Cancer diagnosis has become more precise with advancements in medical imaging, especially with techniques like breast MRI sensitivity improving detection rates. Early detection is key for effective treatment.
Did you know that nearly 1 in 8 women will develop invasive breast cancer in their lifetime? Accurate diagnosis is vital for improving survival rates.
We understand the importance of accurate diagnosis in cancer treatment. Our goal is to provide detailed information on the most effective diagnostic imaging techniques.
Key Takeaways
- Advanced imaging techniques improve cancer detection rates.
- Diagnostic imaging plays a critical role in cancer diagnosis.
- Early detection significantly enhances treatment outcomes.
- We provide detailed information on cancer detection methods.
- Accurate diagnosis is key to effective cancer treatment.
Understanding Cancer Imaging: An Overview
Medical imaging is key in fighting cancer. It helps find, diagnose, and track how well treatments work. We use different imaging methods to see inside the body and spot problems.
Medical imaging has changed cancer care a lot. It gives accurate diagnoses and helps decide on treatments. Doctors can look inside the body without surgery, find tumors, and learn about them.
The Role of Medical Imaging in Cancer Care
Medical imaging is important in cancer care. It helps find cancer early, see how big it is, and check if treatments are working. This info helps doctors choose the best treatments, like surgery or chemotherapy.
We use X-rays, CT scans, MRI, and PET scans for different things. Each has its own strengths and weaknesses. Choosing the right one helps get better results and care for patients.
Accuracy Metrics: Sensitivity, Specificity, and Predictive Values
We look at sensitivity, specificity, and predictive values to see how good cancer imaging is. These numbers tell us how accurate a test is.
| Metric | Description |
| Sensitivity | The ability of a test to correctly identify those with cancer (true positive rate) |
| Specificity | The ability of a test to correctly identify those without cancer (true negative rate) |
| Positive Predictive Value (PPV) | The probability that a positive test result indicates actual cancer |
| Negative Predictive Value (NPV) | The probability that a negative test result indicates the absence of cancer |
Knowing these metrics is key to understanding imaging results. It helps doctors make better choices for patients. This way, we can improve how we diagnose and treat cancer.
Anatomical vs. Functional Imaging Techniques
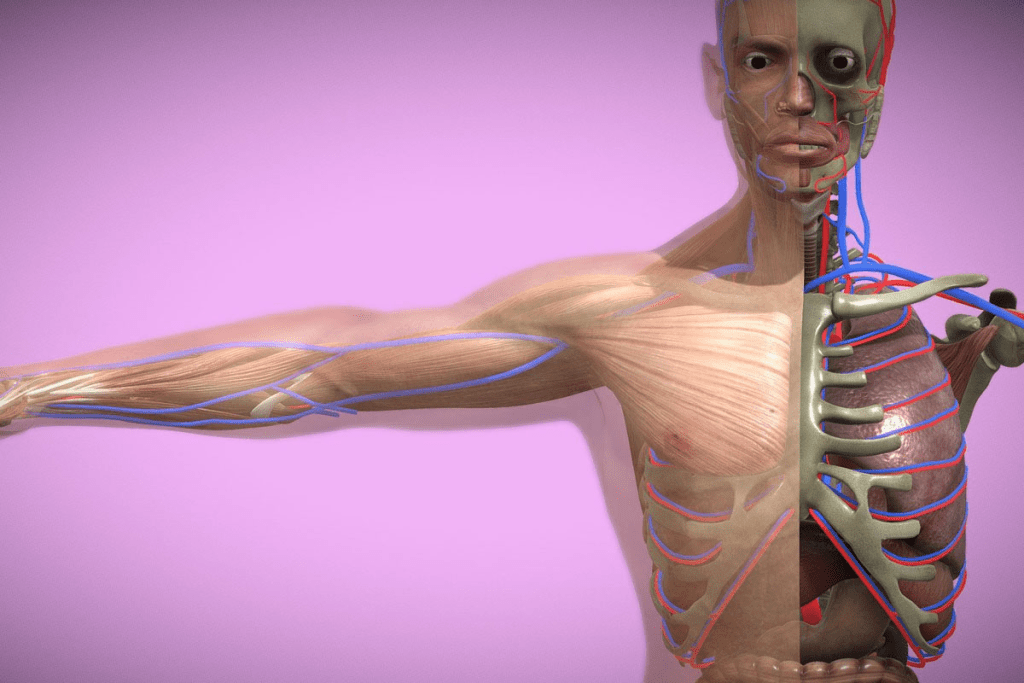
Medical professionals use anatomical or functional imaging to diagnose cancer. Each method has its own benefits. The choice depends on the cancer type, stage, and the patient’s health.
