurgery. We’ve also talked about the importance of technology and surgical expertise. Effective risk management and patient-centered care are key to better outcomes.
Understanding the risks of neurosurgery helps patients and doctors make better choices. The role of specialized skills, thorough health checks, and detailed treatment plans is vital. These steps help ensure the best results for neurosurgery patients.
The main goal of neurosurgery is to help patients with severe conditions while keeping risks low. By using the latest technology and focusing on the patient, neurosurgery can greatly improve lives. It makes a big difference in the quality of life for those undergoing these complex surgeries.
FAQ
What are the risks associated with neurosurgery?
Neurosurgery comes with risks like death, injury, and possible long-term brain or spinal cord problems. This is because brain and spinal cord surgeries are very delicate and complex.
How complex are neurosurgical procedures?
Neurosurgery is very complex. It needs a lot of training and skill because of the brain’s detailed structure and the limited ability of nerve tissue to heal.
What are the common types of neurosurgical procedures?
Common surgeries include removing brain tumors, spine operations for issues like herniated discs, and surgeries on peripheral nerves. Each type has its own challenges.
How does a patient’s age and general health status affect neurosurgical outcomes?
A patient’s age and health greatly affect surgery results. Young and old patients face special challenges. Also, any existing brain or nerve problems can change how a surgery is planned and how risky it is.
What is the difference between emergency and elective neurosurgery?
Emergency surgeries are urgent and riskier. Elective surgeries are planned and have fewer risks because they allow for better preparation.
How do advanced diagnostic techniques and navigation systems reduce neurosurgical risks?
New tools like MRI and CT scans and navigation systems help surgeons be more precise. This reduces the chance of problems and helps plan treatments better.
What is the importance of neurosurgical expertise in determining outcomes?
The skill of the neurosurgeon, and the experience of the team, greatly affects how well a patient does. Specialized training is key for handling complex cases safely.
How can patients optimize their medical condition before neurosurgery?
Patients can prepare by getting a full health check, including heart and lung tests. This helps reduce risks during surgery.
What is the typical recovery process after neurosurgery?
Recovery starts with care in the neuro-ICU and includes long-term steps. Rehabilitation is very important for the best results.
How can patients make informed decisions about their neurosurgical treatment?
Patients should understand the risks and benefits of their treatment. Knowing what to expect and getting a second opinion helps them be part of their care plan.
What are the benefits of minimally invasive neurosurgical approaches?
New, less invasive methods like endoscopy cause less damage. This means less pain, shorter stays, and quicker recovery.
How do neurosurgical risks compare to other surgical specialties?
Neurosurgery is unique because of the brain’s complexity. It carries higher risks of serious problems, needing special care and management.
What is the role of patient-centered care in neurosurgery?
In neurosurgery, care that focuses on the patient is very important. It means treatments are tailored to each person’s needs and values, aiming for the best outcome and quality of life.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19645537/[1