Nearly 30% of patients who have surgery for a brain tumor worry about tumor regrowth a few years later brain tumor recurrence.
This scary fact makes many patients fear their tumor might come back after surgery.
The thought of recurrence is scary. But knowing what can cause it helps patients and doctors find ways to manage it.
Key Takeaways
- Understanding the risk factors for brain tumor recurrence is key.
- The chance of tumor regrowth depends on several things.
- Good management plans can lower the risk of recurrence.
- Patients should talk about their risk with their doctor.
- Regular check-ups are important to watch for tumor growth.
Understanding Brain Tumor Recurrence
Brain tumor recurrence is a big challenge in neuro-oncology. People worry a lot about whether a brain tumor can come back after surgery. This is a big concern for both patients and doctors.
Recurrence means a brain tumor comes back after treatment. This can happen even if the surgery seems to have worked. It’s important to understand this to help patients and plan follow-up treatments.
What Constitutes a Tumor Recurrence
Tumor recurrence happens when a brain tumor grows back in the same spot after treatment. This can happen with both good and bad brain tumors. How likely it is to happen depends on the tumor type, its grade, and how much was removed during surgery.
Benign brain tumors, such as meningiomas, can recur if they are not completely excised. Malignant brain tumors, like glioblastomas, are more likely to come back because they grow fast.
Differentiating Between Recurrence and Progression
It’s important to tell the difference between recurrence and progression. Progression means the tumor keeps growing even if some was removed. Recurrence means the tumor was controlled or gone but then comes back.
- Recurrence often means a new tumor grows where the old one was.
- Progression is when the tumor that was left keeps growing.
The Biological Basis of Tumor Regrowth
The reasons tumors grow back are complex. They involve how tumor cells and brain tissue interact. Studies on brain plasticity and function have helped us understand this.
| Biological Factor | Description | Impact on Recurrence |
| Tumor Microenvironment | The area around the tumor, including blood vessels and immune cells. | Affects how the tumor grows and comes back. |
| Genetic Mutations | Changes in tumor cell DNA that make them grow fast. | Can make it more likely for the tumor to come back. |
| Stem Cell Populations | Tumor cells that can keep the tumor going. | Helps the tumor come back and resist treatment. |
Knowing about these factors helps us find ways to stop or manage tumor recurrence. By studying tumor biology, we can improve care for brain tumor patients.
Types of Brain Tumors and Their Recurrence Rates
Brain tumors vary in how likely they are to come back. This depends on their type and what they are like. Knowing if a tumor is benign or malignant helps doctors figure out the chance of it coming back.
Benign Brain Tumor Recurrence Patterns
Even though benign brain tumors are not cancerous, they can come back if not all of it is removed. Tumors like meningiomas usually don’t come back often if they are removed completely. But, some can come back because of where they are or if not all of it was taken out.
Malignant Brain Tumor Regrowth Statistics
Malignant brain tumors, like glioblastomas, are more likely to come back than benign ones. Glioblastoma recurrence often happens within two years after treatment. This is because glioblastomas grow quickly and are hard to treat.
Comparing Recurrence Across Tumor Types
Looking at different tumors, malignant ones are more likely to come back than benign ones. Glioblastomas and other aggressive tumors are very hard to treat because they tend to come back. Knowing this helps doctors plan better treatment and care for patients.
Glioblastoma Recurrence: The Most Aggressive Form
Glioblastoma recurrence is a big problem in neuro-oncology. This tumor is very aggressive and hard to treat. It’s the most dangerous type of brain tumor, making treatment plans tough.
Factors Contributing to Recurrence
Glioblastomas often come back because they are very aggressive. Several factors contribute to this recurrence. For example, the tumor can spread into the brain, making it hard to remove completely. Also, glioblastoma cells can resist chemotherapy and radiation, making treatment harder.
The heterogeneous nature of glioblastoma also plays a big role. These tumors have different cell types, some of which are harder to treat. This diversity can lead to the survival of tumor cells that cause recurrence.
