
Neurosurgery is a complex medical procedure that needs careful planning and execution. Managing pain during the operation is a key aspect. The dura mater, a protective layer around the brain, is important for pain perception. Even though the brain doesn’t have pain receptors, the dura mater and other tissues can feel pain. The dura mater in brain is tough, but can you feel pain? Discover the amazing facts about why you don’t feel pain during brain surgery.
It’s important to understand what affects pain during neurosurgery for better pain management. The type of anesthesia used can greatly change how much pain you feel during the procedure.
Key Takeaways
- Pain management is critical during neurosurgery.
- The dura mater plays a significant role in pain perception.
- The brain lacks pain receptors, but surrounding tissues can detect pain.
- The type of anesthesia used affects pain experienced during neurosurgery.
- Effective pain management requires understanding factors that influence pain perception.
The brain’s protective layers and pain sensitivity
It’s important to know how the brain’s protective layers work to understand pain during neurosurgery. The brain has three layers called the meninges. These layers are key to the brain’s health and function.
The three meninges: Dura mater, arachnoid mater, and pia mater
The meninges have three layers: the dura mater, arachnoid mater, and pia mater. The dura mater is tough and fibrous, protecting the brain and spinal cord. The arachnoid mater is thinner and more delicate, with a space between it and the dura mater. The pia mater is the innermost layer, closely attached to the brain and spinal cord.
The detailed structure of these layers is vital for understanding their roles and pain sensitivity. Each layer has unique features that help protect and maintain the central nervous system.
Which parts of the brain and its coverings can feel pain
While the brain itself doesn’t have pain receptors, some parts of the meninges and surrounding areas can feel pain. The dura mater is very sensitive to pain, thanks to its nerve connections. This sensitivity is important in neurosurgery and for managing headaches and migraines.
Pain in the brain is complex, involving pain receptors and how the brain interprets signals. Knowing which parts of the brain and its coverings can feel pain is key to managing pain in neurosurgery and neurology.
The dura mater in brain: Anatomy and function
The dura mater is a thick membrane that wraps around the brain. It’s the outermost layer of the three meningeal layers that cover the brain and spinal cord. Knowing about its structure and role helps us see how it keeps the brain healthy.
Structure and location of the cranial dura mater
The cranial dura mater is a dense, fibrous membrane. It sticks closely to the inside of the skull. It has two parts: the periosteal layer, which is attached to the bone, and the meningeal layer, which touches the arachnoid mater. The space between these layers is called the epidural space. It’s filled with nerves and has a complex blood supply.
Key features of the cranial dura mater include:
- Attachment to the cranial bones
- Formation of dural folds and septa that support brain structures
- Presence of venous sinuses that drain blood from the brain
How the dura mater protects and supports the brain
The dura mater is key in protecting the brain in several ways:
| Mechanism | Description |
| Physical Protection | The dura mater acts as a barrier against mechanical injury, shielding the brain from external forces. |
| Support and Stabilization | Dural folds and septa help to stabilize brain structures, preventing excessive movement. |
| Venous Drainage | The venous sinuses within the dura mater facilitate the drainage of blood from the brain. |
In conclusion, the dura mater is essential for the brain’s protection and support. Its detailed structure and functions highlight its critical role in brain health.
Dura mater of spinal cord: Differences from cranial dura
The spinal dura mater is different from the cranial dura mater. Both protect the central nervous system. But, they have different features and roles.
Anatomical Features of Spinal Dura Mater
The spinal dura mater wraps around the spinal cord. It goes from the foramen magnum to the second sacral vertebra. It’s thicker and sticks less to bones than the cranial dura mater.
It’s surrounded by the epidural space. This space has fat, veins, and lymphatics.
