
Nearly 7% of patients face serious issues after brain surgery. This shows how complex and risky this procedure is.What happens after a failed brain surgery? Discover the awful, devastating truth and the critical next steps patients and families face.
If a surgical procedure on the brain fails, the effects can be severe. They affect not just the patient but also their family and caregivers.
Both patients and doctors must understand the potential problems and outcomes of a failed surgical intervention.
Key Takeaways
- The risk of significant complications after brain surgery is substantial.
- Failed surgical interventions can have far-reaching consequences.
- Understanding possible outcomes is key for patients and caregivers.
- Brain surgery complications can vary widely in their impact.
- Doctors must carefully consider the risks and benefits.
Understanding Brain Surgery and Its Complexity
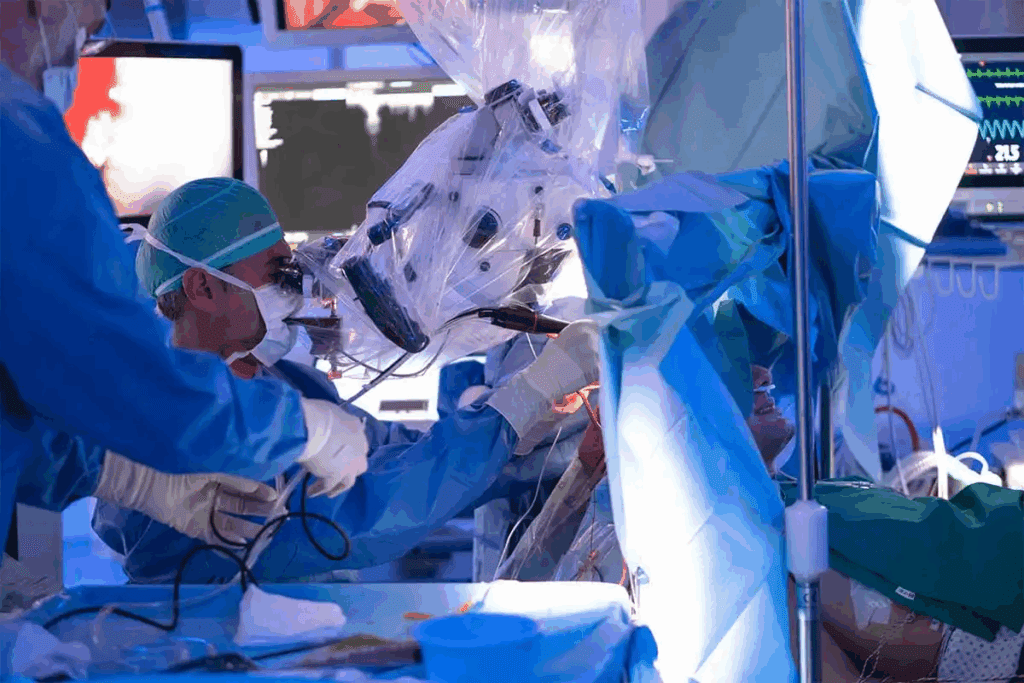
Brain surgery is complex and involves many types and risks. It treats conditions affecting the brain. These surgeries can save lives but are risky due to the brain’s delicate nature.
Types of Brain Surgeries and Their Purposes
There are many types of brain surgeries, like craniotomies and deep brain stimulation. Each is for a different condition. For example, craniotomies remove part of the skull to access the brain.
Tumor removal surgeries aim to take out growths. Deep brain stimulation uses electrodes to manage movement disorders.
Inherent Risks in Neurosurgical Procedures
Even with progress, neurosurgery carries risks. These include surgical complications like infection and bleeding. The risk depends on the patient’s health, the surgery’s complexity, and the team’s skill.
Good surgical risk management is key to reducing these risks. It helps ensure the best results.
Defining Failed Brain Surgery: When Outcomes Don’t Meet Expectations
Surgical failure in brain surgery means not getting the expected results. This can happen for many reasons. These include problems during surgery, risks the patient has, or how the body reacts.
Medical Definition of Surgical Failure
Surgical failure is when surgery doesn’t work as planned. This could be because of technical issues, the brain’s complexity, or unexpected problems.
Doctors look at many things to see if surgery was a success. They check images, how the patient feels, and the results of the surgery. For example, if a tumor isn’t fully removed or symptoms stay, it’s seen as a failure.
Patient Perspective vs. Medical Perspective
Patients and doctors might see surgery differently. Patients might think surgery failed if they’re not better or have bad side effects. Even if the surgery was technically successful.
It’s important to understand these differences. It shows we need to talk clearly between doctors and patients. This way, everyone knows what to expect and the risks involved in brain surgery.
Common Causes of Failed Brain Surgery
It’s important to know why brain surgery can fail. Even with new technology and techniques, brain surgery is very complex. It comes with its own set of risks.
Many things can lead to brain surgery failure. These include mistakes during surgery, technical issues, patient risks, and how the body reacts.
Surgical Error and Technical Complications
Mistakes during surgery and technical problems are big reasons for failure. Surgical error brain happens when the surgeon damages nearby brain tissue or uses the wrong techniques. Issues with equipment or tools can also cause problems.