Timeline for Possible Recurrence
The time when glioblastoma might come back varies a lot. Mostly, it happens within the first two years after treatment. The timing depends on how much of the tumor was removed, how well the treatments worked, and the tumor’s genetic makeup.
- Early recurrence often means a more aggressive tumor.
- Late recurrence might happen in patients with better chances of survival.
Mechanisms of Treatment Resistance
Glioblastoma’s resistance to treatment comes from several sources. Key mechanisms include the tumor’s ability to fix DNA damage from radiation and chemotherapy. It also has cancer stem cells that are hard to kill and a tumor environment that helps it resist treatment.
It’s important to understand these mechanisms. This knowledge helps in finding new ways to treat glioblastoma better. It aims to improve outcomes and lower the chance of recurrence.
Meningioma Recurrence: What to Expect
Meningiomas can come back, and this depends on the tumor’s grade. These tumors are usually benign and grow from the meninges. Knowing when and how often they might come back is key to good care.
Recurrence Rates Based on Meningioma Grade
Meningiomas are graded from I (benign) to III (malignant). The chance of them coming back changes with the grade. Grade I meningiomas rarely come back, less than 10% after surgery. But, Grade II and III meningiomas are more likely to come back, needing stronger treatments.
| Meningioma Grade | Recurrence Rate | Typical Treatment Approach |
| Grade I | Less than 10% | Surgical resection, observation |
| Grade II | 20-40% | Surgery, radiation therapy |
| Grade III | 50-80% | Aggressive surgery, radiation, chemotherapy |
Long-term Surveillance Needs
Watching for meningioma return is key, more so for higher-grade ones. MRI scans are often used, with how often depending on the tumor and surgery. Catching a return early can make a big difference in treatment success.
Atypical and Malignant Meningioma Considerations
Atypical (Grade II) and malignant (Grade III) meningiomas are tough because they come back often and grow fast. Treatment might include surgery, radiation, and sometimes chemotherapy. Researchers are looking for new ways to fight these tumors.
Knowing your meningioma’s details is important for your care plan. Doctors consider the tumor’s grade, how much was removed, and your health. This helps them give you the best care possible.
Low Grade Glioma and Recurrence Patterns
It’s important to know how low-grade gliomas come back. These brain tumors might seem harmless at first but can grow back. Sometimes, they even turn into more serious tumors.
One big worry is that these tumors might turn into more dangerous types. Research shows many low-grade gliomas can change into higher-grade tumors. This often means the treatment plan needs to change.
Transformation Risk to Higher Grades
When low-grade gliomas turn into higher grades, it’s due to changes in their genes. Molecular profiling helps find tumors at risk of changing.
Several things can affect how likely a tumor is to change:
- IDH mutation status
- 1p/19q codeletion status
- Presence of other genetic mutations
Monitoring Protocols for Low Grade Gliomas
It’s key to watch these tumors closely for any signs of change. MRI scans are a main tool for keeping an eye on things. Sometimes, doctors also use other imaging methods and check how the patient is feeling.
Here’s a common plan for checking on these tumors:
| Time Post-Surgery | Monitoring Frequency |
| 0-6 months | Every 3 months |
| 6-24 months | Every 6 months |
| Beyond 24 months | Annually or as needed |
Molecular Markers Predicting Recurrence
Molecular markers are very important for guessing if a tumor will come back. IDH mutations and 1p/19q codeletion are two markers that help doctors know how well a tumor will respond to treatment.
Knowing about these markers helps doctors plan better treatments. This makes it easier to predict when a tumor might come back. It also helps doctors make better choices for their patients.
Metastatic Brain Tumors: Recurrence Considerations
It’s important to know what makes metastatic brain tumors come back. These tumors start in other parts of the body and can be hard to manage. They often come back, which is a big challenge in treating cancer.