Clinical Significance in Spinal Procedures
In spinal surgeries, knowing the spinal dura mater’s anatomy is key. Surgeons must be careful not to harm it. Tears can cause cerebrospinal fluid leaks and serious issues.
| Characteristics | Spinal Dura Mater | Cranial Dura Mater |
| Location | Surrounds the spinal cord | Surrounds the brain |
| Thickness | Thicker | Thinner in some areas |
| Adherence | Less adherent to surrounding bone | More adherent, specially to sutures |
The spinal and cranial dura mater are not just different in anatomy. They also have big clinical differences.Knowing these differences is key for good diagnosis and treatment.
The dura mater, whether around the brain or spinal cord, is vital for protecting the central nervous system. Its unique traits in each area must be respected during medical procedures.
Pain receptors in the brain: Myths and facts
Pain perception in the brain is complex and often misunderstood. The human brain is a detailed organ with a complex relationship with pain. A common myth is that the brain itself lacks pain receptors.
The Truth About “No Pain Receptors in Brain Tissue”
The statement that there are “no pain receptors in brain tissue” is mostly true. The brain’s functional tissue does not have pain receptors. This fact is important for some neurosurgical procedures.The brain itself is not sensitive to pain, which is why surgeons can perform operations on the brain while the patient is awake.But, this doesn’t mean patients don’t feel pain during brain surgery. The pain comes from other sources.
Pain-Sensitive Structures in and Around the Brain
While the brain tissue itself may not feel pain, structures around it are very sensitive. These include the meninges, blood vessels, and nerves. The dura mater, the outermost meningeal layer, is very sensitive to pain.
Irritation or inflammation of these structures can cause a lot of pain. This pain often shows up as headaches or migraines.
It’s important to understand the difference between the brain’s pain insensitivity and the sensitivity of structures around it. This knowledge helps neurosurgeons and patients manage pain better. It improves patient outcomes and comfort.
Why the dura mater is highly pain-sensitive
It’s important to know why the dura mater is so sensitive to pain. This thick membrane protects the brain and spinal cord. Its pain sensitivity is key in many neurological issues.
Innervation of the dura mater
The dura mater has many nerve fibers, making it very sensitive to pain. The trigeminal nerve covers the cranial dura mater, while spinal nerves cover the spinal dura mater. These nerves send pain signals, which we feel as headaches or migraines.
Nerve fibers in the dura mater can detect different kinds of stimuli. This complex setup is why irritation or inflammation here can cause a lot of pain.
Relationship between dura irritation and headaches/migraines
Irritation of the dura mater often leads to headaches and migraines. When it’s irritated, it can send pain signals. This can happen due to inflammation, infection, or mechanical stress.
| Condition | Effect on Dura Mater | Resulting Symptom |
| Inflammation | Irritation of nerve fibers | Headache or Migraine |
| Infection | Stimulation of pain receptors | Severe Headache |
| Mechanical Stress | Activation of pain-sensitive fibers | Migraine or Headache |
Understanding the link between dura mater irritation and headaches/migraines is vital. Knowing how to manage this pain can greatly improve life for those affected.
