Last Updated on December 1, 2025 by Bilal Hasdemir
Glioblastoma multiforme is the most aggressive and malignant brain tumor. It has an inferior prognosis. Getting diagnosed with this condition often means a low brain cancer survival rate. This is a big worry for both patients and doctors glioblastoma cancer.
The glioblastoma survival rate is very low. Most patients face a tough prognosis. It’s important to understand glioblastoma cancer to find better treatments and improve patient care.
Key Takeaways
- Glioblastoma multiforme is the most aggressive form of brain tumor.
- The prognosis for glioblastoma cancer is generally poor.
- Brain cancer survival rates are significantly low for glioblastoma patients.
- Understanding glioblastoma is key to developing effective treatments.
- Research into glioblastoma is ongoing to improve patient outcomes.
Understanding Brain Tumors and Their Classification

Brain tumors are divided into types based on where they start, how they grow, and what they look like under a microscope. This helps doctors figure out the best way to treat them.
Primary vs. Secondary Brain Tumors
Brain tumors are either primary or secondary. Primary brain tumors start in the brain. Secondary brain tumors, or metastatic tumors, come from cancer cells that spread to the brain from elsewhere.
- Primary brain tumors include gliomas, meningiomas, and schwannomas, based on where they start.
- Secondary brain tumors are more common and often come from cancers like lung, breast, or melanoma.
Benign vs. Malignant Brain Tumors
Another key way to classify tumors is by their behavior: benign or malignant. Benign brain tumors are not cancerous and usually have a better outlook. Malignant brain tumors are cancerous and can grow fast.
- Benign tumors grow slowly and don’t spread to nearby tissues.
- Malignant tumors grow quickly, spread to nearby brain tissue, and can spread through the nervous system.
The WHO Classification System for Brain Tumors
The World Health Organization (WHO) has a system for classifying brain tumors. It looks at their appearance and molecular makeup. This system helps doctors diagnose and predict outcomes.
The WHO system grades tumors based on their look, like how abnormal the cells are and how much they grow. Knowing the WHO grade is key for planning treatment and understanding the tumor’s outlook.
Overview of Common Brain Tumor Types
Brain tumors fall into several types, like meningiomas, pituitary adenomas, schwannomas, and gliomas. Knowing these types helps doctors choose the right treatment and predict outcomes.
Meningiomas
Meningiomas are usually benign tumors from the meninges. These protective membranes cover the brain and spinal cord. They grow slowly and might not show symptoms until they press on nearby brain areas.
Characteristics of Meningiomas:
- Usually benign
- Arise from the meninges
- Can be asymptomatic for a long time
Pituitary Adenomas
Pituitary adenomas are benign tumors in the pituitary gland. This small gland is at the brain’s base. They can mess with hormone levels, leading to various symptoms based on their size and hormone impact.
Symptoms may include:
- Hormonal imbalances
- Visual disturbances
- Headaches
Schwannomas
Schwannomas are benign tumors from Schwann cells. These cells cover nerve fibers. They can pop up on any nerve, including brain nerves, and grow slowly.
Key Features:
- Benign nature
- Originate from Schwann cells
- Can cause neurological symptoms depending on their location
Gliomas
Gliomas are tumors from brain glial cells. They vary from low-grade (less aggressive) to high-grade (more aggressive). Glioblastoma is a high-grade glioma known for its aggressive behavior and poor prognosis.
Gliomas are classified based on:
- Cell type
- Grade of malignancy
- Genetic characteristics
Ranking Brain Tumors by Prognosis
Knowing the prognosis of brain tumors is key to choosing the right treatment. The outlook varies greatly based on the tumor type, grade, location, and the patient’s health.
Brain Tumors with Favorable Prognosis
Some brain tumors have a better outlook because they are benign or respond well to treatment. Meningiomas, for instance, are usually benign and can often be cured with surgery. Pituitary adenomas can be managed with surgery, medication, and radiation therapy.
Brain Tumors with Moderate Prognosis
Some gliomas, like low-grade astrocytomas, have a moderate prognosis. These tumors grow slowly and can be treated with watchful waiting, surgery, or radiation. But, they can turn malignant, requiring close monitoring and aggressive treatment.
Brain Tumors with Poor Prognosis
High-grade gliomas, such as Anaplastic astrocytomas and glioblastoma multiforme (GBM), have a poor prognosis. They grow quickly and are hard to treat.