Primary Cancer Influence on Recurrence
The type of cancer and its characteristics affect how likely a metastatic brain tumor will come back. For example, aggressive cancers like melanoma or lung cancer are more likely to spread to the brain again.
Studies have found that the genes in the original tumor can affect how the brain metastases behave. Some genetic changes can make the tumor harder to treat, raising the chance of it coming back.
Managing Multiple Metastatic Lesions
Dealing with many metastatic lesions in the brain is tough. It’s hard to treat several tumors at once. Doctors often use a mix of surgery, radiation, and other treatments.
- Surgery is usually for patients with a few tumors that are easy to reach.
- Stereotactic radiosurgery (SRS) works well for patients with many brain metastases.
- Whole-brain radiation therapy (WBRT) is used when there are lots of tumors or the cancer has spread a lot.
Systemic Disease Control and Brain Recurrence
Keeping the cancer under control is key to stopping metastatic brain tumors from coming back. Treating the original cancer well can lower the chance of more brain metastases.
“The interplay between systemic disease control and the risk of brain metastasis recurrence highlights the need for a complete treatment plan.”
New treatments like targeted therapy and immunotherapy are helping patients with metastatic disease. They show promise in bettering patient outcomes.
By understanding what makes tumors come back and using a variety of treatments, doctors can help patients live better lives.
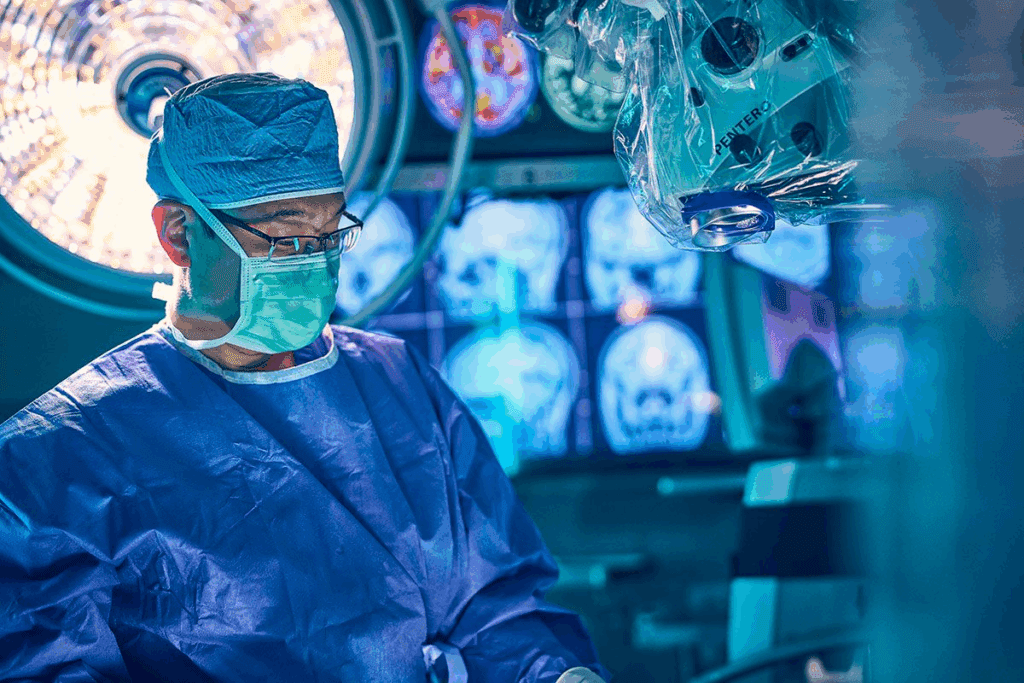
Surgical Factors Affecting Brain Tumor Recurrence
Surgery for brain tumors is a careful process. It aims to remove as much of the tumor as possible while keeping brain function intact. How much of the tumor is removed is key to preventing it from coming back.
Complete vs. Partial Resection Outcomes
Complete resection of brain tumors greatly improves patient outcomes. It lowers the chance of the tumor coming back. On the other hand, partial resection might leave tumor cells behind, leading to recurrence.