How Anatomical Imaging Works
Anatomical imaging, like CT scans and MRI, shows the body’s internal structures. It helps doctors find tumors, measure their size, and locate them. This method is great for spotting big tumors in places like the breast, lung, or liver.
“Anatomical imaging has changed cancer diagnosis by showing tumors and tissues clearly,” says an oncologist. “But it can’t always tell if a lesion is cancerous or not.”
The Value of Functional Imaging in Cancer Detection
Functional imaging, like PET scans, looks at the body’s metabolic activity. It spots cancer cells even when they’re small. This is key for catching cancer early and checking how treatments work.
Functional imaging also helps tell cancerous tissues from non-cancerous ones. This means fewer invasive biopsies are needed. “Adding functional imaging to cancer diagnosis has greatly improved our ability to accurately stage cancer and create personalized treatment plans,” says a radiologist.
When to Use Each Approach
Choosing between anatomical and functional imaging depends on the situation. Anatomical imaging is good for first screenings and finding tumors. Functional imaging is better for checking tumor activity and treatment success.
- Anatomical imaging is ideal for detecting tumors and assessing their size and location.
- Functional imaging is better suited for evaluating the metabolic activity of tumors and monitoring treatment response.
- A combination of both approaches often provides a more complete understanding of the cancer’s extent and behavior.
Knowing the strengths and limits of each imaging type helps doctors choose the best diagnostic path for each patient.
X-Ray and Mammography: Traditional Cancer Detection
For a long time, X-ray and mammography have been key in finding cancer. They help doctors make important treatment plans.
Limitations of Conventional X-Ray Technology
X-ray tech has its limits in finding cancer. It shows the breast in two dimensions, which can hide problems. It also struggles with dense breast tissue, making it hard to see details.
New X-ray tech has improved, but it’s not perfect. It can lead to false alarms and needs more tests to confirm findings.
Digital Mammography Advancements
Digital mammography has changed the game in breast cancer detection. It offers better image quality and helps doctors spot problems more easily. This tech turns X-ray images into digital signals for clearer views.
It’s been shown to find more cancers, even in dense breasts. Digital mammography gives doctors a clearer look, helping them catch what film-screen mammography might miss.
3D Mammography (Tomosynthesis)
3D mammography, or tomosynthesis, is a big step forward. It creates a 3D image of the breast, showing more detail. This helps doctors see through overlapping tissue, making it easier to find problems.
Research shows 3D mammography finds more cancers and fewer false alarms. It’s a big help for women with dense breasts, giving a clearer view of their breast anatomy.
Computed Tomography (CT) in Cancer Diagnosis
Computed Tomography (CT) is a key tool in fighting cancer. It lets doctors see tumors and how far cancer has spread. CT scans give us detailed images of the body, helping us find and understand cancer.
Standard CT Protocols for Cancer Staging
Standard CT protocols are key for cancer staging. We follow strict guidelines to get the best images. This helps us see tumor size, location, and if it has spread.
Contrast agents make tumors stand out more in CT scans. This is vital for knowing the cancer stage and treatment plans.
| Cancer Type | CT Protocol | Contrast Agent Use |
| Lung Cancer | Low-dose CT | Optional |
| Colorectal Cancer | Standard abdominal CT | Required |
| Liver Cancer | Multiphasic CT | Required |
Low-Dose CT Screening for Lung Cancer
Low-dose CT scans are great for catching lung cancer early. They’re recommended for those who have smoked a lot. This can help lower lung cancer deaths.
These scans use less radiation than regular CT scans. But, we must think about the risks, like false positives and radiation.
CT Limitations and Radiation Concerns
CT scans are powerful but have limits. We must think about radiation risks, mainly for young patients or those getting many scans. We’re working to lower radiation doses without losing image quality.
