Last Updated on December 3, 2025 by Bilal Hasdemir
Neurosurgery is a complex field that deals with surgeries on the brain and spinal cord. A surprising fact is that neurosurgical procedures can have a big impact on patient outcomes. Some studies show a high rate of complications. The brain and spinal cord are very delicate. This makes neurosurgery very challenging.
Are all neurosurgeries considered high risk surgeries? Get the awful truth about the dangers and the critical factors that define risk.
Surgeries like craniotomy and spinal surgery are very complex. They carry big risks. Neurosurgery needs a lot of skill and precision from surgeons.
Key Takeaways
- Neurosurgery involves complex procedures on the brain and spinal cord.
- The delicacy of these organs makes neurosurgery inherently challenging.
- Surgeries such as craniotomy and spinal surgery carry significant risks.
- Neurosurgeons must possess a high level of skill and precision.
- Patient outcomes can be significantly impacted by neurosurgical procedures.
Understanding Neurosurgery: Definition and Scope

Neurosurgery deals with surgeries for brain, spine, and nervous system problems. It needs a deep understanding of the nervous system’s complex structures and functions.
What Defines Neurosurgical Procedures
Neurosurgical procedures are precise and delicate. They use advanced technology to avoid harming nearby tissues.
Key elements that define neurosurgical procedures include:
- Precision in surgical techniques
- Use of advanced imaging and navigation systems
- Microsurgical instruments designed for minimal invasiveness
The Delicate Nature of Neural Tissues
The brain, spinal cord, and nerves are highly sensitive and complex. Any surgery in these areas must be done carefully to avoid more harm.
Historical Context of Neurosurgery
Neurosurgery has a long and changing history. It started with ancient practices and has evolved to modern microsurgery and endovascular techniques. Advances in technology and understanding of the brain have greatly improved surgery outcomes.
The history of neurosurgery is filled with important milestones. These include the use of anesthesia, antiseptic techniques, and now robotics and intraoperative imaging.
Why Neurosurgery Ranks Among High Risk Surgeries
Neurosurgery is considered high-risk because it can lead to serious complications. It deals with delicate areas of the body. The complex nature of these surgeries and their impact on critical brain structures make them risky.
Complexity of the Central Nervous System
The central nervous system (CNS) is incredibly complex and essential. It includes the brain and spinal cord, controlling many body functions. This complexity makes neurosurgery very challenging.
The delicate nature of neural tissues and their limited ability to heal add to the challenge. Surgeons must use precise techniques and know neuroanatomy well to avoid harming nearby tissues.
The brain is a complex and dynamic system, and neurosurgery requires a deep understanding of its intricacies.
Proximity to Vital Brain Structures
Neurosurgery often involves working on or near vital brain parts. The proximity to critical areas like the brainstem, cranial nerves, and major blood vessels raises the risk of complications. Damage to these areas can cause severe neurological problems or even death.
Risk Factor | Description | Potential Consequence |
Complexity of CNS | Involves delicate neural tissues and structures | Neurological deficits, limited regeneration |
Proximity to Vital Structures | Operating near critical brain areas | Damage to brainstem, cranial nerves, or major blood vessels |
Surgical Errors | Errors during surgical procedures | Significant neurological damage, death |
Consequences of Surgical Errors
Surgical mistakes in neurosurgery can have severe effects. The margin for error is minimal, and errors can cause serious neurological damage. This can greatly impact a patient’s quality of life or even be fatal.
To reduce these risks, neurosurgeons receive extensive training. They also use advanced technologies like intraoperative imaging and navigation systems. These tools help improve precision and safety during surgeries.
