Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 700,000 Americans live with a brain tumor. Knowing the chances of recovery is key for patients and their families brain tumor recovery chances.
The survival rate for brain tumor patients changes a lot. It depends on the tumor’s type, size, and where it is. It also depends on the patient’s health overall.
It’s important to understand these factors and the prognosis. This helps in making good choices about treatment.
Key Takeaways
- The survival rate for brain tumor patients varies widely.
- Factors such as tumor type, size, and location impact recovery chances.
- Understanding prognosis is key for treatment decisions.
- Patient overall health plays a big role in recovery.
- Recovery chances can be influenced by treatment effectiveness.
Understanding Brain Tumors and Their Impact
A brain tumor is a growth of abnormal cells in the brain. It can greatly affect a person’s health and life quality. This depends on the tumor’s type, size, and where it is located.
What Defines a Brain Tumor
A brain tumor is when cells in the brain grow out of control. These growths can be either benign (non-cancerous) or malignant (cancerous). Benign tumors grow slowly and are less aggressive. On the other hand, malignant tumors grow fast and can spread to other brain areas.
Primary vs. Secondary Brain Tumors
Brain tumors are divided into primary and secondary types. Primary brain tumors start in the brain. Secondary brain tumors come from cancer spreading to the brain from other parts. Knowing the difference is key for the right treatment.
How Brain Tumors Affect Normal Brain Function
Brain tumors can disrupt brain function in many ways. Symptoms include headaches, seizures, and problems with thinking. They can also change a person’s personality or behavior.
The impact on brain function can be big. It can make it hard for people to do everyday things and stay independent.
Types of Brain Tumors and Their General Prognosis
It’s important to know about the different brain tumors to understand treatment and prognosis. Brain tumors vary in type and behavior, affecting patient outcomes.
Benign Brain Tumors
Benign brain tumors are not cancerous and usually have a better outlook. They grow slowly and don’t spread to other brain areas. Meningioma is a common benign tumor, often cured by surgery. Many patients fully recover after surgery.
- Meningiomas are often benign and can be treated with surgery.
- Other benign tumors include acoustic neuromas and pituitary adenomas.
Malignant Brain Tumors
Malignant brain tumors are cancerous and aggressive. They need intense treatments like surgery, radiation, and chemotherapy. Glioblastoma is the most aggressive malignant tumor, with a poor glioblastoma prognosis. Researchers are working on new treatments like targeted therapies and immunotherapy.
“The management of glioblastoma remains a significant challenge due to its aggressive nature and the limited efficacy of current treatments.”
Common Brain Tumor Types and Their Typical Outcomes
Each brain tumor type has its own prognosis based on its characteristics and treatment response. Low-grade gliomas grow slowly and have a better prognosis than high-grade gliomas. Knowing the tumor type is key to choosing the right treatment and predicting outcomes.
| Tumor Type | Typical Outcome |
| Meningioma | Generally favorable with high survival rates |
| Glioblastoma | Poor prognosis with limited survival |
| Low-Grade Glioma | Variable, but generally better than high-grade gliomas |
The prognosis for brain tumor patients depends on several factors. These include the tumor type, location, and the patient’s health. Advances in medical technology and treatments are improving outcomes for many.
Brain Tumor Grading System and What It Means for Recovery
Knowing about the brain tumor grading system is key for understanding a patient’s chances of recovery. This system helps pathologists classify tumors based on their look and behavior under a microscope.
The World Health Organization (WHO) grading system is widely used for brain tumors. It sorts tumors into four grades, from Grade I (least aggressive) to Grade IV (most aggressive). These grades are based on how the cells look, how fast the tumor grows, and if it can spread.
Grade I and II Tumors (Low-Grade)
Grade I and II tumors are considered low-grade. They grow slowly and are less aggressive. People with these tumors usually have a better chance of recovery than those with higher-grade tumors.
“The prognosis for patients with low-grade gliomas is generally favorable, with many patients surviving for years after diagnosis with appropriate treatment.” –
A leading neuro-oncologist
| Tumor Grade | Characteristics | Prognosis |
| Grade I | Slow-growing, minimal invasion | Favorable, high survival rate |
| Grade II | Slow-growing, some invasion | Generally favorable, but with a risk of progression |
Grade III Tumors (Anaplastic)
Grade III tumors, also known as anaplastic tumors, are more aggressive and malignant. They grow faster and can spread to surrounding brain tissue, making treatment harder.