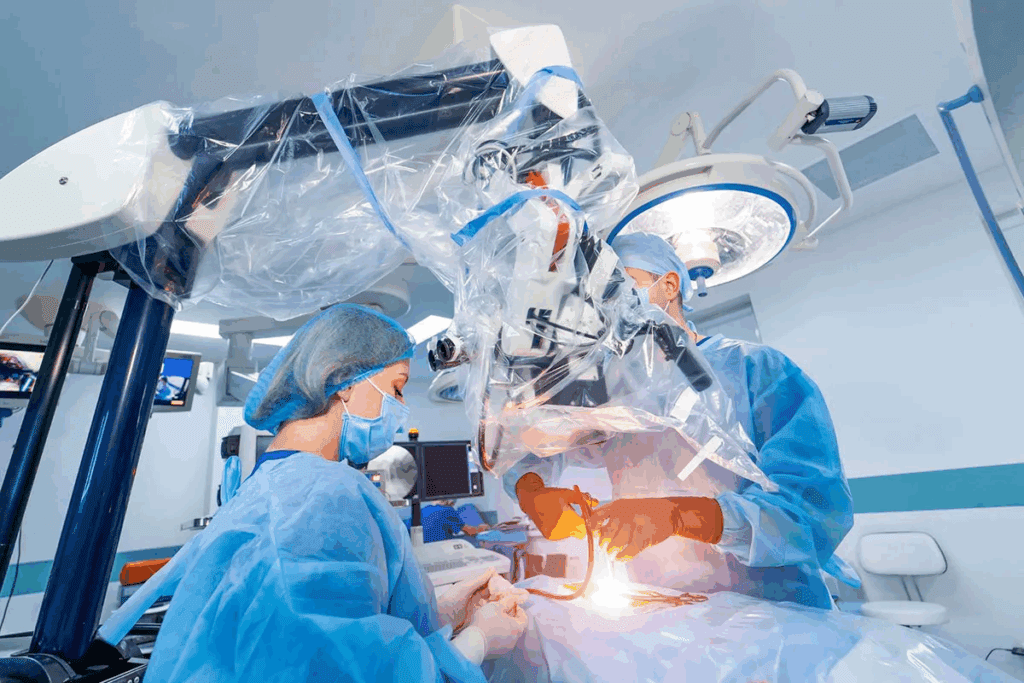
Anesthesia in neurosurgery: Preventing pain
Effective anesthesia is key to preventing pain in neurosurgery. It ensures patients don’t feel pain or discomfort during surgery. The choice of anesthesia depends on the surgery type, patient health, and the anesthesiologist’s expertise.
Types of Anesthesia Used for Brain and Spine Surgery
Several anesthesia types are used in neurosurgery. General anesthesia makes the patient completely unconscious, used for complex surgeries. Local anesthesia numbs a specific area, used for less invasive procedures or with general anesthesia. Conscious sedation relaxes the patient, allowing them to respond to commands or questions.
The right anesthesia choice depends on the surgery, patient history, and the surgical team’s preference.
| Type of Anesthesia | Description | Common Uses in Neurosurgery |
| General Anesthesia | Renders the patient unconscious | Complex or invasive brain and spine surgeries |
| Local Anesthesia | Numbs a specific area | Less invasive procedures, or used with general anesthesia |
| Conscious Sedation | Relaxes the patient, who remains able to respond | Procedures requiring patient response, such as awake craniotomies |
How Anesthesiologists Monitor and Manage Pain During Procedures
Anesthesiologists are vital in managing pain during neurosurgery. They watch the patient’s vital signs and adjust the anesthesia as needed. They use advanced monitoring like EEG and BIS to check the anesthesia depth and make precise adjustments.
Good pain management in neurosurgery improves patient outcomes and the surgical experience. By choosing and managing anesthesia well, anesthesiologists can greatly reduce pain and discomfort during and after surgery.
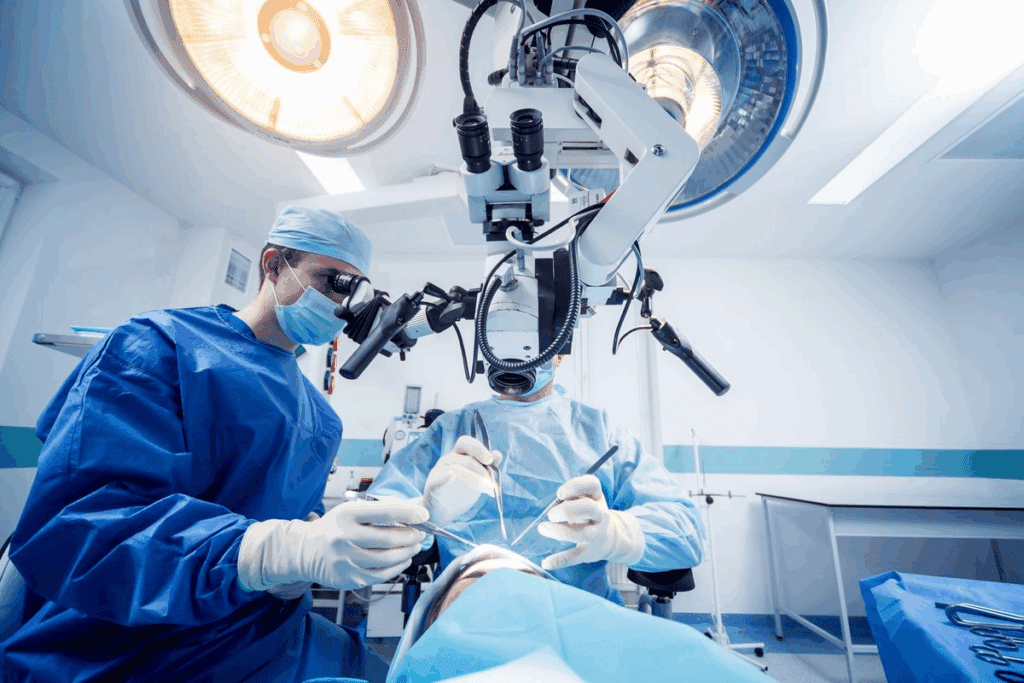
Awake craniotomy: Conscious during brain surgery
Awake craniotomy is a new way to do brain surgery. It lets patients stay awake while their brain is being operated on. This is great for surgeries near parts of the brain that control important things like talking, moving, and feeling.
By keeping patients awake, doctors can talk to them during surgery. This helps make sure these important functions stay safe.
Why Patients Remain Awake During Certain Brain Surgeries
Patients stay awake during some brain surgeries for a good reason. It lets doctors watch how the brain works in real time. This is very important when they’re near areas that control things like language or movement.
The awake craniotomy is used for things like tumors or epilepsy in important brain areas. It lets doctors know where to avoid during surgery, keeping vital parts safe.