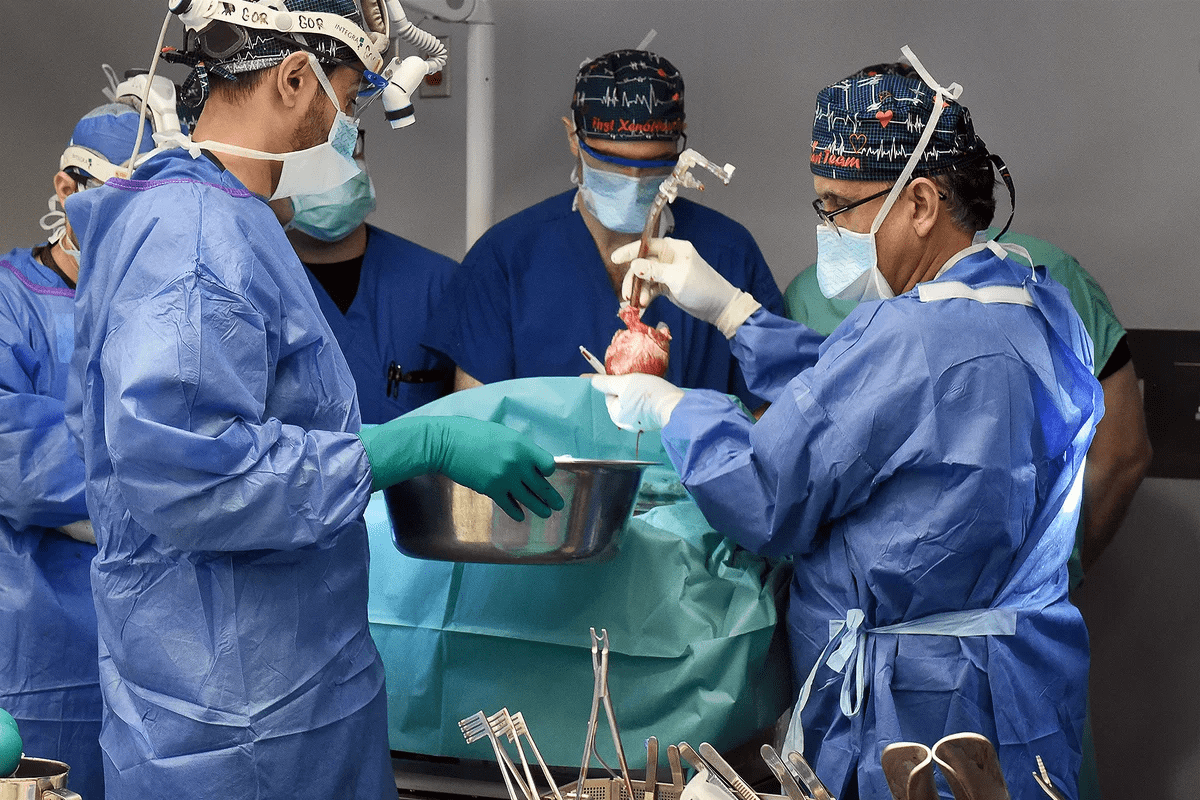
Common Types of Neurosurgical Procedures and Their Risk Profiles
Neurosurgical procedures treat many brain, spine, and nervous system issues. Each procedure has its own risk level. These surgeries are key for treating various conditions.
Brain Tumor Resection
Removing a brain tumor is a complex surgery. It involves taking out a tumor from the brain. This surgery has big risks, like damage to brain tissue, infection, and nerve problems.
The brain’s complex structure and the delicate nature of neural tissues make this surgery very hard.
Cerebrovascular Surgeries
Cerebrovascular surgeries fix blood vessel problems in the brain. These include aneurysm clipping and AVM treatment. Risks include stroke, bleeding, and damage to blood vessels.
The brain’s blood vessels are very complex. Surgeons must be very precise to avoid problems.
Spine and Spinal Cord Procedures
Spine and spinal cord surgeries relieve pressure, stabilize the spine, or fix damaged discs. These include discectomy, spinal fusion, and decompression. Risks include nerve damage, infection, and spine instability.