- Complete resection is linked to longer periods without tumor growth.
- Partial resection might be needed when tumors are in sensitive brain areas.
Tumor Margins and Their Significance
The state of tumor margins after surgery is very important. A clear margin means no tumor cells were found at the edge of the removed tissue. But, a positive margin suggests tumor cells might have been left behind.
- Clear margins are linked to lower recurrence rates.
- Positive margins might mean more treatments, like radiation therapy, are needed.
Advanced Surgical Techniques to Minimize Recurrence
New surgical methods, like intraoperative MRI and fluorescence-guided surgery, help remove tumors more completely. This reduces the risk of the tumor coming back.
| Technique | Description | Benefit |
| Intraoperative MRI | Real-time imaging during surgery | Ensures complete resection |
| Fluorescence-Guided Surgery | Visualization of tumor tissue using fluorescent dyes | Enhances tumor removal accuracy |
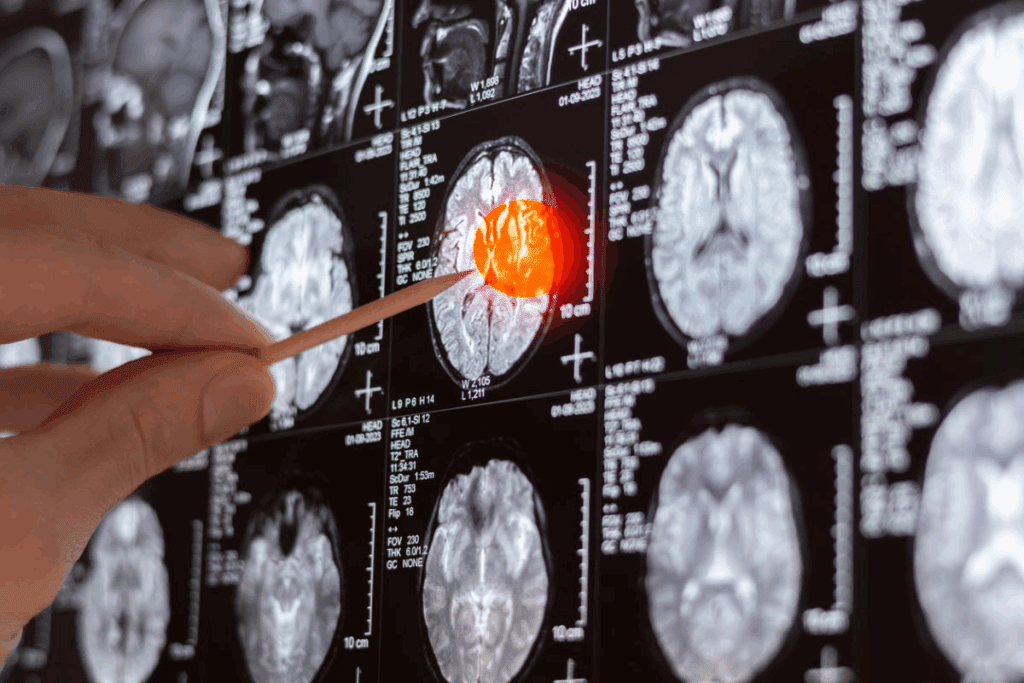
Post-Operative Imaging to Detect Residual Tumor
After surgery, imaging is key to check if all tumor was removed. It finds any tumor left behind, which is important for more treatment.
Immediate Post-Op MRI Protocols
Doctors do an MRI soon after surgery, usually in 24 to 48 hours. This is important to tell if it’s leftover tumor or just surgery changes. They use T1, T2, and contrast-enhanced images for a full view.
Key components of an immediate post-op MRI protocol include:
- Pre-contrast T1-weighted images to assess any hemorrhage or residual tumor.
- Post-contrast T1-weighted images to evaluate the extent of tumor resection.
- T2-weighted images to identify any edema or post-surgical changes.