Treatment for Grade III tumors often involves a combination of surgery, radiation therapy, and chemotherapy. Even with aggressive treatment, the outlook for Grade III tumors is less favorable than for low-grade tumors.
Grade IV Tumors (Glioblastoma)
Grade IV tumors, known as glioblastomas, are the most aggressive and malignant type. They grow quickly and have a high chance of coming back. Glioblastoma is one of the toughest brain cancers to treat.
The outlook for glioblastoma patients is poor, even with new treatments. Research is ongoing to improve treatment outcomes for this aggressive tumor type.
Understanding the brain tumor grading system is vital for patients and their families. It helps them understand the severity of their condition and the possible outcomes of different treatments.
Key Factors That Influence Brain Tumor Recovery Chances
Recovering from a brain tumor depends on several key factors. These include how easy it is to reach the tumor and genetic markers. Knowing these factors helps both patients and doctors make better treatment choices.
Tumor Location and Accessibility
The place of a brain tumor in the brain matters a lot. Tumors in easier-to-reach spots can often be treated with surgery. This can lead to better treatment outcomes and improved quality of life for patients. But, tumors in hard-to-get spots can be tougher to remove, which can affect recovery.
Critical locations that can affect tumor accessibility include:
- Eloquent areas of the brain controlling critical functions like speech and motor skills
- Deep-seated tumors within vital brain structures
- Tumors closely associated with major blood vessels or cranial nerves
Patient Age and Overall Health
A patient’s age and health are big factors in recovery from a brain tumor. Younger people with fewer health problems usually have a better chance of getting better. Older people or those with serious health issues might face more hurdles.
Key health factors influencing recovery include:
- Presence of other serious medical conditions
- Physical fitness and functional status
- Cognitive and neurological baseline
Genetic and Molecular Markers
The genetic makeup of a brain tumor is very important. It helps doctors understand how the tumor will behave and how it will react to treatment. Some genetic markers can mean a tumor is more likely to be treatable.
Important genetic markers include:
- IDH1 and IDH2 mutations in gliomas
- MGMT promoter methylation status
- 1p/19q codeletion in oligodendrogliomas
Timing of Diagnosis and Treatment
When a brain tumor is found and treated early can make a big difference. Early action can stop the tumor from growing and reduce risks. This can lead to better outcomes.
Factors influencing timely diagnosis and treatment include:
- Promptness of medical evaluation upon symptom onset
- Efficiency of diagnostic workup
- Coordination of care among healthcare providers
Brain Tumor Recovery Chances by Specific Tumor Types
The type of brain tumor a patient has greatly affects their recovery chances. Different tumors grow at different rates and respond differently to treatment. This impacts how well a patient can recover.
Meningioma Survival Rates and Recovery Outlook
Meningiomas are usually benign tumors that grow slowly. They come from the meninges, which protect the brain and spinal cord. Most meningiomas are not aggressive and have a good outlook.
Low-Grade Glioma Recovery Prospects
Low-grade gliomas are slower-growing and have a better outlook than high-grade gliomas. They are classified as Grade I or II. The 5-year survival rate can be from 60% to over 90%, depending on several factors.
Treatment for low-grade gliomas usually includes surgery, radiation, and sometimes chemotherapy.
Glioblastoma Prognosis and Survival Statistics
Glioblastoma is the most aggressive brain tumor, classified as Grade IV. It has a poor prognosis, with a median survival time of about 15 months after diagnosis. Despite aggressive treatment, the 5-year survival rate is less than 10%.
Treatment for glioblastoma often involves surgery, radiation, and chemotherapy.
Other Common Brain Tumor Types
Other brain tumors include acoustic neuromas, pituitary adenomas, and medulloblastomas. Each has its own prognosis and treatment options. Acoustic neuromas are benign and have a high success rate for surgery.