Functional Neurosurgery
Functional neurosurgery aims to improve nervous system function. This includes deep brain stimulation for Parkinson’s disease or epilepsy. While these surgeries can greatly improve life, they also have risks.
Risks include infection, hardware failure, and side effects like cognitive or motor problems.
It’s important to know the risks of these neurosurgical procedures. This helps patients make informed choices. Weighing the risks and benefits is key to the best outcomes.
Mortality Rates in Neurosurgery: Statistical Analysis
Looking at neurosurgery mortality rates shows a complex picture. Many factors play a role. Neurosurgical procedures are risky because they deal with the nervous system.
Procedure-Specific Mortality Data
Different neurosurgical procedures have different mortality rates. For example, surgeries for brain tumors have different risks than cerebrovascular surgeries or spinal procedures.
- Brain tumor resections have mortality rates ranging from 1-5% depending on the tumor’s location and size.
- Cerebrovascular surgeries, such as aneurysm clipping, have reported mortality rates between 2-10%.
- Spinal surgeries generally have lower mortality rates, typically less than 1%, but can vary based on the complexity of the procedure.
Comparison with Other Surgical Specialties
Neurosurgery is among the higher risk categories when compared to other surgical specialties. But, the conditions treated are often life-threatening. This justifies the risks.
“The mortality rates for neurosurgical procedures are comparable to those of cardiac surgery, highlighting the high-risk nature of both specialties.”
N. G. Birbilis et al., Journal of Neurosurgery
Factors Influencing Survival Rates
Several factors affect survival rates in neurosurgery. These include the patient’s health before surgery, the surgeon’s experience, and postoperative care.
- Patient comorbidities and age play a significant role in determining outcomes.
- The experience and volume of surgeries performed by the neurosurgeon are critical factors.
- Advancements in surgical techniques and technology have contributed to improved survival rates.
Understanding these factors is key for patients and healthcare providers. It helps make informed decisions about neurosurgical interventions.
Major Complications Associated with Neurosurgical Procedures
Neurosurgical procedures can lead to major complications, affecting patient outcomes greatly. These surgeries are often needed to treat life-threatening conditions. They involve delicate tissues and critical structures, making them risky.
Neurological Deficits
Neurological deficits are a big risk in neurosurgery. These can happen when brain or spinal cord tissues get damaged during surgery. Even with careful techniques, there’s always a chance of harming neurological function.
Types of Neurological Deficits:
- Motor deficits: Weakness or paralysis of limbs
- Sensory deficits: Loss of sensation or altered sensory perception
- Cognitive deficits: Impairments in memory, attention, or executive function
Infection and Hemorrhage Risks
Infections and hemorrhages are serious issues after neurosurgery. Infections can come from contamination during or after surgery. Hemorrhages might happen if there’s not enough bleeding control or if a blood vessel is injured.
Complication | Description | Risk Factors |
Infection | Bacterial or fungal infection at the surgical site | Contamination, compromised immune status |
Hemorrhage | Bleeding at the surgical site or intracranially | Inadequate hemostasis, vascular fragility |
Long-term Complications
Long-term issues can greatly affect a patient’s quality of life after neurosurgery. These can include chronic pain, epilepsy, and hydrocephalus, among others.
Managing these long-term problems often needs a team effort. This team includes neurologists, rehabilitation specialists, and other healthcare experts.
It’s key for surgeons and patients to understand these possible complications. By knowing and preparing for these risks, healthcare providers can better care for patients and improve outcomes.
Patient-Specific Risk Factors in Neurosurgery
Neurosurgery is complex due to many patient-specific risk factors. These factors greatly affect the success of neurosurgical procedures. It’s vital for healthcare providers to evaluate them carefully.
Age and Comorbidities
Age is a big risk factor in neurosurgery. Older patients have less physical strength and often have health issues like high blood pressure and diabetes. These health problems can make surgery and recovery harder.