Patient-Related Risk Factors
Patient-related risk factors are key in brain surgery success or failure. Things like age, health, and past medical conditions matter. For example, older people or those with certain health issues might face more risks of neurological damage during surgery.
Unpredictable Biological Responses
How the body reacts to surgery can also cause failure. Even with good planning, the body’s response can be unpredictable. This can lead to infections, inflammation, or bad reactions to anesthesia.
In summary, brain surgery can fail due to surgical mistakes, patient risks, and unexpected body reactions. Knowing these reasons helps us find ways to reduce risks and improve results.
Immediate Complications Following Unsuccessful Neurosurgery
When neurosurgery doesn’t go as planned, immediate complications can arise. These complications can be life-threatening and require immediate medical intervention.
Brain Swelling and Increased Intracranial Pressure
Recovering from brain surgery involves a complex and detailed process.
Symptoms of increased ICP include headache, nausea, vomiting, and altered consciousness. Prompt treatment, including medications to reduce swelling and, in some cases, surgical intervention to relieve pressure, is essential.
Hemorrhage and Blood Clots
Hemorrhage, or bleeding, is another serious complication that can occur after neurosurgery. It can lead to the formation of blood clots in or around the brain, which can cause stroke or further brain damage. Hemorrhagic complications can be catastrophic, highlighting the need for close monitoring.
Signs of hemorrhage or blood clots may include sudden neurological deficits, headache, or changes in consciousness. Immediate imaging studies, such as CT scans, are critical for diagnosing these conditions, and urgent intervention may be required to prevent long-term damage.
Infection and Inflammation
Recovering from brain surgery involves a complex and detailed process.
Symptoms of infection or inflammation include fever, headache, and neurological changes. Prompt antibiotic treatment and, in some cases, additional surgery may be necessary to manage these complications effectively.
| Complication | Symptoms | Treatment |
| Brain Swelling | Headache, nausea, vomiting, altered consciousness | Medications to reduce swelling, surgical intervention |
| Hemorrhage/Blood Clots | Sudden neurological deficits, headache, changes in consciousness | Immediate imaging, urgent surgical intervention |
| Infection/Inflammation | Fever, headache, neurological changes | Antibiotics, additional surgery |
Long-Term Neurological Consequences
Failed brain surgery can cause many long-term problems. These issues can greatly affect a person’s life quality. They can impact different parts of the brain’s function.
Cognitive and Memory Impairments
Cognitive and memory problems are common after failed brain surgery. These can be mild or severe. They can make it hard to do everyday tasks and stay independent. Rehabilitation programs that focus on cognitive therapy can help.
Motor Function Deficits
Motor function problems are another issue. Patients might have weakness, paralysis, or trouble with coordination. The severity depends on where the surgery was and the complication. Physical therapy is key in helping patients regain lost motor skills or adapt to new limitations.
Speech and Language Disorders
Speech and language disorders can also happen. These make it hard for patients to talk and communicate. Speech therapy is usually suggested to improve communication skills.
The long-term effects of failed brain surgery highlight the need for good care and rehab after surgery. Knowing these outcomes helps healthcare providers support patients better in their recovery.
Specific Outcomes of Failed Brain Surgery by Procedure Type
When brain surgery fails, the effects can be severe. They depend on the type of surgery. Each procedure has its own risks and possible problems.
Tumor Removal Complications
Tumor removal surgeries are complex. They can lead to incomplete removal, damage to brain tissue, and infections. Complications can lead to significant morbidity, affecting the patient’s quality of life.
Aneurysm Clipping and Coiling Failures
Aneurysm clipping and coiling treat cerebral aneurysms. Failures can cause aneurysm rupture or rebleeding, leading to severe consequences. Technical issues, like clip slippage or coil migration, can also happen.
Deep Brain Stimulation Issues
Deep brain stimulation (DBS) treats various neurological conditions. Complications include hardware malfunction, infection, and unwanted stimulation effects. These issues can greatly affect the patient’s condition and quality of life.
Craniotomy Risks and Complications
Craniotomy involves temporarily removing a skull bone flap. Risks include infection, brain swelling, and damage to brain tissue. Post-operative hemorrhage is another serious complication that needs immediate medical attention.
Understanding these specific outcomes is key. It helps manage patient expectations and improve surgical techniques.
Post-Operative Management After Surgical Complications
Recovering from brain surgery involves a complex and detailed process.
Emergency Interventions
When surgery problems happen, quick action is needed. Life-saving procedures like emergency brain surgeries or bleeding control are often required. Acting fast is critical to avoid more harm and help the patient get better.
Secondary Surgeries and Revisions
At times, more surgeries are needed to fix issues from the first operation. These follow-up surgeries aim to fix problems like leftover tumors or malfunctioning brain implants. The choice to have more surgery depends on the patient’s health and the surgery’s benefits.
Medical Management Strategies
Recovering from brain surgery involves a complex and detailed process.
| Management Strategy | Description | Goals |
| Emergency Interventions | Immediate actions to stabilize the patient | Prevent further damage, save life |
| Secondary Surgeries | Additional surgeries to correct complications | Correct issues, improve outcomes |
| Medical Management | Use of medications to manage symptoms and complications | Support recovery, minimize deficits |
Rehabilitation and Recovery Process
Recovering from brain surgery involves a complex and detailed process. It involves a rehabilitation program made just for the patient. This program is key to helping patients get back their lost functions and reach the best possible outcome.