Interpreting Post-Surgical Changes vs. Residual Tumor
Reading MRI scans after surgery is tricky because of changes like swelling and bleeding. Doctors must tell these apart from tumor to give a true report.
As noted by a study published in a reputable medical journal, “The accuracy of post-operative MRI in detecting residual tumor is highly dependent on the timing and quality of the imaging.”
Advanced Imaging Techniques for Recurrence Detection
Techniques like diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI), and magnetic resonance spectroscopy (MRS) offer more info than regular MRI. They help spot recurrence sooner and more accurately.
DWI spots areas where water moves slowly, which might mean tumor return. PWI looks at blood flow in the tumor. MRS gives metabolic details about the tumor.
“Advanced imaging has changed how we care for brain tumor patients,” says a top neuro-oncology expert. “It lets us find recurrence early, which can lead to better results.”
Adjuvant Therapy to Prevent Tumor Regrowth
Adjuvant therapies like radiation and chemotherapy are key in stopping brain tumors from coming back. After surgery, these treatments help get rid of any cancer cells left behind.
Radiation Therapy Approaches
Radiation therapy is a common treatment for brain tumors. It uses high-energy beams to kill cancer cells. There are two main types: external beam radiation therapy and stereotactic radiosurgery.
The choice of therapy depends on the tumor type and the patient’s health. External beam radiation therapy is given daily for several weeks. This method helps protect healthy brain tissue.
Chemotherapy Protocols
Chemotherapy is another treatment for brain tumors. It uses drugs to kill cancer cells. The drugs can be taken by mouth or given through an IV, depending on the plan.
Chemotherapy is often used with radiation therapy for brain tumors. The choice of chemotherapy depends on the tumor type, grade, and the patient’s health. Temozolomide is a common drug for glioblastoma.
Targeted Therapy Options
Targeted therapy is a treatment that focuses on tumor cells, reducing harm to healthy cells. It uses drugs that target specific molecular flaws in cancer cells.
Bevacizumab is a targeted therapy drug. It works by stopping tumors from making their own blood supply, a process called angiogenesis.
Molecular and Genetic Factors Influencing Recurrence Risk
Understanding the molecular and genetic factors that influence brain tumor recurrence risk is key. Recent research has found several important factors that affect recurrence likelihood.
Key Genetic Markers Associated with Recurrence
Specific genetic markers are linked to a higher risk of brain tumor recurrence. For example, mutations in the IDH1 and IDH2 genes can impact glioma prognosis. Certain molecular markers in meningiomas also suggest a higher recurrence risk.
Genetic profiling of brain tumors can spot these markers. This helps doctors better understand recurrence risk. It’s essential for creating personalized treatment plans.
How Molecular Profiling Guides Treatment
Molecular profiling analyzes a tumor’s genetic and molecular traits to guide treatment. By identifying specific genetic mutations, doctors can choose the best targeted therapy. This approach has shown to improve outcomes for patients with recurrent brain tumors.
For instance, tumors with certain mutations may respond better to specific chemotherapies. Molecular profiling helps find these mutations, guiding treatment choices.
Emerging Biomarkers for Recurrence Prediction
Research is ongoing to find new biomarkers for predicting brain tumor recurrence. These could include genetic mutations, gene expression changes, or other molecular traits.
Finding reliable biomarkers for recurrence risk could greatly improve brain tumor management. It could lead to earlier interventions and better patient outcomes. As research continues, new biomarkers are likely to be discovered, helping us better predict and manage recurrence.