Glioblastoma: The Brain Tumor with the Worst Prognosis
Glioblastoma multiforme (GBM) is the most aggressive and malignant brain tumor. Despite treatments like surgery, radiation, and chemotherapy, the outlook for GBM patients is grim. They usually live about 15 months after diagnosis. GBM’s fast growth and tendency to come back make its prognosis very poor.
Factors Affecting Brain Tumor Prognosis
Many things can affect how well someone with a brain tumor will do. Knowing these factors is key for both patients and doctors. It helps in making the best treatment and care plans.
Tumor Type and Grade
The type and grade of a brain tumor are very important. Brain tumors are grouped by where they come from, like gliomas, meningiomas, and schwannomas. The grade shows how much the tumor cells look like normal cells.
Tumors are graded from I to IV. Higher grades mean the tumors are more aggressive and grow faster.
- Low-grade tumors (Grade I and II) grow slowly and usually have a better outlook.
- High-grade tumors (Grade III and IV) grow quickly and have a worse outlook.
Tumor Location and Size
The spot and size of a brain tumor also matter a lot. Tumors in hard-to-reach spots or near important brain areas are harder to treat. Bigger tumors are also tougher to manage than smaller ones.
Patient Age and Overall Health
A person’s age and health can greatly affect their chances. Younger people usually do better than older ones because they can handle treatments better. Those who are healthier and have fewer other health issues also tend to do better.
Genetic and Molecular Markers
Genetic and molecular markers are used more and more to guess how a brain tumor will do. Certain genetic changes or molecular signs can mean a tumor might do better or worse. For example, some markers show if a tumor will respond well to certain treatments.
- IDH1 and IDH2 mutations in gliomas are linked to a better outlook.
- MGMT promoter methylation is a marker that means a tumor might do better with certain chemo.
By knowing these factors, doctors can give more accurate predictions. They can also make treatment plans that fit each patient’s needs better.
Glioblastoma Cancer: The Most Aggressive Brain Tumor
Glioblastoma is the most severe form of glioma, posing big challenges for doctors and scientists. It’s a fast-growing and aggressive brain cancer that starts in the brain’s glial cells.
What Is Glioblastoma Multiforme (GBM)?
Glioblastoma multiforme grows quickly and spreads into the brain’s tissue, making it hard to remove surgically. It’s classified as a Grade IV astrocytoma by the World Health Organization (WHO). This means it’s very malignant.
Why Glioblastoma Is So Aggressive
Glioblastoma grows fast, spreads into the brain, and doesn’t respond well to treatments. These traits lead to a poor outlook for GBM patients.
- Rapid cell division and growth
- Infiltration into surrounding brain tissue
- Resistance to chemotherapy and radiation
Glioblastoma vs. Other Gliomas
Glioblastoma is different from other gliomas because of its high grade and aggressive nature. It’s more likely to come back and has a worse prognosis than lower-grade gliomas.
| Tumor Type | WHO Grade | Prognosis |
| Glioblastoma | IV | Poor |
| Anaplastic Astrocytoma | III | Moderate to Poor |
| Diffuse Astrocytoma | II | Favorable to Moderate |
Molecular Subtypes of Glioblastoma
Studies have found different molecular subtypes of glioblastoma. This knowledge is key for creating targeted treatments.
- Proneural subtype: Often has a slightly better outlook
- Mesenchymal subtype: Shows a more aggressive behavior
- Classical subtype: Often has EGFR amplification
More research into glioblastoma’s molecular makeup is needed to improve treatment results.
