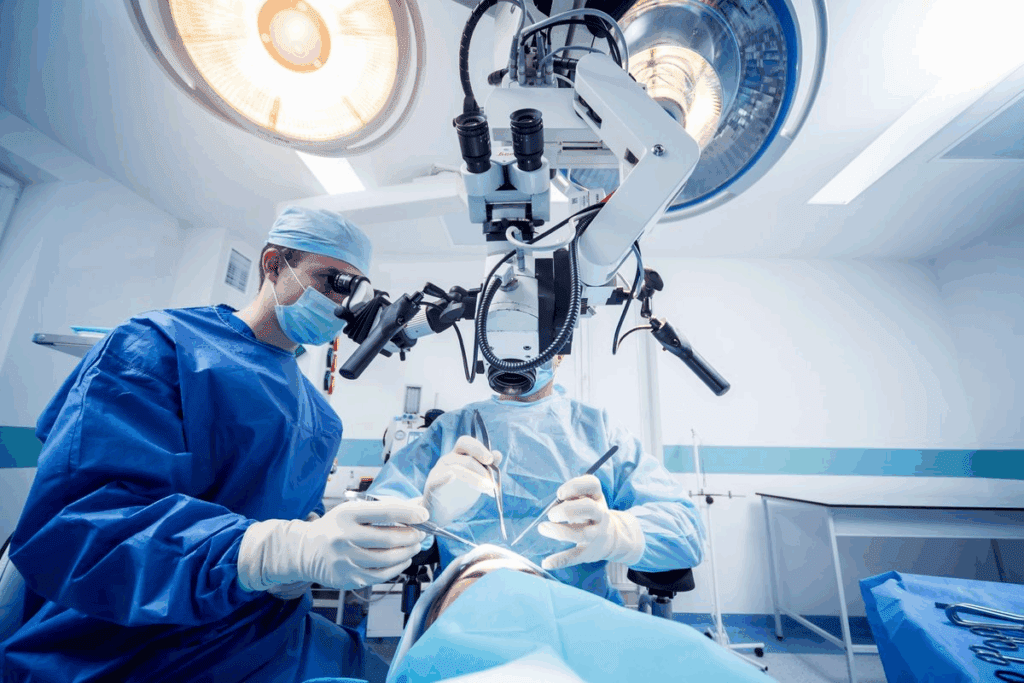
Many people worry about being restrained during surgery. The truth is about surgical patient immobilization. It’s all about keeping the patient safe and the surgery successful. Our guide to patient positioning during neurosurgery. Learn the amazing, critical safety steps, including straps, to ensure a successful operation.
In neurological procedures, safety is top priority. Neurosurgery needs the patient to stay very calm. This is why keeping them steady is so important.
To do this, doctors use straps and stabilizing devices. They pick the right tools based on the surgery and the patient‘s health.
Key Takeaways
- Immobilization is key for neurosurgery success.
- Teams use different ways to keep patients safe.
- The right method depends on the surgery and patient health.
- Patient safety guides the choice of immobilization.
- Good immobilization helps with precise neurological procedures.
The Necessity of Surgical Restraints in Neurosurgery
Neurosurgery needs precision, and surgical restraints are key to keeping patients safe. These procedures are so delicate that patients must stay perfectly calm to avoid harm.
Medical Rationale Behind Patient Immobilization
Keeping patients steady during neurosurgery is vital. Even a tiny move can hurt the brain’s tiny parts. Restraints help keep the patient stable, reducing risks.
Consequences of Patient Movement During Neurological Procedures
Moving during neurosurgery can cause big problems. It can lead to brain damage or too much bleeding. The table below shows what can happen if a patient moves during surgery.
| Consequence | Description | Potential Outcome |
| Neurological Damage | Movement causing injury to neural structures | Permanent neurological deficit |
| Excessive Bleeding | Movement resulting in vascular injury | Hemorrhage, potentially life-threatening |
| Infection | Movement compromising sterile technique | Post-operative infection |
Knowing these risks shows why surgical restraint protocols are so important. They help keep patients safe and make sure surgeries go well.