Pituitary adenomas are tumors of the pituitary gland and are often treated with surgery or medication. Medulloblastomas are malignant tumors that mainly affect children. They require a combination of surgery, radiation, and chemotherapy.
| Tumor Type | 5-Year Survival Rate | Typical Treatment |
| Meningioma | 85-90% | Surgery |
| Low-Grade Glioma | 60-90% | Surgery, Radiation, Chemotherapy |
| Glioblastoma | <10% | Surgery, Radiation, Chemotherapy |
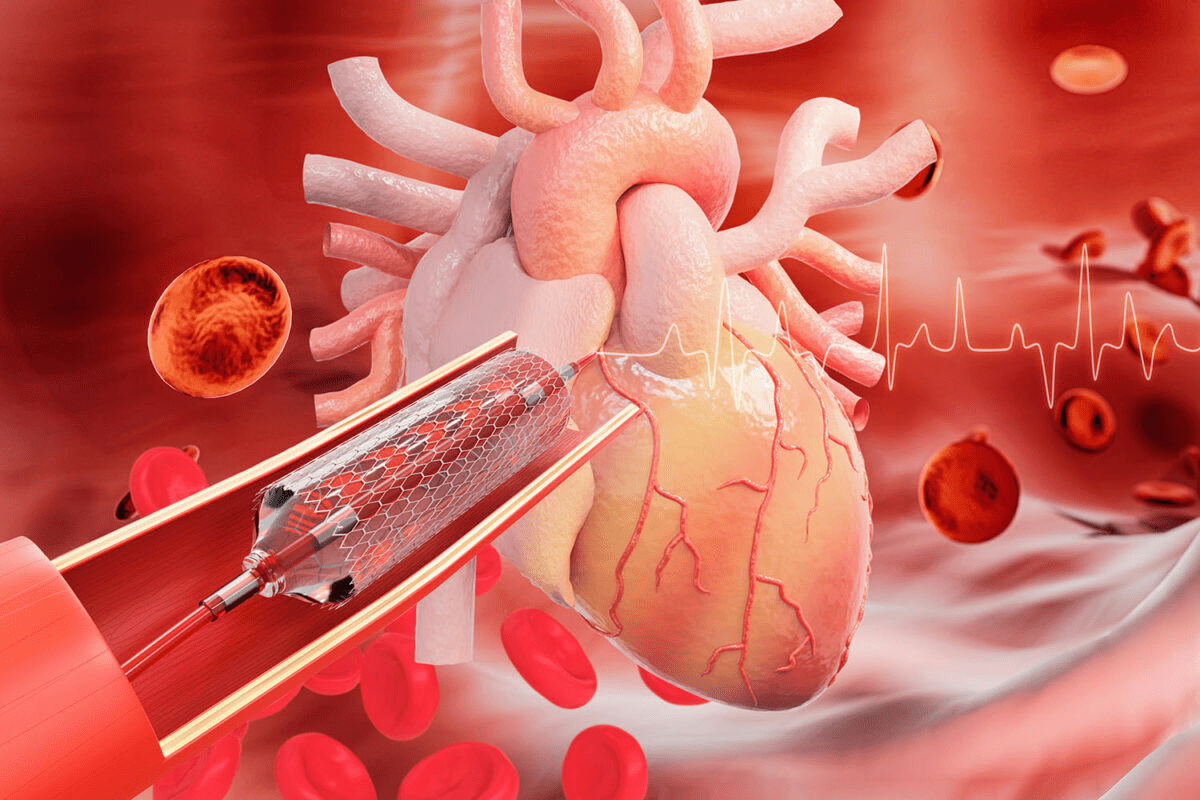
Surgical Treatment Success Rates and Recovery Outcomes
Brain tumor surgery has made big strides, leading to better success rates and recovery for patients. New surgical methods, imaging, and care after surgery have all helped improve outcomes.
Complete vs. Partial Resection Outcomes
The success of surgery depends a lot on how much of the tumor is removed. Complete resection means removing the whole tumor. This is linked to better chances of survival and quality of life compared to partial resection, where only part of the tumor is taken out.
Research shows that complete resection leads to fewer tumor comebacks and better life quality. But, it’s not always possible due to the tumor’s size, location, and how close it is to important brain areas.
Minimally Invasive Surgical Approaches
Minimally invasive surgery is becoming more common for brain tumors. It aims to cut down on recovery time and damage to tissues. Techniques like endoscopic surgery and stereotactic surgery use advanced imaging to precisely remove tumors.
These methods offer smaller cuts, less blood loss, and shorter hospital stays. But, they work best for certain types of tumors and patients’ health.
Post-Surgical Recovery Timeline
Recovery time after brain tumor surgery varies. It depends on the surgery’s extent, tumor location, and the patient’s health. Patients usually spend a few days to a week in the hospital to start recovering.
Rehabilitation after surgery is key to getting back to normal. It focuses on regaining brain function, managing symptoms, and improving life quality. A team of doctors, including neurosurgeons and rehabilitation experts, helps patients through this journey.