CT scans might not always tell the difference between cancer and non-cancer. This can lead to extra tests or biopsies. We’re always improving our methods to be more accurate and safe.
Knowing what CT scans can and can’t do helps us fight cancer better. As technology gets better, CT scans will keep being a big part of cancer care.
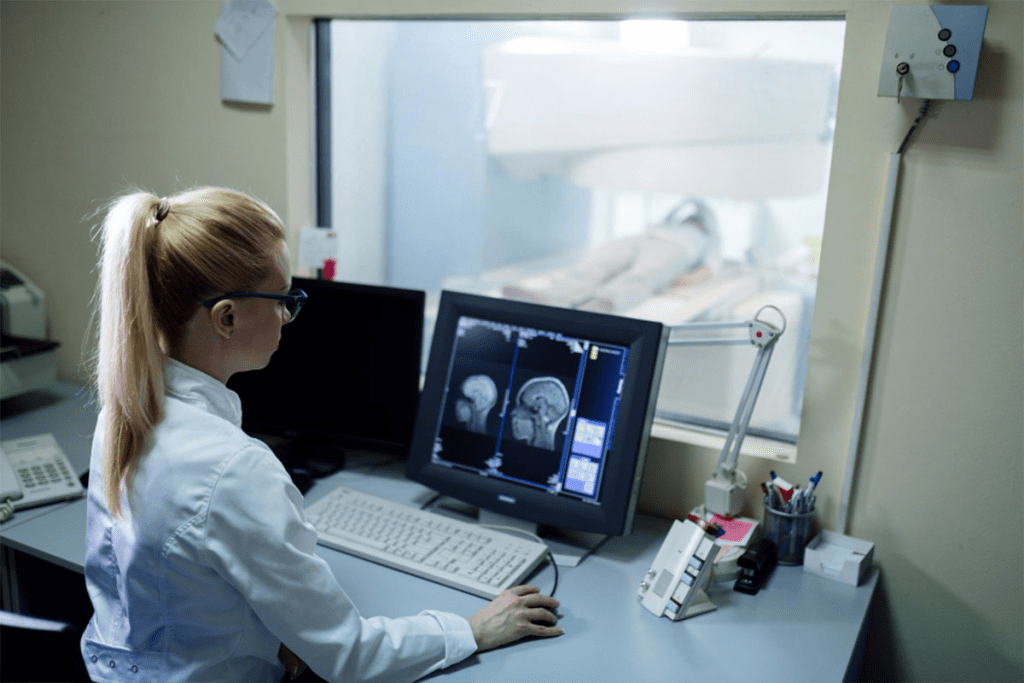
Magnetic Resonance Imaging (MRI) Fundamentals
MRI is a non-invasive way to see inside the body. It helps doctors find and track many health issues, like cancer. MRI makes detailed pictures of the inside without using harmful radiation. This makes it a key tool in fighting cancer.
How MRI Visualizes Tissue Differences
MRI works by using nuclear magnetic resonance. It uses a strong magnetic field to align hydrogen nuclei in the body. Then, radiofrequency pulses disturb this alignment, causing the nuclei to emit signals.
The contrast between different tissues is based on variations in proton density and relaxation times. This lets MRI show the differences between healthy and sick tissues.
Contrast Enhancement in Cancer Imaging
Contrast agents, like gadolinium-based compounds, are used in MRI. They change how nearby hydrogen nuclei behave, making different tissues stand out more. In cancer imaging, contrast-enhanced MRI helps in delineating tumor boundaries, assessing tumor vascularity, and monitoring treatment response. This has made MRI much better at finding and understanding cancers.
“The use of MRI in cancer diagnosis has revolutionized our ability to detect and stage cancer, providing critical information that guides treatment decisions.” – An Oncologist
Multiparametric MRI Applications
Multiparametric MRI uses many imaging sequences to get a full picture of tissue characteristics. It’s very useful in cancer imaging, helping to spot and understand tumors. By combining different MRI sequences, such as T1-weighted, T2-weighted, diffusion-weighted imaging, and dynamic contrast-enhanced MRI, we can obtain detailed information about tumor morphology, cellularity, and vascularity. This approach has shown to improve how accurately MRI can diagnose and guide treatment.
| MRI Sequence | Information Provided | Clinical Application |
| T1-weighted | Anatomical detail, fat suppression | Tumor detection, assessing lymph nodes |
| T2-weighted | Water content, edema | Detecting tumors, assessing tissue inflammation |
| Diffusion-weighted | Tissue cellularity, water diffusion | Detecting malignant tumors, assessing treatment response |
| Dynamic Contrast-enhanced | Tissue vascularity, perfusion | Assessing tumor angiogenesis, monitoring treatment response |
Breast MRI Sensitivity: The Gold Standard for Breast Cancer Detection
Breast MRI is top-notch for finding breast cancer, thanks to its high sensitivity. It’s great for spotting cancer in dense breast tissue. This makes it a key tool for those at high risk.