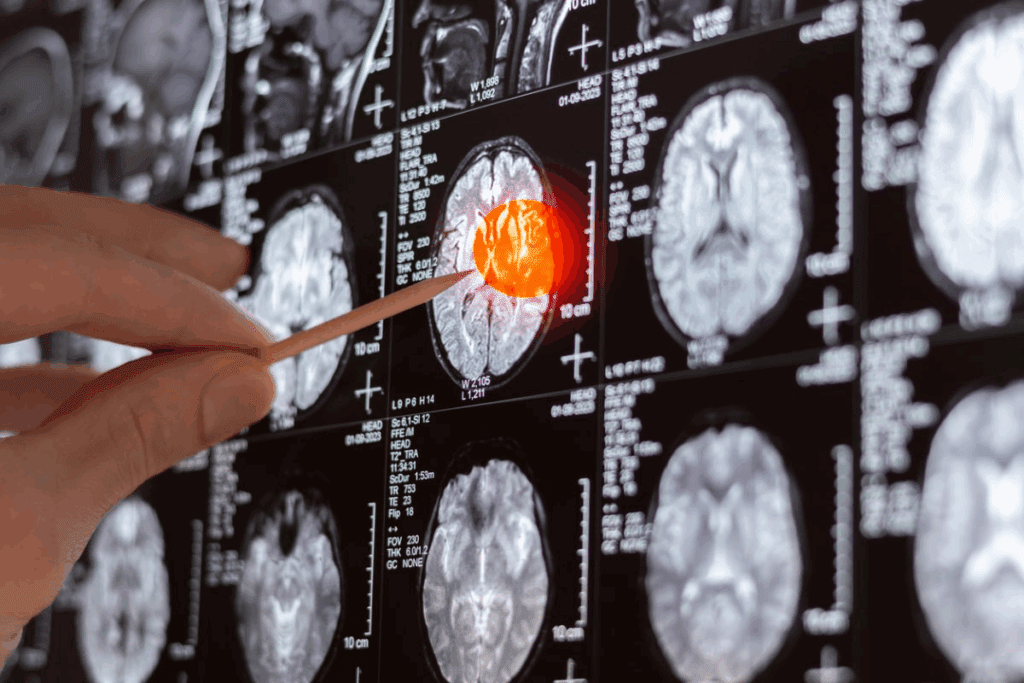
Diagnosing Glioblastoma and Other Malignant Brain Tumors
Diagnosing glioblastoma and other brain tumors is a detailed process. It includes clinical checks, imaging tests, and looking at tissue samples. This thorough method helps find out the tumor’s type and how serious it is. It also guides treatment choices.
Initial Symptoms and Warning Signs
Glioblastoma symptoms can appear quickly. They might include headaches, seizures, confusion, and trouble with speech or moving. ” Spotting these signs early is key for quick medical help.
Common first signs are:
- Headaches that get worse over time
- Seizures, even if you’ve never had them before
- Confusion, disorientation, or memory loss
- Difficulty with speech, vision, or moving
Imaging Techniques (MRI, CT, PET)
Imaging is key in finding glioblastoma. Magnetic Resonance Imaging (MRI) is often first because it’s good at spotting soft tissue issues. Computed Tomography (CT) scans are used too, mainly in emergencies because they’re fast and easy to get. Positron Emission Tomography (PET) scans help see how active the tumor is and if it’s coming back or not.
Biopsy and Pathological Examination
A biopsy is vital to confirm glioblastoma. A neurosurgeon takes a tumor sample, which a pathologist then examines. The pathologist looks at the tumor’s features, like its grade and cells. This info helps figure out how aggressive the tumor is and what treatment to use.
“The histopathological diagnosis remains the gold standard for diagnosing glioblastoma, providing critical information on tumor biology and prognosis.”Neuropathologist
Molecular and Genetic Testing
Molecular and genetic tests are also key in diagnosing glioblastoma. Tests for MGMT promoter methylation and IDH1/IDH2 mutations give important info on how the tumor might behave. These markers help find the best treatments and predict how well a patient will do.
By using clinical signs, imaging, tissue analysis, and genetic tests, doctors can accurately diagnose glioblastoma. This helps create a good treatment plan.
Understanding Glioblastoma Survival Rates
Knowing the survival rates for glioblastoma is key for setting realistic goals and making smart treatment choices. Glioblastoma is a fast-growing brain cancer with survival rates that change based on several factors.
Median Survival Time for Glioblastoma Patients
The median survival time for glioblastoma patients is a key number to know. It usually is about 15 months after diagnosis. But, it can range from 12 to 18 months, depending on the treatment and the patient’s health.
Survival Rates by Age Group
Age plays a big role in glioblastoma survival rates. Younger people generally live longer than older ones. Here’s a table showing survival rates by age.
| Age Group | 1-Year Survival Rate | 5-Year Survival Rate |
| 20-44 years | 40% | 15% |
| 45-54 years | 30% | 8% |
| 55-64 years | 20% | 5% |
| 65 years and older | 10% | 2% |
Factors That May Improve Survival
Several things can help glioblastoma patients live longer. These include:
- Extent of Surgical Resection: Removing more of the tumor can help.