Pain Management Techniques During Awake Neurosurgery
Managing pain is key during awake neurosurgery. Doctors use local anesthesia to numb the scalp and sedation to keep patients comfortable but awake.The secret to good pain management is getting ready mentally and using the right anesthesia. Doctors use scalp blocks and watch how patients feel to reduce pain. It’s also important to talk openly with patients about their feelings and worries. This helps make the surgery go smoothly.
Patient experiences during different neurosurgical procedures
Patients going through neurosurgery share many feelings during and after their surgeries. These feelings change a lot based on the surgery type, the patient’s health, and the surgical team’s methods.
What Patients Report Feeling During Various Types of Brain Surgery
Each neurosurgical procedure brings its own set of sensations. For example, those having an awake craniotomy might feel pressure or hear the doctors talking. On the other hand, patients under general anesthesia might feel pain or discomfort after the surgery.
Some patients feel numbness, tingling, or warmth during their procedures. These feelings depend on the brain area being worked on and the surgical techniques used.
Sensations Other Than Pain During Neurosurgery
Patients might feel more than just pain during neurosurgery. They might feel pressure, vibration, or even nausea. It’s important for the surgical team to watch these feelings closely to keep the patient comfortable.
New techniques and anesthesia methods have made surgeries better for patients. Knowing about these experiences helps improve neurosurgery care even more.
Brain tumor removal: Pain considerations
Removing a brain tumor is a complex surgery that needs careful pain management. The surgery’s complexity means we must plan for pain from the start to after the surgery.
It’s vital for the surgical team to manage pain well. This helps the patient feel better and ensures the surgery’s success. Pain considerations are key to the surgery’s outcome.
Approaches to Accessing and Removing Brain Tumors
Surgeons use different methods to reach and remove brain tumors. The method chosen depends on the tumor’s size, location, and the patient’s health.
- Craniotomy: This involves temporarily removing a part of the skull to access the tumor.
- Endoscopic surgery: This is a minimally invasive method using an endoscope to see and remove the tumor.
- Stereotactic surgery: A precise method using a three-dimensional system to locate and remove the tumor.
The surgical approach affects the pain management plan. Different methods can lead to different levels of pain after surgery.