Detection Rates Compared to Other Modalities
Breast MRI finds more breast cancers than mammography and ultrasound. It’s better at catching cancers that other tests miss. This makes it a must-have for screening high-risk groups.
A study showed MRI found 93% of cancers in high-risk women. Mammography only found 33%. This shows MRI is better at finding cancers early.
Sensitivity in Dense Breast Tissue
Breast MRI shines when it comes to dense breast tissue. Dense tissue can hide tumors on mammograms. But MRI can see through it.
Studies show MRI is much better at finding cancers in dense tissue. This makes it a top choice for women with dense breasts.
Specificity Challenges and False Positives
Even though MRI is great at finding cancers, it can also lead to false positives. False positives mean more biopsies and worry for patients.
To deal with this, we use advanced imaging and strict rules. Despite the issues, MRI’s benefits for high-risk groups are worth it.
Current Guidelines for Breast MRI Screening
Guidelines suggest MRI for women at high risk of breast cancer. These guidelines look at family history and genetic risk.
We stick to these guidelines to make sure our patients get the right screening. High-risk women should get an MRI every year, starting at 25 or sooner based on risk.
MRI Breast Imaging: Technical Considerations
The quality of MRI breast imaging depends on several technical aspects. These include optimizing the protocol and using the right contrast agents. We will look into these factors and how they affect accuracy.
Breast MRI Protocol Optimization
Getting high-quality images for accurate diagnosis is key. Important factors include the magnetic field strength, coil design, and imaging sequences. We use high-field MRI systems (1.5T or 3T) for better image quality.
The protocol must match the clinical question. This could be finding breast cancer, seeing how far it has spread, or checking treatment progress. Changing parameters like slice thickness and field of view can greatly improve image quality.
Contrast Agents for Breast MRI
Contrast agents are essential for making lesions more visible in breast MRI. Gadolinium-based contrast agents (GBCAs) are often used because they highlight areas with more blood flow, common in cancer.
The choice of contrast agent and how much to use can impact accuracy. We consider the patient’s kidney function and any allergies when picking a contrast agent.
Interpretation Challenges and Solutions
Reading breast MRI images can be tough due to the complex anatomy and varied appearances. Key challenges include telling benign from malignant lesions, measuring size and extent, and avoiding false positives.
To overcome these, we use advanced techniques like diffusion-weighted imaging and dynamic contrast-enhanced MRI. Working together with radiologists, surgeons, and oncologists is also vital for accurate diagnosis and treatment planning.
Positron Emission Tomography (PET) Technology
PET technology gives us a special look at how tumors work. It helps find cancer and plan treatments. This tool is key in fighting cancer, giving us insights that other images can’t.
FDG-PET: Tracking Cancer Metabolism
FDG-PET uses a special sugar that cancer cells love. It shows where cancer is by seeing how much sugar it uses. This helps doctors find and check on tumors.
Key applications of FDG-PET include:
- Cancer staging and restaging
- Monitoring response to treatment
- Detecting recurrence
PSMA-PET for Prostate Cancer
PSMA-PET is great for finding prostate cancer. It looks for a protein that prostate cancer cells make a lot of. This helps doctors find cancer spots very accurately.
| Feature | FDG-PET | PSMA-PET |
| Target | Glucose metabolism | PSMA expression |
| Primary Use | Various cancers | Prostate cancer |
Other Specialized PET Tracers
New PET tracers are being made to find different things in cancer. For example, FET-PET looks at brain tumors. FAPI-PET finds proteins in tumor growth.
“The development of new PET tracers continues to expand the capabilities of PET imaging, allowing for more precise characterization of tumors and personalized treatment planning.”