- Participation in Clinical Trials: New treatments in trials can improve survival.
- Genetic and Molecular Markers: Some genetic markers can affect how well treatments work.
Understanding Statistical Limitations
It’s important to know the limits of statistics when looking at glioblastoma survival rates. Survival stats are based on big groups and might not match what happens to one person. Health, how well treatments work, and new treatments can all affect a person’s outcome.
By understanding these points, patients and doctors can make better choices about treatment and care.
Standard Treatment Approaches for Glioblastoma
Treating glioblastoma involves a team of experts. It’s a tough brain cancer that needs a detailed plan. This plan usually includes surgery, radiation, and chemotherapy.
Surgical Resection
Surgery is often the first step in treating glioblastoma. The goal is to remove as much of the tumor as possible safely. This is called maximal safe resection.
“Maximal surgical resection is associated with improved overall survival and is a critical component of the initial treatment plan for glioblastoma patients.”
Radiation Therapy
After surgery, radiation therapy is used to kill any remaining cancer cells. External beam radiation therapy is the most common method. It uses high-energy beams from outside the body.
Radiation therapy is key in managing glioblastoma. It helps slow down the tumor’s growth. A study showed that it improves survival when used with surgery and chemotherapy.
Temozolomide and Chemotherapy Options
Chemotherapy is also a vital part of glioblastoma treatment. Temozolomide is the main chemotherapy drug used. It stops cancer cells from making copies of themselves.
Using temozolomide has been shown to help patients live longer. It’s often given with radiation therapy, followed by more temozolomide.
The Stupp Protocol
The Stupp Protocol is a well-known treatment for glioblastoma. It combines radiation therapy with temozolomide chemotherapy. The treatment involves giving radiation and temozolomide together, then more temozolomide after.
The Stupp Protocol has become a standard treatment. It offers better survival chances. As explained, “The combination of radiation therapy and temozolomide, as outlined in the Stupp Protocol, represents a significant advancement in the treatment of glioblastoma.”
Treatment Outcomes and Recurrence
Understanding how glioblastoma patients respond to treatment is key to improving their lives. Treatment outcomes in glioblastoma show how well the tumor reacts to surgery, radiation, and chemotherapy.
Response Assessment in Neuro-Oncology (RANO) Criteria
The Response Assessment in Neuro-Oncology (RANO) criteria help measure how well brain tumors, like glioblastoma, respond to treatment. They look at changes in tumor size on scans, steroid use, and how the patient feels.
- Complete Response: Disappearance of all tumor on MRI.
- Partial Response: Significant decrease in tumor size.
- Stable Disease: No change in tumor size.
- Progressive Disease: Tumor grows or new lesions appear.
Pseudoprogression vs. True Progression
Pseudoprogression makes it seem like the tumor is growing, but it’s really due to treatment effects. It’s hard to tell the difference between pseudoprogression and true progression, but it’s very important for patient care.
True progression means the tumor is growing despite treatment. This calls for a change in treatment. Doctors use advanced imaging and molecular markers to tell the difference.
Recurrent Glioblastoma Treatment Options
Dealing with recurrent glioblastoma is tough. There are a few ways to manage it:
- Re-resection: Surgery to remove as much of the tumor as possible.
- Re-irradiation: More radiation therapy, planned to avoid harm.
- Salvage Chemotherapy: Different chemotherapy options.
- Clinical Trials: Trying new treatments in trials.
Managing Treatment Resistance
Overcoming treatment resistance in glioblastoma needs a detailed plan. This includes understanding why resistance happens and finding new treatments.
Ways to beat resistance include:
- Creating targeted therapies based on the tumor’s genetics.
- Trying combination therapies to fight resistance.
- Improving immunotherapy to boost the immune system’s fight against the tumor.
Other High-Grade Brain Tumors with Poor Prognosis
High-grade brain tumors like anaplastic astrocytoma and diffuse midline glioma have poor outcomes. They grow fast and don’t respond well to treatments.
Anaplastic Astrocytoma (Grade III)
Anaplastic astrocytoma is a Grade III glioma. It’s more aggressive than lower-grade tumors and can turn malignant easily.
Symptoms include seizures, headaches, and neurological problems. Doctors use MRI and tissue tests to diagnose it.