Patient Positioning During Neurosurgery: Core Principles and Importance
In neurosurgery, how the patient is positioned is key to a successful surgery. Patient positioning techniques help surgeons get the best view of the area they need to operate on. They also make sure the patient is safe and comfortable.
Fundamental Concepts of Neurosurgical Positioning
Neurosurgical positioning follows a few main rules. These rules help surgeons work with precision. They make sure the patient’s body is aligned right, the area to be operated on is visible, and the patient is not harmed.
The supine, prone, lateral, and sitting positions are often used in neurosurgery. Each position has its own use and challenges. The right position depends on where the problem is, how the surgery will be done, and the patient’s health.
Impact of Positioning on Surgical Outcomes
Good patient positioning is key to keeping the patient’s nerves safe. It helps surgeons find and access the problem area accurately. This reduces risks and improves results.
It’s important to do a full check-up before deciding on the best position for the patient. This check-up looks at the patient’s health, the type of neurosurgery needed, and any risks of the surgery.
Balance Between Restraint and Patient Safety
Finding the right balance between keeping the patient steady and keeping them safe is important. The use of restraints and positioning tools must be careful. This is to avoid pressure injuries, nerve damage, and other complications while keeping the patient in the right position.
“The art of neurosurgery is not just about the technical skill of the surgeon, but also about the meticulous attention to detail in patient positioning.”
— Expert Neurosurgeon
Understanding the basics of patient positioning and its role in neurosurgery helps improve care. It makes surgeries better, keeps patients safer, and leads to better results.
Common Types of Positioning Devices and Restraints

Neurosurgical procedures need precise patient positioning. This is done with various devices and restraints. The right position is key for surgery success and patient safety. Different devices help keep the patient in the right spot during the procedure.
Head Fixation Systems: Pins, Clamps, and Frames
Head fixation systems are vital in neurosurgery. They keep the patient’s head stable. These systems include:
- Pins: Used in skull fixation, these pins are part of a rigid frame that holds the head in place.
- Clamps: Adjustable clamps are used to secure the head, providing flexibility and stability.
- Frames: Stereotactic frames are used for precise localization and fixation of the head.
These head fixation systems allow forprecision medical intervention. They make sure the surgical site is accessible and stable.
Body Positioning Systems: Cushions, Pads, and Tables
Body positioning systems support the patient’s body during surgery. They ensure comfort and safety. These include:
- Cushions and pads: Used to support and protect vulnerable areas, such as the back and limbs.
- Surgical tables: Specialized tables that can be adjusted to various positions, facilitating surgical table positioning.
Using these systems well helps withpatient comfort management. It reduces the risk of pressure injuries and nerve damage.
Limb Securing Mechanisms: Straps, Tapes, and Supports
Limb securing mechanisms are key for keeping the patient’s limbs safe and stable. These mechanisms include:
- Straps: Adjustable straps that secure the limbs to the surgical table.
- Tapes: Hypoallergenic tapes used to gently secure limbs or medical devices.
- Supports: Customized supports that cradle the limbs, preventing movement.
| Device | Purpose | Benefits |
| Head fixation systems | Stabilize the head | Precision, stability |
| Body positioning systems | Support the body | Comfort, safety |
| Limb securing mechanisms | Secure limbs | Stability, safety |
A medical expert notes, “The key to successful neurosurgery lies in the precise positioning of the patient. This is achieved through a combination of these devices and restraints.”
This shows the importance of the right equipment and skilled staff for patient positioning.
Understanding the different positioning devices and restraints is key. Medical professionals can then ensure patients get the best care during neurosurgical procedures. This balancesanesthetic response monitoringwith the need for precise positioning.
The Surgical Positioning Process: Step by Step
The surgical positioning process is key in neurosurgery. It needs careful planning and execution. It ensures the patient’s safety and the success of the surgery.
Pre-operative Assessment and Planning
A comprehensive health assessment is done before surgery. It looks at the patient’s medical history and current health. It also considers their specific needs for the surgery.
The team plans the best positioning strategy. They think about the surgery type, the patient body alignment, and neuromuscular system protection.
Intraoperative Positioning Protocols
In the operating room, surgical team coordination is vital. They position the patient as planned. They adjust the table, use devices, and secure the patient to prevent movement.