” Expert in Nuclear Medicine
PET technology is a big help in fighting cancer. As we learn more, PET imaging will get even better. This will help doctors treat cancer more effectively.
Hybrid Imaging: PET/CT and PET/MRI
Hybrid imaging like PET/CT and PET/MRI combines different imaging types. This helps in better cancer staging and treatment planning. We’ll see how these methods work together to improve diagnosis.
The Synergy of Combined Modalities
Hybrid imaging mixes PET’s metabolic info with CT or MRI’s body details. This mix gives a deeper look into tumor biology and behavior.
Key benefits of hybrid imaging include:
- Improved diagnostic accuracy
- Enhanced tumor localization
- Better assessment of treatment response
- More precise staging of cancer
PET/CT for Cancer Staging
PET/CT is key in cancer staging. It offers both metabolic and anatomical info. We use it to see how far cancer has spread and to guide treatment.
The advantages of PET/CT in cancer staging are:
- Accurate detection of primary and metastatic tumors
- Assessment of tumor viability and response to treatment
- Guidance for biopsy and surgical planning
Emerging PET/MRI Applications
PET/MRI combines PET’s info with MRI’s soft-tissue contrast. It’s showing promise in cancers like brain, prostate, and liver. MRI’s strengths are key here.
The benefits of PET/MRI include:
- Reduced radiation exposure compared to PET/CT
- Improved characterization of soft-tissue tumors
- Enhanced assessment of complex anatomical regions
As hybrid imaging grows, we’ll see better cancer diagnosis and treatment. Using multiple modalities, we aim for more accurate and personalized care for patients.
Ultrasound Technology in Cancer Detection
Ultrasound technology has made a big leap in finding and diagnosing cancer. It’s a key tool for spotting and figuring out different types of cancer.
Capabilities of Conventional Ultrasound
Conventional ultrasound gives us live images of what’s inside our bodies. It’s great for checking on organs like the liver, pancreas, and thyroid.
We use it to look at tumors’ size, shape, and how they feel. We also see how they fit with the tissues around them.
Advanced Techniques: Elastography
Elastography is a fancy ultrasound trick that checks how stiff tissues are. Stiffer tissues might be cancerous.
We use elastography to make ultrasound better, when regular images aren’t clear enough.
Contrast-Enhanced Ultrasound Applications
Contrast-enhanced ultrasound (CEUS) uses tiny bubbles to make images clearer. It helps us see how tumors are getting blood and nutrients.
We use CEUS to figure out what liver spots are, see how treatments are working, and help with procedures.
| Ultrasound Technique | Application | Benefits |
| Conventional Ultrasound | Initial assessment of tumors | Real-time imaging, widely available |
| Elastography | Tissue stiffness assessment | Improved diagnostic accuracy for malignant lesions |
| Contrast-Enhanced Ultrasound | Tumor vascularity and perfusion assessment | Enhanced visualization, improved characterization of lesions |
Liver Cancer Imaging: The Role of Contrast-Enhanced MRI
Contrast-enhanced MRI is key in liver cancer imaging. It gives us detailed views of tumors. This helps in making accurate diagnoses and planning treatments.
Liver-Specific Contrast Agents
Liver-specific contrast agents make liver lesions more visible. They stick well to liver tissue, helping us see tumor edges and sizes more clearly.
These agents are great for spotting small liver tumors. They greatly improve how well we can diagnose liver cancer.
Detection Accuracy for Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the main type of liver cancer. Accurate detection is key for treatment. MRI with liver-specific contrast agents is very good at finding HCC.
MRI’s accuracy in finding HCC comes from its detailed views of tumor shape, blood flow, and liver function. This info is vital for planning treatment.
MRI vs. CT for Liver Metastases
Both MRI and CT scans are used for liver metastases. MRI is better at showing liver lesions because of its high detail and use of liver-specific agents.
Compared to CT, MRI is better at finding and describing liver metastases. But CT is useful for initial checks and staging because it’s widely available and quick.
Screening vs. Diagnostic Imaging: Different Purposes
The world of cancer imaging is split into screening and diagnostic imaging. Screening aims to find cancer in people who don’t show symptoms. It’s about catching cancer early. Diagnostic imaging, on the other hand, looks at symptoms or findings from screening. It helps doctors decide on treatment.