Diffuse Midline Glioma (Including DIPG)
Diffuse midline glioma, like DIPG, is a very aggressive tumor. It happens in the brain’s midline, like the brainstem.
It’s mostly found in kids and has a bad prognosis. Treatment options are few, and survival time is short.
Medulloblastoma in Adults
Medulloblastoma starts in the cerebellum. It’s more common in kids but can happen in adults too.
In adults, it has a variable prognosis. Treatment includes surgery, radiation, and chemotherapy. Outcomes depend on how much of the tumor is removed and its molecular makeup.
Primary CNS Lymphoma
Primary CNS lymphoma is a rare brain tumor. It’s found in the brain, spinal cord, and eyes. It’s more common in people with weakened immune systems, like those with HIV/AIDS.
Treatment involves chemotherapy and radiation. While it can be cured, it often comes back. Prognosis depends on age, health, and how well it responds to treatment.
The Disease Progression of Glioblastoma
Understanding glioblastoma’s timeline and signs is key to managing it well. This aggressive brain cancer is a big challenge for everyone involved.
Typical Timeline After Diagnosis
The disease’s progression varies, but it usually follows a pattern. After diagnosis, treatments like surgery, radiation, and chemotherapy are common.
Median survival times have improved with better treatments. But, the outlook is generally not good.
| Timeframe | Typical Progression | Common Symptoms |
| 0-3 months | Initial treatment phase | Fatigue, headaches, seizures |
| 3-6 months | Tumor recurrence | Worsening neurological deficits |
| 6+ months | Advanced disease | Significant cognitive decline, increased intracranial pressure |
Signs of Disease Progression
As glioblastoma gets worse, symptoms like worsening neurological deficits and cognitive decline become more common. It’s important to watch for these signs to adjust treatment.
- Increased frequency of seizures
- Worsening headaches or nausea
- Changes in personality or cognitive function
End-of-Life Considerations
For those with advanced glioblastoma, end-of-life care focuses on comfort and symptom management. This phase needs careful support for patients and their families.
Palliative care is key in improving life quality. It helps manage pain and other symptoms.
How Glioblastoma Affects the Body
Glioblastoma affects the body in many ways, including the brain and overall health. As it grows, it can damage brain tissue, leading to various problems.
It can also cause fatigue, weight loss, and overall health decline. These systemic effects make managing the disease harder.
Emerging Treatments and Clinical Trials
New treatments and clinical trials are giving glioblastoma patients hope. Doctors are always looking for better ways to fight this tough brain cancer.
Immunotherapy Approaches
Immunotherapy uses the body’s immune system to fight cancer. Checkpoint inhibitors and CAR-T cell therapy are being tested in trials.
- Checkpoint inhibitors help the immune system attack cancer cells better.
- CAR-T cell therapy changes T cells to find and destroy glioblastoma cells.
Targeted Therapies
Targeted therapies aim at specific parts of glioblastoma. Bevacizumab is one therapy used for glioblastoma that comes back.
- These therapies are more precise than old treatments, which can mean fewer side effects.
- Researchers are finding new targets for therapy, like genetic changes in glioblastoma.
Tumor Treating Fields (TTFields)
TTFields use electric fields to stop cancer cells from dividing. It has helped patients live longer when used with other treatments.
- TTFields are worn on the scalp, making it a less invasive option.
- Trials are checking how well TTFields work at different stages of glioblastoma treatment.
Promising Research Directions
Research into glioblastoma is moving forward. There’s a focus on personalized medicine, tailoring treatments to each patient’s tumor.
The outlook for glioblastoma treatment is good. New treatments and trials are bringing hope to patients.
Quality of Life Considerations for Patients
Quality of life is key for those with glioblastoma. As the disease advances, patients face many challenges. These include managing symptoms, dealing with treatment side effects, and coping with brain and thinking changes.
Managing Symptoms and Side Effects
It’s important to manage symptoms and side effects well. This helps keep quality of life high. Personalized care plans that fit the patient’s health, preferences, and lifestyle can make a big difference.
Medications, therapies, and lifestyle changes are key in managing symptoms. For example, physical therapy can help with mobility and fatigue. Counseling supports mental health.
Neurological and Cognitive Changes
Glioblastoma and its treatment can cause brain and thinking changes. These include memory loss, speech difficulties, and changes in personality. It’s important for patients and their families to understand these changes.