The aim is to keep the patient in the best position. This helps the surgery and keeps the patient safe and comfortable.
Continuous Monitoring of Patient Position
The patient’s position is watched closely during surgery. This ensures the position is optimal and safe. It helps protect the patient body alignment and overall health.
Any needed changes are made quickly. This keeps the patient safe and the surgery successful.
Position-Specific Considerations for Different Neurosurgical Approaches
The choice of patient position is key in neurosurgery. It affects both how easy it is to do the surgery and how safe it is for the patient. Neurosurgery needs precise positioning to get the best results and avoid problems.
Supine Position Techniques and Applications
The supine position is very common in neurosurgery. It’s great for reaching the front and sides of the brain. Proper padding and support are key to avoid injuries and nerve damage. This position is often used for clipping aneurysms in the brain and for decompressing cranial nerves.
Prone Position Challenges and Solutions
The prone position is used for surgeries in the back of the brain and spine. It has its challenges, like the risk of injuries and breathing problems. Careful positioning and constant monitoring are vital to reduce these risks. To help, special tables and padding are used to protect sensitive areas.
Lateral and Sitting Position Requirements
The lateral position is for surgeries on the sides of the brain and spine. It requires careful attention to keep the spine straight and avoid nerve compression. The sitting position, though less common, is used for surgeries in the back of the brain. It offers better access to the area.
Park Bench Position for Posterior Fossa Surgery
The park bench position is a special version of the lateral position. It’s used for surgeries in the back of the brain and cerebellum. It gives great access to the area while keeping the patient stable.
Considerations for Skull Base Approaches
Skull base surgeries need special positioning to reach complex areas. The position chosen depends on the specific problem and how the surgery will be done. Preoperative planning and intraoperative adjustments are essential for a successful surgery.
| Position | Applications | Key Considerations |
| Supine | Anterior circulation aneurysm clipping, cranial nerve decompression | Proper padding, support to prevent pressure injuries |
| Prone | Posterior fossa and spinal surgeries | Pressure injury prevention, airway management |
| Lateral | Lateral cranial and spinal procedures | Spinal alignment, nerve compression prevention |
Procedure-Specific Positioning Requirements
Neurosurgical procedures need special positioning to improve surgical accuracy. The complexity of these surgeries means patient positioning must be carefully planned. This ensures the best possible results.
Brain Tumor Resection Positioning
For brain tumor surgeries, getting the position right is key. It helps surgeons reach the tumor without harming nearby brain tissue. MRI and CT scans help plan the best position for accessing the tumor.
Spine Surgery Positioning Challenges
Spine surgeries face unique challenges because of the need to keep the spine stable. Proper positioning is critical. It helps surgeons get the right angle and ensures their tools work accurately.
Cerebrovascular Procedure Considerations
Cerebrovascular surgeries, like aneurysm clipping, need careful positioning. This is to protect neurological function. The strategy must be well thought out to access the vascular lesion effectively.
Functional Neurosurgery Positioning Precision
In functional neurosurgery, getting the position right is essential. Comprehensive surgical evaluation is needed to find the best position for each patient. This ensures the placement of electrodes or other devices is accurate.
| Procedure | Positioning Requirement | Surgical Consideration |
| Brain Tumor Resection | Precise tumor localization | Minimize brain tissue damage |
| Spine Surgery | Maintain spinal stability | Ensure instrumentation accuracy |
| Cerebrovascular Procedure | Optimal vascular access | Preserve neurological function |
| Functional Neurosurgery | Precise electrode placement | Maximize therapeutic efficacy |
The Role of Anesthesia in Patient Positioning and Immobilization
Anesthesia is key in placing patients correctly for surgery. It keeps them comfortable and safe, which is very important in neurosurgery. Here, the right position is critical.
Anesthetic Considerations for Different Positions
The type of anesthesia needed changes with the patient’s position. For example, those lying face down need different care than those on their back. Precision in anesthetic delivery is vital to avoid problems.
Monitoring Physiological Responses During Positioning
It’s important to watch how the patient reacts during positioning. This means keeping an eye on their vital signs and neuromuscular function. This helps make sure the patient is not stressed or hurt.