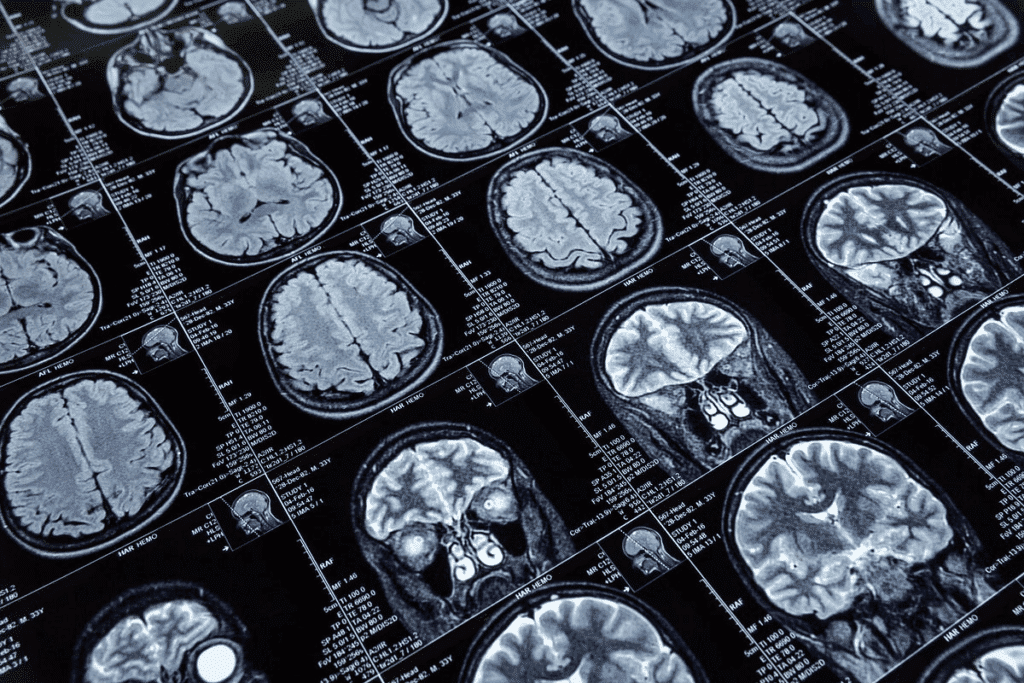
Tumor Follow-Up Protocols After Surgery
The journey doesn’t end after brain tumor surgery. A structured follow-up plan is key to catch any signs of recurrence early. After surgery, patients must follow a strict follow-up protocol to closely monitor their condition.
Short-term Monitoring Schedule
In the short term, patients have regular imaging tests like MRI or CT scans. These tests check for any remaining tumor or signs of recurrence. The scan frequency depends on the tumor type, grade, and the patient’s health.
Short-term follow-up is vital for spotting immediate complications or remaining disease. During this time, patients see their healthcare provider often. They might visit every few weeks to check on their recovery and adjust treatment plans as needed.
Long-term Surveillance Recommendations
Long-term surveillance is also key to catch late recurrences. The follow-up schedule can last for years. The visits and imaging tests decrease over time if there’s no sign of recurrence.
For long-term surveillance, annual or bi-annual MRI scans are common. Patients also have regular check-ups with neurosurgeons or oncologists. This ongoing monitoring is essential for catching any recurrence early, when it’s easier to treat.
Tumor Surveillance Technology Advancements
New imaging technologies have greatly improved early detection of tumor recurrence. Functional MRI, PET scans, and diffusion tensor imaging offer detailed insights into tumors and brain tissue.
| Technology | Description | Benefits |
| Functional MRI | Maps brain function and activity | Helps in identifying tumor location and impact on brain function |
| PET Scans | Measures metabolic activity | Useful in detecting recurrence by highlighting areas of high metabolic activity |
| Diffusion Tensor Imaging | Visualizes white matter tracts | Aids in surgical planning by mapping critical brain structures |
These advancements in tumor surveillance technology have made follow-up care more precise. Healthcare providers can now tailor treatment plans better to meet each patient’s needs.
Signs and Symptoms of Brain Tumor Recurrence
Spotting the signs of brain tumor recurrence early is key to better treatment results. Brain tumors can come back in different ways. It’s important for patients to know the possible signs.