Strategies like memory aids, cognitive rehabilitation, and support groups can help. Cognitive rehabilitation programs aim to help patients regain or compensate for lost thinking abilities.
Palliative Care Options
Palliative care helps with the symptoms and stress of serious illnesses like glioblastoma. It’s a key part of care, improving life quality for patients and their families.
Palliative care teams create care plans that meet each patient’s needs. This includes pain management, emotional support, and practical help. Palliative care can be given alongside treatments aimed at curing the disease.
Making Treatment Decisions
Choosing the right treatment is critical for glioblastoma patients. It’s about understanding the options, their benefits and risks, and how they match the patient’s values and goals.
Patients should talk openly with their healthcare team. This includes their oncologist, neurosurgeon, and palliative care specialists. This teamwork ensures treatment choices support the patient’s quality of life.
Support Resources for Patients and Families
For those dealing with glioblastoma, finding good support is key. The journey from diagnosis to treatment and beyond is tough. Having all the support you need is vital.
Financial and Insurance Considerations
Treatment for glioblastoma can be very expensive. Patients and their families face big medical bills and lost income. It’s important to know what insurance covers and to look for financial help.
- Reviewing insurance policies to understand what is covered
- Exploring patient assistance programs offered by pharmaceutical companies
- Seeking help from non-profit organizations that provide financial aid
Caregiver Support
Caregivers are essential for glioblastoma patients. But, caregiving can be very stressful. It’s important to have support for caregivers.
- Counseling and emotional support services
- Support groups for caregivers
- Respite care services to provide temporary relief
End-of-Life Planning
As the disease gets worse, planning for the end of life becomes more important. This includes deciding on treatment, palliative care, and hospice care.
Talking openly with healthcare providers and family is key. It helps make sure the patient’s wishes are followed.
Conclusion
Glioblastoma multiforme is the most aggressive brain cancer, with a poor prognosis. The survival rate varies based on age, health, and how much of the tumor is removed. It’s important for patients and families to understand glioblastoma to deal with diagnosis, treatment, and care.
The survival rate for glioblastoma patients is a big concern, with short median survival times. But, new treatments and clinical trials give hope for better survival rates. Advances in surgery, radiation, and chemotherapy, like the Stupp Protocol, show promise.
Research is finding new ways to fight glioblastoma by understanding its molecular and genetic roots. Patients and families need to stay updated and work with doctors to make the best care choices.
Knowing about glioblastoma and its treatments helps people cope with the disease. It can also improve their quality of life.
FAQ
What is glioblastoma cancer?
Glioblastoma, also known as glioblastoma multiforme (GBM), is the most aggressive brain cancer. It’s classified as a grade IV astrocytoma.
What are the symptoms of glioblastoma?
Symptoms include headaches, seizures, and confusion. You might also experience memory loss and changes in behavior.
How is glioblastoma diagnosed?
Doctors use MRI or CT scans for imaging. A biopsy is then done to confirm the presence of glioblastoma cells.
What is the prognosis for glioblastoma patients?
The prognosis is poor. Patients usually live about 15 months after diagnosis, despite aggressive treatment.
What are the standard treatment approaches for glioblastoma?
Treatment includes surgery, radiation, and chemotherapy. The Stupp protocol is often followed.
Can glioblastoma be cured?
Glioblastoma is currently considered incurable. But, treatments can manage symptoms and extend life in some cases.
What factors affect the survival rate of glioblastoma patients?
Survival depends on age, health, tumor location and size, and surgical extent. Molecular markers like MGMT promoter methylation also play a role.
Are there any emerging treatments for glioblastoma?
Yes, new treatments include immunotherapy, targeted therapies, and tumor treating fields (TTFields). These are being tested in clinical trials.
How does glioblastoma affect the body?
As glioblastoma progresses, it can cause neurological deficits and cognitive changes. It can also lead to life-threatening complications.
What support resources are available for glioblastoma patients and their families?
Support includes patient advocacy groups, financial help, caregiver support, and palliative care. These help manage symptoms and improve quality of life.
What is the typical timeline after a glioblastoma diagnosis?
The timeline varies, but most patients see rapid disease progression. The median survival time is about 15 months after diagnosis.
How can glioblastoma patients make informed treatment decisions?
Patients should talk to their healthcare team about treatment options. Consider the tumor’s characteristics, overall health, and the benefits and risks of treatments.
Referenes
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa043330