“The anesthesiologist plays a critical role in managing the patient’s physiological responses to positioning, ensuring that any adverse effects are promptly addressed.” – Expert in Anesthesiology
Managing Anesthetic Complications Related to Positioning
Even with careful planning, problems can happen. Effective management of these issues is key to avoiding long-term damage. This includes being ready to handle breathing or heart problems caused by the position.
In summary, anesthesia plays a big role in how patients are positioned and kept safe during surgery. It requires careful thought and management to ensure the patient’s comfort and safety.
Comprehensive Risk Assessment Before Positioning
Before neurosurgery, a detailed risk assessment is key. It looks at many factors that could affect patient safety and the surgery’s success.
Patient safety is the top priority. A thorough risk assessment spots possible problems during positioning. This way, healthcare teams can act early to prevent issues.
Patient-Specific Risk Factors
Each patient’s unique factors guide the positioning strategy. These include:
- Age and overall health status
- Pre-existing medical conditions, such as diabetes or cardiovascular disease
- Previous surgical procedures or injuries
- Anatomical variations or abnormalities
For example, a patient with spinal surgery history needs careful positioning to avoid worsening their condition.
Procedure-Related Risk Considerations
The neurosurgical procedure’s type affects the risk assessment. Each procedure has its own needs and possible complications. For instance:
“The positioning of patients for neurosurgical procedures requires careful consideration of the surgical approach, the patient’s anatomy, and the possible risks of the procedure.”
Surgeons must think about the procedure’s specific demands. This includes the need for precise positioning or the risk of nerve damage.
Medical History Review for Safe Positioning
Reviewing a patient’s medical history is vital for safe positioning. It helps spot risks and plan ways to reduce them. Important parts of the review include:
| Medical History Element | Relevance to Positioning |
| Previous surgeries or injuries | Impacts positioning strategy and risk assessment |
| Chronic conditions (e.g., diabetes, hypertension) | Influences patient response to positioning and anesthesia |
| Allergies or sensitivities | Affects choice of materials used in positioning (e.g., straps, pads) |
By examining patient-specific risks, procedure-related risks, and medical history, healthcare teams can ensure safe and effective positioning.
Patient Safety Protocols During Surgical Immobilization
Keeping patients safe during surgery is very important. Surgical immobilization is key in many neurosurgical procedures. It requires precise positioning for the best results. Good safety protocols help avoid risks.
Preventing Pressure Injuries and Nerve Damage
One big worry is avoiding pressure injuries and nerve damage. Pressure injuries happen when pressure stays on one spot for too long. Nerve damage can come from bad positioning or too much pressure on nerves. To avoid these, teams use padding and special devices.
They use gel pads and foam cushions to ease pressure on sensitive spots. They also make sure limbs are positioned right to avoid nerve issues.
Maintaining Proper Body Alignment
Keeping the body aligned right is key for safety. It helps avoid muscle and joint strain. This reduces the chance of pain and problems after surgery.
optimal patient positioning is critical for neurosurgical success and avoiding complications.Optimal patient positioning is critical for neurosurgical success and avoiding complications.
Protecting Vulnerable Anatomical Structures
Special care is needed for sensitive areas like the eyes, ears, and nerves. They use eye shields, padding around the ears, and careful positioning to protect these areas.
- Eye shields to protect the eyes
- Padding around the ears to prevent pressure damage
- Meticulous positioning to avoid nerve compression
Temperature Management During Prolonged Procedures
Keeping the right temperature is also important during long surgeries. Too cold or too hot can harm the patient. Teams use warming blankets and heated fluids to keep the body temperature normal.
They watch the patient’s temperature closely and adjust as needed to keep it stable.
Special Positioning Considerations for Diverse Patient Populations
Neurosurgical success depends on tailored positioning for different patients. A patient-centered treatment approach means knowing each patient’s unique needs. This includes kids, seniors, and those with health issues.