Radiation Therapy Effectiveness for Different Brain Tumors
Radiation therapy is key in treating brain tumors. It works best for different types of tumors.
Conventional Radiation Therapy Outcomes
Conventional radiation therapy is common for brain tumors. It uses beams from outside the body to hit the tumor. The success depends on the tumor type and how advanced it is.
This treatment can help patients live longer and shrink tumors. But, results vary based on the tumor and the patient’s health.
Stereotactic Radiosurgery Success Rates
Stereotactic radiosurgery (SRS) is very precise. It gives a high dose of radiation to a small area. It’s great for small to medium-sized tumors.
SRS works well for controlling tumors, like meningiomas and acoustic neuromas. It’s precise, which means less damage to the brain.
Proton Therapy and Other Advanced Radiation Approaches
Proton therapy uses protons to kill cancer cells. It’s good for tumors near important brain areas.
| Therapy Type | Tumor Types Treated | Advantages |
| Conventional Radiation Therapy | Various brain tumors | Wide availability, effective for large tumors |
| Stereotactic Radiosurgery | Small to medium-sized tumors | High precision, minimal damage to surrounding tissue |
| Proton Therapy | Tumors near critical structures | Reduced risk to surrounding brain tissue |
Chemotherapy Response Rates in Brain Tumor Treatment
Chemotherapy plays a key role in treating brain tumors. It involves different treatments and drugs to fight these cancers. The success of chemotherapy depends on the type of tumor, its grade, and the patient’s health.
Standard Chemotherapy Protocols and Their Effectiveness
Standard treatments for brain tumors include a mix of drugs given orally or through an IV. The success of these treatments depends on the tumor’s genetics and how it reacts to the drugs. Chemotherapy is often used with surgery and radiation to treat aggressive tumors.
Temozolomide, a common chemotherapy drug, works well on some brain tumors like glioblastoma. It’s good because it can get into the brain easily.
Temozolomide and Other Common Agents
Temozolomide is a key part of treating glioblastoma and some other aggressive brain tumors. Other drugs might be used based on the tumor and the patient’s health. Doctors choose the right drugs based on guidelines and the patient’s needs.
- Temozolomide is taken by mouth and can get into the brain well.
- Drugs like carmustine and lomustine are used in some cases.
Chemotherapy Side Effects and Management
Chemotherapy for brain tumors can cause side effects, from mild to severe. Common issues include nausea, tiredness, hair loss, and a higher risk of infections. It’s important to manage these side effects to keep the patient’s quality of life good.
Supportive care, like anti-nausea meds and nutrition, can help lessen side effects. Patients should also eat well and tell their doctor about any side effects right away.
Emerging Treatments and Their Impact on Recovery Chances
The field of brain tumor treatment is changing fast. New therapies are coming along. These new treatments could help patients recover better.
Targeted Therapies and Precision Medicine
Targeted therapies are a big step forward in treating brain tumors. They focus on the tumor’s specific traits. This helps avoid harming healthy tissue. Precision medicine is key here, making treatments fit each patient’s tumor.
- Identifying specific genetic mutations within the tumor.
- Developing drugs that target these mutations.
- Monitoring the response to treatment and adjusting as necessary.
Immunotherapy Approaches
Immunotherapy is another exciting area. It uses the body’s immune system to fight tumors. This includes methods like checkpoint inhibitors and CAR-T cell therapy.
Checkpoint inhibitors help the immune system attack cancer cells better. CAR-T cell therapy changes T cells to fight tumor cells.
Clinical Trials and Experimental Treatments
Clinical trials are vital for new treatments. They test the safety and how well these treatments work. Patients in trials get new treatments and help science move forward.
- Phase I trials focus on safety and dosage.
- Phase II trials assess efficacy and side effects.
- Phase III trials compare the new treatment to existing standards.
As research keeps improving, hope for brain tumor patients grows. New treatments offer better chances for recovery and a better life.
Brain Tumor Remission: What It Means and How Common It Is
Brain tumor remission means the tumor’s growth stops or gets much smaller. It’s a big win in treatment, giving patients a better life and maybe more time.
Defining Remission in Brain Tumors
Remission in brain tumors means the tumor is barely there or gone. It’s key to know the difference between complete remission and partial remission. Complete remission means the tumor is gone. Partial remission means it’s much smaller.