Younger patients face different risks, often tied to their condition, not age. Knowing these age-related factors helps tailor surgery and care to each patient’s needs.
Tumor Location and Characteristics
The location and type of brain tumors or neurosurgical conditions are key in determining surgical risk. Tumors in eloquent areas of the brain, like those controlling speech or vision, are riskier. This is because they can lead to serious neurological problems after surgery.
The size, grade, and type of tumor also affect the surgery’s approach and risk. For example, big, blood-rich tumors are at higher risk of bleeding. Tumors deep in the brain may need more complex surgery to reach.
Previous Neurological History
A patient’s past neurological history is also very important. Those with previous brain surgeries, radiation, or neurological conditions like stroke face more challenges. This is because their brain’s structure and function may be different.
Knowing a patient’s neurological history helps surgeons prepare for possible complications. It shows the need for a detailed preoperative check-up to reduce risks.
In summary, factors like age, health conditions, tumor details, and past neurological issues are key in neurosurgery. By carefully looking at these, healthcare providers can manage risks better. This leads to better outcomes for patients undergoing neurosurgery.
The Surgeon Factor: Training and Expertise in Neurosurgery
Neurosurgery is very complex and requires a lot of training and experience. It’s a specialized field that needs a deep understanding of the brain, spine, and nervous system. Surgeons must also have the technical skills for detailed surgical procedures.
To become a neurosurgeon, one must go through a lot of education and training. This includes medical school and a neurosurgery residency that lasts six to seven years. During this time, they get hands-on experience in neurosurgical procedures under experienced surgeons.
Educational Requirements for Neurosurgeons
The path to becoming a neurosurgeon is long and challenging. After medical school, they apply for a neurosurgery residency program. These programs are accredited by the Accreditation Council for Graduate Medical Education (ACGME). They offer training in both the theory and practice of neurosurgery.
Getting into a neurosurgery residency is very competitive. Candidates need a strong academic record and a commitment to neurosurgery. In the program, they work under experienced neurosurgeons, gradually taking on more responsibility as they gain experience and skills.
Volume-Outcome Relationship
Studies show that the volume of surgical procedures a surgeon performs affects patient outcomes. Surgeons who do more procedures tend to have better results. This is because they gain more experience and refine their techniques.
This is very true in neurosurgery, where procedures are complex and delicate. High-volume neurosurgeons have lower complication rates and better outcomes for complex procedures like brain tumor resections and cerebrovascular surgeries.
Subspecialization Impact on Outcomes
Subspecialization in neurosurgery also affects patient outcomes. As neurosurgery has evolved, many surgeons specialize in areas like pediatric neurosurgery, spine surgery, or neuro-oncology.
Subspecialization helps neurosurgeons develop deeper expertise in their chosen area. This can lead to better outcomes for patients. For example, a pediatric neurosurgeon is better equipped to handle surgeries on children.
In conclusion, the training and expertise of neurosurgeons are key to patient outcomes in neurosurgery. Understanding the educational requirements, the volume-outcome relationship, and the impact of subspecialization helps us appreciate the complexities of this field.