Pediatric Neurosurgical Positioning
Pediatric patients face special challenges because of their size and growing bodies. Innovative surgical techniques are needed. This includes special head fixation and careful padding to avoid injuries.
| Consideration | Pediatric | Adult |
| Head Fixation | Specialized pediatric pins | Standard adult pins |
| Body Support | Custom padding | Standard gel pads |
Geriatric Patient Considerations
Geriatric patients often have health issues like osteoporosis or arthritis. Medical risk stratification helps identify risks. This way, their positioning can be adjusted.
The key to successful surgical outcomes in elderly patients lies in meticulous preoperative assessment and planning, including careful consideration of their positioning needs.
Adaptations for Patients with Pre-existing Conditions
Patients with neurological conditions need special positioning. It’s important to understand how their condition affects neurological condition management.
- Careful assessment of the patient’s medical history
- Adaptation of positioning to accommodate physical limitations
- Monitoring for complications related to their condition
Obesity and Its Impact on Surgical Positioning
Obesity adds challenges to surgical positioning, like pressure injuries and breathing problems. Innovative surgical techniques and special equipment, like bariatric tables, are key for obese patients.
By meeting the unique needs of different patients, neurosurgeons can improve outcomes and safety.
Technological Advancements in Surgical Positioning Systems
New technologies are changing how patients are positioned during surgery. This makes surgeries more precise and safer. Advanced systems are improving patient care and outcomes.
Computer-Assisted Positioning Technologies
Computer-assisted systems are becoming key for better patient positioning. They use smart software and hardware. This ensures patients are placed correctly, cutting down on mistakes.
Benefits of Computer-Assisted Positioning:
- Enhanced precision in patient alignment
- Reduced risk of positioning-related injuries
- Improved surgical access and visibility
Pressure-Sensing Devices and Monitoring
Pressure-sensing devices are now part of surgical tables and systems. They watch for pressure points on the patient’s body. This helps avoid injuries and keeps patients comfortable during long surgeries.
Key Features of Pressure-Sensing Devices:
- Real-time pressure monitoring
- Alerts for excessive pressure points
- Customizable pressure thresholds
Integration with Neuronavigation Systems
Combining surgical systems with neuronavigation tech makes neurosurgery more precise. This setup tracks the patient’s body and the tools in real-time. It boosts surgical accuracy.
Advantages of Integrated Systems:
- Improved anatomical accuracy
- Enhanced surgical precision
- Better outcomes in complex neurosurgical procedures
Robotic Assistance in Patient Positioning
Robots are helping with patient positioning for better accuracy and consistency. They can place patients accurately and keep them in position during surgery. This reduces the need for manual adjustments.
Benefits of Robotic Assistance:
- High precision in patient positioning
- Reduced risk of human error
- Improved efficiency in the operating room
Potential Complications from Improper Positioning and Prevention Strategies
Neurosurgical procedures need careful patient positioning to avoid complications. This ensures the surgery goes well and keeps the patient safe. But, if the positioning is wrong, it can cause serious and lasting problems.
Neurological Complications: Recognition and Prevention
Improper positioning can damage nerves and cause compression injuries. Monitoring neurological function during surgery is key. This helps catch and fix any problems early on. Using electrophysiological monitoring is a good way to spot issues quickly.
Vascular and Circulatory Issues
Wrong positioning can also cause blood flow and vein problems. Making sure the patient’s body is properly aligned and supported helps avoid these issues. It’s important to check blood flow and vein health during long surgeries.
Musculoskeletal Injuries and Long-term Effects
Muscle and joint injuries can happen from too much pressure or bad positioning. Careful planning and padding of pressure points can help prevent these injuries. It’s also key to check for muscle and joint problems after surgery.
Respiratory Complications in Prone and Lateral Positions
Respiratory problems are more likely in prone and lateral positions. This is because the lungs can get compressed and the diaphragm can move less. Adjusting the patient’s position to help breathing and watching breathing closely are important steps to prevent these issues.
| Complication Type | Prevention Strategies | Monitoring Requirements |
| Neurological | Electrophysiological monitoring, careful positioning | Continuous neurological monitoring |
| Vascular/Circulatory | Proper body alignment, regular circulation checks | Regular vascular assessment |
| Musculoskeletal | Padding pressure points, careful positioning | Post-operative musculoskeletal assessment |
| Respiratory | Optimizing position for respiratory mechanics | Continuous respiratory monitoring |
Patient Preparation, Communication, and Psychological Aspects
A patient-centered treatment approach is key in neurosurgery. It starts with thorough preparation and clear communication. This method boosts patient safety and improves surgical results. It makes sure patients are ready both physically and mentally for the surgery.