Neurological Indicators
Neurological symptoms are often the first signs of brain tumor recurrence. These can include:
- Headaches that worsen over time
- Seizures, if they are new or different from before
- Weakness or numbness in the arms or legs
- Changes in vision, speech, or thinking
Differentiating Treatment Effects from Recurrence
Telling treatment effects from tumor recurrence is hard but very important. Treatment effects, like radiation necrosis, can look like tumor recurrence on scans.
| Characteristics | Treatment Effects | Tumor Recurrence |
| Imaging Features | Often shows necrosis or inflammation | Typically shows enhancement with contrast |
| Clinical Presentation | May present with similar neurological symptoms | Often presents with progressive neurological decline |
Advanced imaging, like perfusion-weighted MRI, can help tell these apart.
Managing Recurrent Brain Tumors
Recurrent brain tumors are a big challenge. They need a treatment plan that looks at many things. This includes the tumor type, where it is, and the patient’s health.
Second Surgery Considerations
Thinking about a second surgery for brain tumors involves many factors. These include the tumor’s size, where it is, and the patient’s past surgeries. A detailed check is key to see if a second surgery is a good idea.
- Looking at if the tumor can be removed
- Checking the patient’s brain health
- Thinking about past treatments and how they worked
Alternative Treatments for Recurrent Tumors
If a second surgery isn’t right, other treatments are important. These can be radiation therapy, chemotherapy, or targeted therapy. The right treatment depends on the tumor and the patient’s health.
- Using radiation to kill tumor cells
- Chemotherapy to slow tumor growth
- Targeted therapy for specific tumor traits
Clinical Trials for Recurrent Disease
Clinical trials are a hope for treating brain tumors that come back. They test new treatments and drugs. Joining clinical trials can be a good choice for patients with recurring tumors.
- Trying new treatments
- Helping with medical research
- Chance for better treatment results
Quality of Life After Recurrence
After a brain tumor comes back, the main goal is to improve quality of life. This means focusing on supportive care, palliative treatments, and mental health support. It’s all about meeting the needs of patients and their families.
Supportive Care Approaches
Supportive care is key in managing symptoms and side effects of a brain tumor recurrence. It’s tailored to each person and might include physical therapy to improve strength and mobility. Occupational therapy helps with daily tasks, and speech therapy aids in communication.
Good nutrition is also important. It helps manage symptoms and supports overall health. Doctors might suggest a special diet or supplements based on the patient’s needs.
Palliative Interventions
Palliative care focuses on easing symptoms and stress from serious illnesses like brain tumors. It includes pain management, managing neurological symptoms, and emotional support.
Palliative care teams work with the patient’s oncologist and other doctors. They aim to provide complete care for the patient’s well-being.
Psychological Support for Patients and Families
The emotional impact of a brain tumor recurrence is big. It affects not just the patient but also their family and caregivers. Getting psychological support is vital to deal with these challenges.
This support can be in many ways, like individual counseling, family therapy, and support groups. These help patients and their families handle the tough emotions of recurrence. They build resilience and enhance quality of life.
In summary, improving quality of life after a brain tumor recurrence needs a full approach. This includes supportive care, palliative treatments, and mental health support. By meeting the needs of patients and their families, healthcare providers can greatly enhance their quality of life during this tough time.
Prognosis After Brain Tumor Recurrence
When a brain tumor comes back, many things affect how well a person will do. This includes the type of tumor and any treatments they’ve had. Knowing these details helps both patients and doctors make better choices for future care.
Survival Statistics by Tumor Type
How long someone might live after a brain tumor comes back depends a lot on the tumor type. For example, glioblastoma is very aggressive and has a worse outlook than meningiomas, which are usually not cancerous.
| Tumor Type | Median Survival After Recurrence |
| Glioblastoma | 6-12 months |
| Meningioma (Benign) | 5-10 years |
| Low Grade Glioma | 2-5 years |
Factors That Improve Outcomes
There are a few things that can help someone do better after a brain tumor comes back. These include catching the tumor early, how well the first treatment worked, and the patient’s overall health.