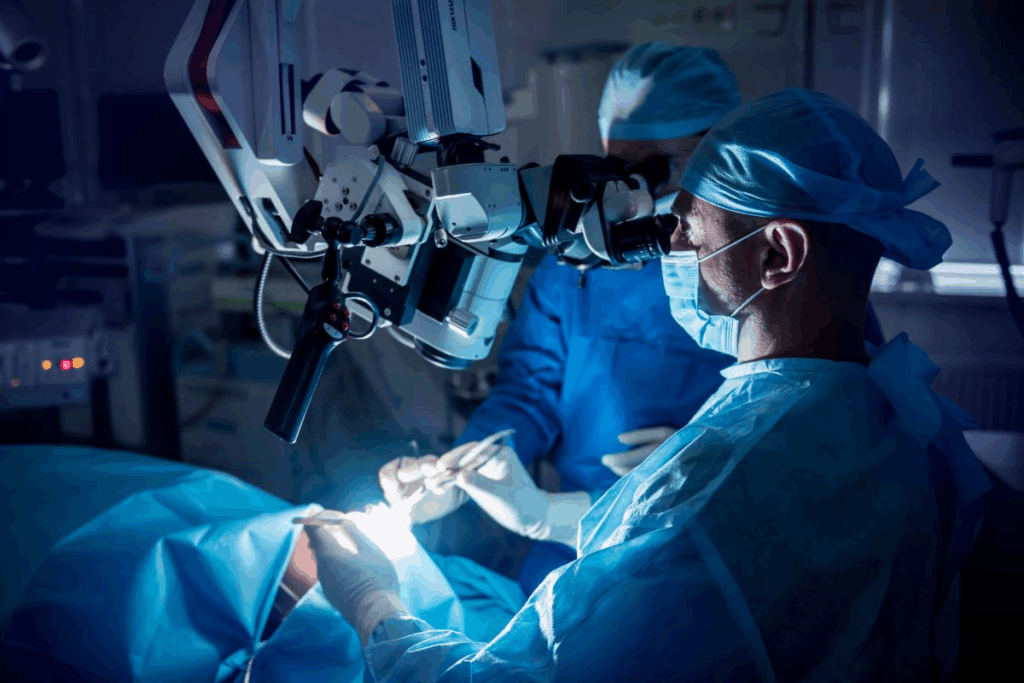
Technological Advancements Reducing Risks in Neurosurgery
New technology is changing neurosurgery for the better. It makes surgeries safer and more precise. This is thanks to better tools for working on the brain and spinal cord.
Intraoperative Imaging and Navigation
Intraoperative imaging and navigation are big steps forward. They let surgeons see the brain in real-time. This makes it easier to find and remove problems.
- Improved Accuracy: This tech helps surgeons make better plans during surgery. It makes removing tumors or other issues more precise.
- Enhanced Safety: It also gives surgeons feedback in real-time. This reduces the chance of harming important brain parts.
Minimally Invasive Approaches
Minimally invasive surgery is becoming more common. It causes less damage, scarring, and recovery time. These surgeries use small incisions and special tools for detailed work.
- Reduced Trauma: These surgeries cause less damage to tissues. This means patients recover faster and feel less pain after surgery.
- Lower Infection Risk: With smaller cuts, there’s a lower chance of infections.
Robotic Assistance in Neurosurgery
Robotic systems are being used more in neurosurgery. They offer better control, precision, and stability. This helps with very detailed and tricky surgeries.
- Precision and Control: Robots give surgeons better control over their tools. This leads to more accurate and careful work.
- Complex Procedure Support: Robots help with surgeries that are hard or impossible with old methods.
These new technologies are making neurosurgery safer and more effective. They help improve patient results and open up new ways to treat brain and spinal cord problems.