Cancer Screening Programs and Modalities
Cancer screening programs are key for finding cancer early. This can lead to better treatment and survival rates. Modalities like mammography for breast cancer, low-dose CT for lung cancer, and colonoscopy for colorectal cancer are common. These are mainly for people at higher risk or over a certain age.
Mammography is often used for breast cancer screening. It’s recommended for women over 40 every year. Low-dose CT scans are suggested for lung cancer in heavy smokers or those with a long smoking history.
Diagnostic Workup After Positive Screening
If a screening test shows something abnormal, a diagnostic workup follows. This aims to confirm cancer and understand how far it has spread. Tests like MRI, CT, or PET scans are used, along with biopsy for tissue samples.
The type of imaging used depends on the suspected cancer type, location, and the patient’s health. For example, a woman with a suspicious mammogram might get a breast MRI before a biopsy.
Risk-Benefit Analysis of Different Approaches
Screening and diagnostic imaging both have benefits and risks. Screening can catch cancer early, saving lives, but it can also lead to false positives. This causes unnecessary worry and more tests. Diagnostic imaging is key for treatment planning but involves radiation and possible complications from contrast agents.
It’s important to weigh the risks and benefits for each patient. This includes looking at age, cancer risk, and symptoms. This helps tailor imaging to each person’s needs, aiming for the best results with the least risk.
In summary, knowing the differences between screening and diagnostic imaging is vital for managing cancer. By choosing and using these imaging methods wisely, doctors can improve patient care and life quality.
Choosing the Right Scan: Cancer-Specific Considerations
Getting the right imaging scan is key for cancer diagnosis. The right scan depends on the cancer type. Each cancer acts differently, so knowing these differences is important.
Breast Cancer: Mammography vs. MRI vs. Ultrasound
Choosing between mammography, MRI, and ultrasound for breast cancer depends on several things. These include the patient’s risk and breast density. Mammography is common for screening but works less well in dense breasts.
Mammography is good for finding calcifications and tumors in older women. But it’s not as good in dense breasts.
MRI is very sensitive, great for high-risk patients or those with dense breasts. It helps see how far the disease has spread and how well treatments are working.
Ultrasound is often used with mammography. It helps figure out what a lesion is and guides biopsies.
| Imaging Modality | Sensitivity | Specificity | Common Use |
| Mammography | Moderate | High | Screening |
| MRI | High | Moderate | High-risk screening, extent of disease |
| Ultrasound | Moderate | High | Lesion characterization, biopsy guidance |
Lung Cancer: CT vs. PET/CT
For lung cancer, CT and PET/CT are key. CT shows the body’s structure, while PET/CT shows how active tumors are.
CT is great for finding tumors and seeing their size and location. Low-dose CT is recommended for lung cancer screening in high-risk groups.
PET/CT combines CT’s structure with PET’s metabolic activity. This helps spot malignant tumors and see how far the disease has spread.
“The use of PET/CT in lung cancer staging has significantly improved the accuracy of detecting distant metastases, influencing treatment decisions.”
Prostate Cancer: Multiparametric MRI vs. PSMA-PET
In prostate cancer, multiparametric MRI and PSMA-PET are becoming key for diagnosis and staging. MRI gives detailed prostate gland info, helping spot and stage tumors.
PSMA-PET is great for finding metastatic disease. It’s very sensitive for spotting prostate cancer spread to lymph nodes and bones.
Colorectal Cancer: CT Colonography vs. Conventional Imaging
For colorectal cancer, CT colonography and conventional imaging (like CT scans) are used. CT colonography is a special CT scan for the colon and rectum.
CT colonography is good for finding polyps and tumors in the colon. It’s less invasive than traditional colonoscopy and can be an option for those who can’t have colonoscopy.
Conventional CT scans are used for staging and seeing if colorectal cancer has spread to other parts of the body.
Biopsy: The Definitive Gold Standard
Imaging techniques have changed how we find cancer. But, biopsy is the only way to know for sure. Tools like CT, MRI, and PET scans show where tumors are and how big they are. Yet, they can’t always tell if a spot is cancer.
Biopsy gives us tissue samples to check for cancer. This is key for planning treatment.