Pain Management Strategies Specific to Tumor Resection
Managing pain during and after brain tumor removal is essential for patient comfort and recovery. Strategies include:
| Pain Management Technique | Description | Application |
| Preemptive analgesia | Administering pain relief before the surgical incision | Reduces postoperative pain |
| Multimodal analgesia | Using a combination of pain relief medications | Enhances pain control with fewer side effects |
| Regional anesthesia | Numbing specific regions of the body | Effective for managing pain during and after surgery |
Understanding brain tumor removal and using effective pain management can improve patient care. This leads to better outcomes and a higher quality of care.
Spine surgery and the dura mater
Protecting the spinal dura mater is key during spine surgery. This layer shields the spinal cord. Keeping it safe is vital to avoid problems.
The spinal dura mater is essential for protecting the spinal cord. Surgeons must be very careful not to harm this thin membrane.
Protecting the Spinal Dura During Procedures
Surgeons use special methods to keep the spinal dura mater safe. They use precise tools and keep a clear view to avoid dural tears.
Before surgery, doctors plan and use imaging to spot risks. This helps them prepare to avoid problems.
Complications Related to Dural Tears and CSF Leaks
Dural tears can cause CSF leaks. These leaks can lead to headaches, infections, or other brain issues. It’s important to fix dural tears quickly to stop these problems.
Fixing dural tears and CSF leaks involves careful surgery. Sometimes, doctors use grafts or sealants to help the dura mater stay closed.
In summary, handling the spinal dura mater during spine surgery needs a lot of care. This is to avoid issues like dural tears and CSF leaks. By focusing on keeping the dura mater intact, surgeons can help patients recover better and reduce risks after surgery.
Dura mater grafts and repairs in neurosurgery
Neurosurgeons use dura mater grafts and repairs in surgeries. The dura mater protects the brain and spinal cord. It’s important to fix it when damaged to avoid leaks and infections.
Materials and techniques for dural repair
There are many ways to repair the dura mater. The choice depends on the defect size and the patient’s health. Autologous grafts, taken from the patient, are the best choice because they’re safe and match the body.
Synthetic materials like DuraGen or Gore-Tex are also used. They’re easy to get and use. The right material and technique are key for a good seal and healing.
Recovery and possible complications after dural procedures
Recovery from dural repair varies based on the surgery and condition. Patients are watched for leaks, infections, or other issues. Care after surgery may include lowering pressure in the brain to help heal.
Complications like infections, leaks, and reactions to the graft can happen. It’s important to manage these to get a good outcome.
Post-operative pain after neurosurgery
Neurosurgery is lifesaving but often causes post-operative pain. This pain needs careful management. The complexity of these surgeries can lead to different pain sources during recovery.
Common sources of pain following brain and spine surgery
Patients may feel pain after neurosurgery for many reasons. Brain surgery pain can come from the incision, swelling, or irritation of the meninges. Spine surgery pain can result from the approach, bone grafting, or instrumentation.
Pain sources specific to brain surgery include headaches from swelling or irritation. For spine surgery, pain can come from muscle dissection, bone removal, or the fusion process.
Medications and techniques for managing post-surgical pain
Managing pain is key for patient comfort and recovery. Many medications and techniques are used for pain management after neurosurgery.
- Pharmacological interventions: Opioids, NSAIDs, and other analgesics are used to control pain. The choice of medication depends on the pain’s severity, patient history, and side effects.
- Multimodal pain management: Using different analgesic techniques, like local anesthetics, nerve blocks, or patient-controlled analgesia, can improve pain relief. This approach also reduces opioid use.
As one expert says, “A multimodal approach to pain management not only improves patient outcomes but also reduces the risk of opioid dependency.” Pain management strategies are tailored to each patient’s needs and the specific surgery.
Innovations in minimally invasive neurosurgery
The field of neurosurgery is changing fast, moving towards less invasive methods. This change helps reduce surgical trauma and speeds up patient recovery. It’s all thanks to new medical technologies and a better understanding of the brain.