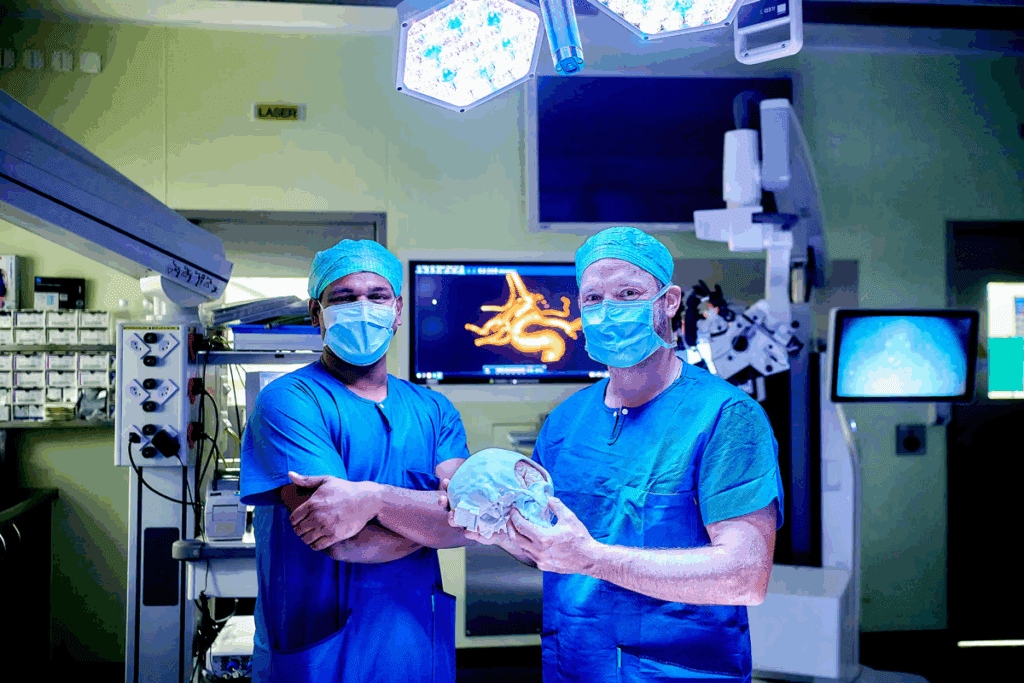
Preoperative Planning and Risk Assessment
Neurosurgery’s success depends on good preoperative planning and risk assessment. Neurosurgeons must look at the patient’s condition, the surgery’s complexity, and possible risks. This ensures the best results.
Advanced Imaging Techniques
Advanced imaging is key in planning surgeries. Tools like MRI and CT scans give detailed views of the body’s structure and any problems. This helps surgeons choose the best surgical path.
Multidisciplinary Tumor Boards
Multidisciplinary tumor boards are important. They gather experts from different fields to talk about tough cases. This teamwork helps make better decisions for the patient.
Specialty | Role in Tumor Board |
Neurosurgeon | Surgical planning and execution |
Oncologist | Cancer treatment planning |
Radiologist | Imaging interpretation |
Patient-Specific Surgical Planning
Planning surgery for each patient is vital. It means making the surgery fit the patient’s unique body and health issues. This can lower risks and better outcomes.
Key elements of patient-specific planning include:
- Detailed imaging analysis
- 3D modeling and simulation
- Intraoperative navigation
By using advanced imaging, teamwork, and custom planning, neurosurgeons can make surgeries safer and more effective.
Comparing Neurosurgery to Other High Risk Surgeries
Neurosurgery is as risky as cardiac and transplant surgery. It deals with the brain and spinal cord, which are very delicate. This makes neurosurgery very complex.
High-risk surgeries, like neurosurgery, cardiac surgery, and complex oncological procedures, have some things in common. They all need precise techniques and skilled surgeons. They also carry the risk of serious complications.
Cardiac Surgery Risk Comparison
Cardiac surgery is also very risky. It involves the heart, which is vital for life. The procedures are complex, adding to the risks.
Both neurosurgery and cardiac surgery have high mortality rates. But, the risks are different because of the organs involved.
Surgical Specialty | Average Mortality Rate (%) | Common Complications |
Neurosurgery | 1-2 | Neurological deficits, infection |
Cardiac Surgery | 2-3 | Myocardial infarction, renal failure |
Transplant Surgery | 1-5 | Rejection, infection, graft failure |
Transplant Surgery Risk Profiles
Transplant surgery is also high-risk. It involves replacing a diseased organ with a healthy one. Risks include rejection, infection, and graft failure.
Transplant surgery is complex and requires immunosuppression. This adds to its risks. While both neurosurgery and transplant surgery are risky, the risks are different.
Complex Oncological Procedures
Complex oncological surgeries are risky too. They involve removing tumors, which can be dangerous. The risks depend on the tumor’s location, size, and the patient’s health.