- Early detection and intervention
- Aggressive treatment strategies
- Participation in clinical trials
Case Studies of Long-term Survivors
There are stories of people living a long time after their brain tumor came back. This is often because of good treatment and the tumor’s nature.
Surviving a long time often means the tumor was not very aggressive and the person responded well to treatment. More research is needed to help more people live longer after a brain tumor recurrence.
Conclusion: Living with the Possibility of Recurrence
It’s important for patients who have had brain tumor surgery to know about the risk of it coming back. Even if treatment seems to work, the tumor can grow again. So, it’s key to keep watching for any signs.
Patients need to stay in touch with their doctors to catch any problems early. This means watching for changes in how they feel or new symptoms. Regular check-ups and scans are a big part of taking care of yourself after surgery.
Dealing with the chance of the tumor coming back means being active. By keeping up with your care plan and following your doctor’s advice, you can handle any issues quickly. This helps you stay on top of your health.
New medical discoveries and treatments are helping people with brain tumors. Keeping up with these advancements and joining clinical trials can offer new hope. It might also lead to better ways to manage the tumor.
FAQ
What is brain tumor recurrence?
Brain tumor recurrence happens when a tumor grows back after treatment. This can happen with both benign and malignant tumors. Treatments include surgery, radiation, or chemotherapy.
How does recurrence differ from progression?
Recurrence means a tumor grows back after treatment. Progression is when a tumor keeps growing even with treatment.
What are the chances of a benign brain tumor recurring?
The chance of a benign tumor coming back depends on the tumor type and how well it was removed. Some, like meningiomas, rarely come back if fully removed.
Why do glioblastomas commonly recur?
Glioblastomas are aggressive and hard to treat. They often come back because they spread and can resist treatment.
How is meningioma recurrence managed?
Managing meningioma recurrence involves regular check-ups and imaging. Sometimes, more surgery or radiation is needed, mainly for atypical or malignant types.
What is the risk of low-grade glioma transforming to a higher grade?
Low-grade gliomas can turn into more serious ones over time. Regular checks with imaging and tests can spot this early.
How does the primary cancer influence metastatic brain tumor recurrence?
The type and stage of the primary cancer affect the risk of brain tumor recurrence. Controlling the main cancer is key to preventing brain recurrence.
What is the significance of tumor margins in surgery?
Tumor margins are the edges of the tumor and surrounding tissue removed. Clear margins are important to lower recurrence risk.
How is post-operative imaging used to detect residual tumor?
Imaging, like MRI, after surgery checks how much tumor was removed. It also finds any left behind, guiding further treatment.
What adjuvant therapies are used to prevent tumor regrowth?
Adjuvant therapies, like radiation and chemotherapy, prevent tumor growth. They are chosen based on the tumor type and molecular characteristics.
How do molecular and genetic factors influence recurrence risk?
Molecular and genetic factors, like specific mutations, affect recurrence risk. Molecular profiling helps guide treatment and find new biomarkers for prediction.
What is the importance of follow-up protocols after surgery?
Follow-up protocols, including regular imaging and check-ups, are vital. They help catch recurrence early and improve outcomes.
What are the signs and symptoms of brain tumor recurrence?
Signs of recurrence include neurological problems, seizures, and cognitive changes. It’s important to tell these apart from treatment effects.
How is recurrent brain tumor managed?
Managing recurrent brain tumors involves a team effort. This includes second surgeries, alternative treatments, and clinical trials. Treatment plans are tailored to each patient.
What is the prognosis after brain tumor recurrence?
The prognosis after recurrence depends on the tumor type, how much it has come back, and previous treatments. It’s influenced by molecular characteristics and overall health.
How can quality of life be maintained after recurrence?
Quality of life can be kept up with supportive care, palliative interventions, and psychological support. This helps patients and their families.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S0140673605674924

