Explaining Positioning Procedures to Patients
It’s important to clearly explain positioning procedures to patients. This helps reduce their anxiety. The surgical team should communicate effectively. They need to make sure patients understand why they must stay in place during surgery.
They should explain the devices used and how they keep patients safe and comfortable.
Addressing Patient Concerns About Restraints
Patients often worry about being restrained during surgery. It’s vital to address these concerns empathetically. Explain that restraints are for their safety and the success of the surgery.
By understanding the reasons, patients can feel more at ease.
Obtaining Informed Consent for Positioning
Getting informed consent is a key step in preparing patients. This means discussing the surgery, the positioning process, and any restraints. Patients need to know what to expect, including any risks or discomforts from positioning.
Managing Anxiety Related to Immobilization
Reducing patient anxiety is a big part of preoperative care. Using relaxation exercises and preoperative counseling can help. The surgical team should work together to create a supportive environment.
This environment should address patient concerns and help them feel calm.
By focusing on patient preparation, clear communication, and psychological support, healthcare providers can improve the surgical experience for neurosurgery patients. This approach not only leads to better outcomes but also makes the surgery less intimidating.
Conclusion: Balancing Surgical Necessity with Patient Comfort and Safety
Getting a patient in the right position for neurosurgery is key. It helps get the best results and keeps the patient safe and comfortable. A full health check is needed to spot risks and plan to avoid problems.
It’s important to weigh the need for surgery against keeping the patient safe. This means careful planning and watching the patient closely during the surgery. This way, we can avoid bad outcomes.
Knowing how to position patients right is a big step in making surgery safer. It helps doctors and nurses give better care. This mix of surgery needs and patient comfort is what makes care top-notch.
In the end, a good plan for patient positioning is essential. It helps get the best results and keeps patients safe during neurosurgery.
FAQ
Why is patient positioning so important in neurosurgery?
Proper positioning in neurosurgery is key for a successful surgery. It ensures the surgeon can access the area they need. It also lowers the risk of problems and improves the surgery’s outcome.
What types of positioning devices are used in neurosurgery?
Neurosurgery uses various devices for positioning. These include head fixation systems like pins and frames. Body positioning systems, such as cushions, and limb securing mechanisms like straps are also used.
How does anesthesia affect patient positioning in neurosurgery?
Anesthesia is very important for positioning in neurosurgery. The type of anesthesia needed changes based on the position. It’s vital to watch how the body reacts to the position to avoid problems.
What should be considered when positioning patients with pre-existing conditions?
Patients with pre-existing conditions need special care in positioning. It’s important to adapt the positioning to their needs. This might mean extra protection for certain areas or managing obesity.
How do new technologies improve surgical positioning systems?
New technologies like computer-assisted systems and pressure sensors make positioning safer and more accurate. Robotic help in positioning is also becoming more common.
What complications can arise from improper patient positioning?
Improper positioning can cause many problems. These include damage to the nervous system, blood flow issues, muscle injuries, and breathing problems. It’s important to know these risks and take steps to prevent them.
How can patient safety be ensured during surgical immobilization?
To keep patients safe during immobilization, it’s important to prevent pressure injuries. Maintaining proper alignment and protecting sensitive areas are also key. Managing temperature during long procedures is another important aspect.
Why is a thorough risk assessment necessary before positioning?
A detailed risk assessment is essential before positioning. It helps identify risks specific to the patient and the procedure. This information allows for a safe and effective positioning plan.
How can patient comfort and anxiety be managed during positioning?
To manage comfort and anxiety, clear communication and empathy are key. Explaining the positioning process and listening to concerns can help reduce anxiety. Getting informed consent is also important.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S1878875017340366




