Physical Therapy Approaches
Physical therapy is a big part of getting better. It focuses on getting patients to move and function again. Personalized therapy plans are made for each patient. These plans include exercises to boost strength, balance, and coordination.
Physical therapists work with patients to beat physical challenges. They use physical manipulation and exercise therapy to help. The goal is for patients to be able to do things on their own again.
Cognitive Rehabilitation
Cognitive rehabilitation is also very important. It helps with problems caused by brain surgery. This includes strategies to improve memory, attention, and problem-solving skills.
Cognitive therapists use different methods, like cognitive training programs and compensatory strategies. They aim to help patients do daily tasks better.
Timeline and Expectations for Recovery
The time it takes to recover can vary a lot. It depends on the surgery’s complexity and the patient’s health. Recovery usually takes several months to a year or more.
Knowing the recovery timeline and expectations helps patients and their families prepare. Regular check-ups with doctors are important. They help track progress and adjust the rehabilitation plan if needed.
| Rehabilitation Phase | Timeline | Expected Outcomes |
| Initial Recovery | 0-3 months | Regaining basic functions, managing pain |
| Intensive Rehabilitation | 3-6 months | Improving mobility, cognitive functions |
| Advanced Rehabilitation | 6-12 months | Achieving independence, refining skills |
Advances in Neurosurgery to Prevent Failures
The field of neurosurgery is seeing big changes with new technologies and methods. These aim to cut down on surgical mistakes. Recent years have brought big improvements in many areas, making neurosurgery more precise and safe.
Imaging and Navigation Technologies
Recovering from brain surgery involves a complex and detailed process.
- Improved accuracy in tumor removal
- Enhanced safety during aneurysm clipping
- Better preservation of surrounding brain tissue
Minimally Invasive Techniques
Minimally invasive methods have changed neurosurgery a lot. They make incisions smaller, which means less recovery time and less scarring. Endoscopic surgery and keyhole surgery are examples. They let surgeons do complex work through small openings. These methods lead to better results and lower risks for patients.
Surgical Risk Management Protocols
Managing surgical risks is very important in neurosurgery. Preoperative checklists and intraoperative monitoring help spot and fix possible problems. These steps make sure teams are ready and can handle any issues quickly.
- Preoperative planning and patient assessment
- Intraoperative monitoring and adjustment
- Postoperative care and follow-up
Conclusion: Moving Forward After Unsuccessful Brain Surgery
Recovering from brain surgery involves a complex and detailed process.
Support after surgery is key. It helps patients deal with the surgery’s effects. This support includes medical care and ways to regain lost abilities. Knowing what options are available can help people face their challenges.
Recovering from brain surgery involves a complex and detailed process.
FAQ
What are the most common complications of brain surgery?
Common issues include brain swelling, hemorrhage, and blood clots. Infections and neurological damage are also possible. These problems can happen right away or later and might need extra medical help.
How is failed brain surgery defined?
Failed brain surgery means the surgery didn’t work as planned. This can lead to ongoing or new brain problems. It might also mean needing more surgery. The exact definition depends on the surgery’s goal and the patient’s situation.
What are the risks associated with craniotomy?
Risks with craniotomy include infections, bleeding, and blood clots. There’s also a chance of stroke, seizures, and brain damage. But, these risks can be lowered with careful planning and aftercare.
Can brain surgery cause long-term neurological damage?
Yes, brain surgery can lead to lasting brain problems. These can affect thinking, memory, movement, and speech. The extent of damage varies based on the surgery, where it was done, and the patient’s health.
What is the role of rehabilitation after brain surgery?
Rehabilitation is key for recovery after brain surgery, even with complications. Physical, cognitive, and speech therapy help patients regain lost abilities. They also learn to cope with any lasting issues.
How can surgical risk be managed in neurosurgery?
Managing risk in neurosurgery means choosing the right patients and planning carefully. Using precise techniques and providing good aftercare also helps. New technologies and methods have made surgeries safer and more effective.
What are the possible consequences of brain swelling after surgery?
Brain swelling can cause high pressure in the brain. This might lead to more damage, seizures, or even death. Quick medical action is needed to control swelling and avoid serious problems.
Can infection occur after brain surgery?
Yes, infections can happen after brain surgery. They can be caused by bacteria or fungi. Quick treatment with antibiotics or antifungals is needed to prevent serious issues.
How long does it take to recover from brain surgery?
Recovery time varies based on the surgery, the patient’s health, and any complications. Some might recover in weeks, while others take months or more to fully recover.
What are the benefits of minimally invasive neurosurgical techniques?
Minimally invasive techniques cause less damage, reduce pain, and lead to shorter hospital stays. They also help patients recover faster. These methods can lower the risk of complications and improve surgery outcomes.
References
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://www.bmj.com/content/352/bmj.i1297



