Advanced Techniques to Reduce Surgical Trauma
Minimally invasive neurosurgery uses new methods to cut down on surgical trauma. Endoscopic surgery is one, where doctors make small cuts and use a camera and special tools. Stereotactic surgery uses precise images to find and treat specific brain areas.
Laser technology is also making a big impact in neurosurgery. Lasers can precisely target tumors and lesions, causing less damage to healthy tissue. This leads to quicker healing times.
How New Technologies Minimize Pain During and After Surgery
New tech is key in cutting down pain during and after neurosurgery. Intraoperative imaging like MRI and CT scans lets surgeons see what they’re doing in real-time. This means they can avoid extra steps and damage, reducing pain.
Also, there’s been big progress in pain management. Now, doctors can create custom pain plans for patients. They use non-opioid painkillers, which are safer and less likely to cause addiction.
By using these advanced methods and tech, neurosurgeons can greatly lessen the harm of surgery. This results in less pain and quicker healing for patients.
Conclusion
The dura mater is key in protecting the brain and spinal cord. Knowing about it is important for managing pain during and after neurosurgery. It’s very sensitive to pain because of its nerve connections.
This sensitivity can cause headaches and migraines. To manage pain well, neurosurgeons and anesthesiologists need to understand the dura mater’s structure and function. They work together to reduce pain during surgery.
They use anesthesia and pain medicines to help. New, less invasive surgery methods have made recovery better and pain less. By learning more about the dura mater, doctors can find new ways to help patients feel less pain.
FAQ
Does the brain have pain receptors?
The brain itself does not have pain receptors. But, the dura mater, a protective layer around the brain, is very sensitive to pain.
What is the dura mater, and where is it located?
The dura mater is the outermost layer that covers the brain and spinal cord. It’s between the skull and the brain. It also surrounds the spinal cord in the spinal canal.
Why is the dura mater highly pain-sensitive?
The dura mater has many nerve fibers. This makes it very sensitive to pain. When it gets irritated or inflamed, it can cause headaches or migraines.
Can you feel pain during neurosurgery?
Usually, patients don’t feel pain during neurosurgery because they’re under anesthesia. But, the type of anesthesia can change based on the surgery. Some surgeries, like awake craniotomy, need patients to be awake.
What is an awake craniotomy, and how is pain managed during it?
An awake craniotomy is a surgery where the patient stays awake. Pain is managed with local anesthesia and careful watching by the anesthesiologist.
How do surgeons protect the spinal dura during spine surgery?
Surgeons are very careful to not hurt the spinal dura during spine surgery. They use special techniques and tools to avoid dural tears.
What are the complications related to dural tears and CSF leaks?
Dural tears can cause cerebrospinal fluid (CSF) leaks. This can lead to headaches, infection, or other problems. Surgeons often fix dural tears right away to avoid these issues.
How is post-operative pain managed after neurosurgery?
After neurosurgery, pain is managed with medicines like analgesics. Sometimes, more advanced pain management is used. The choice depends on the surgery and the patient’s health.
What innovations are being made in minimally invasive neurosurgery?
New technologies and techniques are making neurosurgery less invasive. This reduces trauma, pain, and recovery time. Advances include better imaging, endoscopic procedures, and robotic-assisted surgery.
Are there pain receptors in the pia mater or arachnoid mater?
The pia mater, attached to the brain and spinal cord, doesn’t have pain receptors like the dura mater. The arachnoid mater, another layer, is not sensitive to pain.
Can brains feel pain?
The brain tissue itself can’t feel pain because it lacks pain receptors. But, the dura mater and blood vessels around it can cause pain.
What role does anesthesia play in neurosurgery?
Anesthesia is key in neurosurgery to prevent pain and keep patients comfortable. Anesthesiologists watch and manage the anesthesia to ensure the best conditions for surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202893/



