In conclusion, neurosurgery is risky, but so are cardiac surgery, transplant surgery, and complex oncological procedures. Knowing these risks helps surgeons and patients make better choices.
The Risk-Benefit Analysis: When Is Neurosurgery Worth the Risk?
When thinking about neurosurgery, patients and their families must weigh the benefits against the risks. This is called a risk-benefit analysis. It’s key to making a smart choice about surgery.
Life-Threatening Conditions
For life-threatening conditions like brain tumors or severe brain injuries, surgery might be the only choice. The chance to save a life or prevent more damage makes surgery worth the risk.
For example, surgery for a brain tumor can greatly improve survival and quality of life. Doctors carefully look at the patient’s health, the condition, and the surgery’s chances of success before deciding.
Quality of Life Considerations
Neurosurgery is also considered for conditions that badly affect a patient’s quality of life. This includes chronic pain or certain mental health issues. The surgery’s benefits are weighed against the risks to see if it can greatly improve daily life.
For instance, deep brain stimulation for Parkinson’s can greatly reduce symptoms and improve movement. This can greatly improve a patient’s life. The choice to have surgery depends on the expected benefits and risks.
Alternative Treatment Options
The existence of alternative treatments is also important in deciding on neurosurgery. Patients and doctors must think if other treatments, like medicine or therapy, can manage the condition without surgery.
In some cases, a mix of treatments might be suggested. This could include surgery along with other therapies for the best results. The choice depends on the benefits and risks of each option and what’s best for the patient.
In summary, choosing neurosurgery is a complex decision. It involves a detailed risk-benefit analysis. This looks at the condition’s severity, the chance for better quality of life, and other treatment options.
Informed Consent in High-Risk Neurosurgical Procedures
Informed consent is key in high-risk neurosurgery. It makes sure patients know the risks and benefits. This involves a detailed talk between the patient and the doctor about the surgery.
Communicating Surgical Risks Effectively
Talking about surgical risks is very important. Neurosurgeons need to explain the possible problems like brain damage, infection, and bleeding. This helps patients understand what they might face.
Using pictures and written info can help patients get it better. For example, brain diagrams can show where the surgery will be and what risks are there.
Patient Decision-Making Process
The decision-making process for patients is complex. It depends on their values, what they want, and how well they understand the info. Patients should be able to ask questions and get things clarified if they’re unsure.
A good decision-making process includes:
- Explaining the diagnosis and treatment choices
- Talking about the risks and benefits of each option
- Looking at other treatments or care options
Legal and Ethical Considerations
Informed consent is both a moral and legal must. Not getting proper consent can lead to legal trouble, like lawsuits.
Legal Consideration | Description |
Informed Consent Doctrine | Patients must know about the risks, benefits, and other choices. |
Patient Autonomy | It’s about respecting the patient’s right to decide on their health care. |
Documentation | Keeping detailed records of the consent process is vital. |
In conclusion, informed consent is essential in neurosurgery. It makes sure patients are well-informed and involved in their care decisions.
Future Directions in Reducing Neurosurgical Risks
New trends and technologies are changing neurosurgery. They offer ways to lower risks and better patient results. The field is set for a big change, thanks to new tools that promise better surgery, fewer problems, and faster healing.
Emerging Technologies
Technologies like artificial intelligence (AI), robotics, and advanced imaging are key. AI algorithms can predict patient results, spot problems, and plan surgeries better. Robotics adds precision and skill to complex operations.
AI in neurosurgery is more than just better results, a top neurosurgeon. It’s about making care fit each patient’s needs, thanks to advanced data and models.
Personalized Medicine Approaches
Personalized medicine is a big hope for safer neurosurgery. Tailoring treatments to each patient’s genes, environment, and lifestyle can lower risks and boost success.