When Imaging Isn’t Enough
Imaging alone can’t always tell if a tumor is cancer. Some tumors look like normal spots on scans. A biopsy is needed to be sure.
Even if scans suggest cancer, a biopsy confirms it. Knowing the exact cancer type helps doctors choose the right treatment.
Image-Guided Biopsy Techniques
Image-guided biopsy makes getting tissue samples safer and more accurate. Using ultrasound, CT, or MRI, we can aim right at the tumor. This lowers the chance of mistakes.
These methods also help avoid harming nearby important areas. Image-guided biopsy is a key part of cancer diagnosis today. It lets us get good tissue samples without a big cut.
Liquid Biopsy: A Complementary Approach
Liquid biopsy is a new way to check for cancer. It looks at DNA or biomarkers in blood or fluids. It’s not a full replacement for tissue biopsy yet.
But, liquid biopsy is non-invasive and gives quick updates on tumors. It’s useful for tracking how well treatments work and finding new cancer types.
Conclusion: The Future of Cancer Detection
Diagnostic imaging is key in finding cancer early and treating it. MRI, CT scans, and PET scans have made diagnosing cancer more accurate. This has greatly helped doctors in treating the disease.
New methods like PET/CT and PET/MRI are making diagnosis even better. These new tools help doctors find cancer more precisely. This leads to better treatments for patients.
Research is making cancer diagnosis even more advanced. We can expect even better tools in the future. These will help patients get better care and outcomes.
Healthcare providers are working hard to use the latest imaging tech. This means they can give patients the best care possible. It’s all about finding and treating cancer better.
FAQ
What is the most accurate scan for detecting breast cancer?
Breast MRI is the most accurate for finding breast cancer, thanks to its high sensitivity. It works best in dense breast tissue, outperforming mammography and ultrasound.
How does breast MRI compare to mammography in terms of accuracy?
Breast MRI finds more breast cancers than mammography, but it can also find more false positives. This is more common in women with dense breasts.
What are the benefits of using multiparametric MRI in cancer detection?
Multiparametric MRI gives detailed info on tumor characteristics. This boosts cancer detection and staging accuracy. It’s key in diagnosing prostate and breast cancers.
How does PET/CT compare to CT alone in cancer staging?
PET/CT combines metabolic info from PET with CT’s anatomical details. This gives a better view of cancer spread than CT alone.
What is the role of contrast-enhanced MRI in liver cancer imaging?
Contrast-enhanced MRI uses liver-specific agents to spot liver lesions better. It’s great for finding and characterizing liver cancer, like hepatocellular carcinoma.
When is biopsy considered the gold standard for cancer diagnosis?
Biopsy is the top choice for cancer diagnosis. It confirms cancer through tissue analysis. It’s vital when imaging results are unclear.
How does low-dose CT screening benefit lung cancer detection?
Low-dose CT scans use less radiation than standard CTs. This makes them safer for lung cancer screening in high-risk groups.
What are the advantages of using ultrasound in cancer detection?
Ultrasound is non-invasive and doesn’t use radiation. It’s good for checking thyroid and breast cancers and guiding biopsies.
How does PSMA-PET improve prostate cancer diagnosis?
PSMA-PET is very good at finding prostate cancer, even when it’s not detectable by other means. It helps in accurate staging and treatment planning.
What is the difference between screening and diagnostic imaging?
Screening imaging looks for cancer in people without symptoms. Diagnostic imaging checks symptoms or findings from screening to confirm or rule out cancer.
What are the challenges associated with breast MRI specificity?
Breast MRI might find more false positives, leading to extra biopsies and worry. Improving its specificity while keeping high sensitivity is a big challenge.
How does functional imaging differ from anatomical imaging?
Functional imaging, like PET, shows tissue metabolic activity. Anatomical imaging, such as CT and MRI, looks at structural details. Both are essential for a full cancer assessment.
What is the role of hybrid imaging in cancer diagnosis?
Hybrid imaging, like PET/CT and PET/MRI, combines different imaging strengths. This boosts diagnostic accuracy and gives a deeper look into cancer extent and biology.
Reference
- Schoub, P. K. (2018). Understanding indications and defining guidelines for breast MRI. SA Journal of Radiology.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6837823/



