- Genomic profiling to find genetic markers linked to neurosurgical risks
- Custom surgical plans based on each patient’s unique anatomy and disease
- Targeted treatments that tackle the specific causes of a patient’s condition
Training Innovations
New ways to train surgeons are also vital. Simulation training lets surgeons practice in a safe space. This boosts their skills and confidence before real surgeries.
Simulation training is changing how we teach neurosurgeons. It’s not just about lowering risks; it’s about making sure our surgeons have the best skills.
By following these new paths, neurosurgery is ready to see big drops in surgical risks. This will lead to better patient results and a better life for everyone.
Conclusion: Balancing Risks and Benefits in Neurosurgery
Neurosurgery is a complex field with big risks but also great benefits. It helps patients with serious and life-threatening conditions. We’ve looked at what neurosurgery is, its scope, and the risks involved.
Success in neurosurgery comes from weighing the risks against the benefits. This means careful planning before surgery, using advanced imaging, and knowing the patient’s needs well.
Knowing the risks and benefits helps patients and doctors make better choices. New techniques and technologies in neurosurgery are making treatments safer and more effective. This gives hope to those with complex neurological conditions.
Choosing neurosurgery should be a thoughtful decision. It involves looking at the risks and benefits and talking it over with your healthcare team.
FAQ
What are the most common types of neurosurgical procedures?
Neurosurgery includes many types of procedures. These include removing brain tumors, fixing blood vessels in the brain, and surgeries on the spine. It also includes surgeries that improve brain function.
What are the risks associated with brain tumor resection?
Removing brain tumors can be risky. It can damage nearby brain tissue, cause neurological problems, lead to infection, or cause bleeding.
How does the complexity of the central nervous system contribute to the risk of neurosurgery?
The brain and spinal cord are very complex. This makes neurosurgery very challenging. It requires careful work on delicate and important structures.
What are the major complications associated with neurosurgical procedures?
Serious complications can happen. These include lasting brain or nerve damage, infection, bleeding, and long-term problems like memory loss.
How do patient-specific risk factors influence outcomes in neurosurgery?
Each patient’s situation is unique. Factors like age, health problems, where the tumor is, and past health can affect the surgery’s success and recovery.
What role does the surgeon’s training and expertise play in neurosurgery?
A surgeon’s skill and experience are key in neurosurgery. More experienced neurosurgeons usually have better results for their patients.
How are technological advancements reducing risks in neurosurgery?
New technologies are making neurosurgery safer. These include better imaging, smaller incisions, and robotic tools. They help surgeons work more precisely.
What is the importance of preoperative planning and risk assessment in neurosurgery?
Planning and assessing risks before surgery are very important. They help reduce risks and improve outcomes. This includes using advanced imaging and planning the surgery for each patient.
How does neurosurgery compare to other high-risk surgical specialties?
Neurosurgery is as risky as other high-risk surgeries. This includes heart surgery, transplant surgery, and complex cancer surgeries. They all have similar risks and outcomes.
What is the risk-benefit analysis involved in deciding to undergo neurosurgery?
Deciding on neurosurgery involves weighing the benefits against the risks. This includes considering life-threatening conditions and how the surgery will affect the patient’s quality of life.
What is the role of informed consent in high-risk neurosurgical procedures?
Informed consent is very important in neurosurgery. It means clearly telling patients about the risks. It also involves understanding their decision-making process.
What are the future directions for minimizing risks in neurosurgery?
The future looks promising. New technologies, personalized medicine, and better training are on the horizon. They aim to improve patient outcomes.
What is the hardest surgery to perform?
Neurosurgery is often the most challenging. This is because of the brain and spinal cord’s complexity and delicacy.
What is the riskiest surgery?
Neurosurgery is considered one of the riskiest. It’s complex, involves critical areas, and has a high chance of complications.
What are the top 3 riskiest surgeries?
Neurosurgery, heart surgery, and complex cancer surgeries are among the riskiest. They all have high risks and outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25260742/