Partial vs. Complete Remission Statistics
Remission rates vary by tumor type and grade. For example, low-grade gliomas have better chances of complete remission than glioblastomas. Studies show patients in complete remission live longer than those who aren’t.
- Low-grade glioma patients: 70-80% partial or complete remission rate
- Glioblastoma patients: 20-30% partial remission rate, with complete remission being rare
- Meningioma patients: 80-90% surgical cure rate, often resulting in complete remission
Factors That Improve Remission Chances
Several things can help brain tumor patients get remission. Early diagnosis, the tumor’s location, and the patient’s health are important. So is the treatment plan. New surgery, radiation, and chemotherapy methods help too.
Key factors influencing remission chances:
- Tumor type and grade
- Patient’s age and overall health
- Effectiveness of the treatment plan
- Early diagnosis and intervention
In conclusion, brain tumor remission is a hopeful concept. Knowing what affects remission and the stats for different tumors helps patients and families. It makes the treatment journey clearer.
Recurrence Risk: Understanding the Chances of Tumor Return
Knowing the risk of recurrence is key for those with brain tumors. Recurrence means the tumor comes back after treatment. This can happen even if the first treatment seemed to work well.
Recurrence Rates by Tumor Type
The chance of recurrence changes a lot based on the tumor type. For example, meningiomas, which are usually not cancerous, have a lower chance of coming back. On the other hand, glioblastomas, which are cancerous and aggressive, have a higher chance of coming back.
- Meningiomas: Usually have a low chance of coming back, mostly if they are completely removed.
- Glioblastomas: Have a higher chance of coming back, often needing more treatments.
- Low-grade gliomas: May have a moderate chance of coming back, with some types more likely than others.
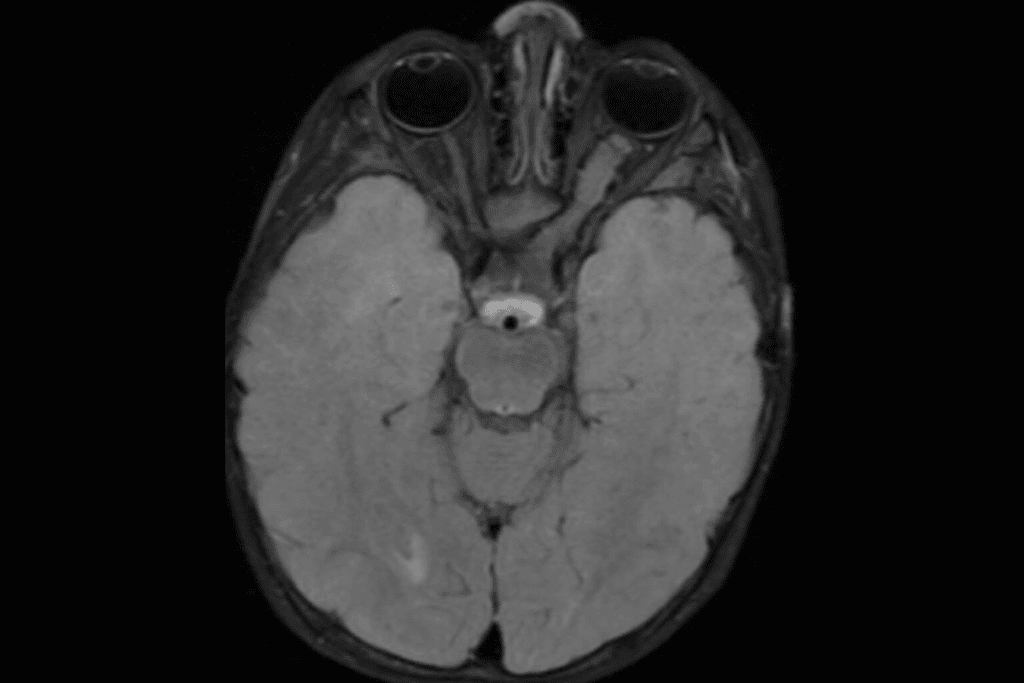
Monitoring and Early Detection of Recurrence
Regular checks are key for catching recurrence early. This usually includes imaging like MRI or CT scans and doctor visits.
Early detection is very important. It can greatly improve how well a tumor can be managed and treated when it comes back.
Treatment Options for Recurrent Tumors
Treatment for tumors that come back depends on many things. These include what treatments were used first, where and how big the tumor is, and the patient’s health.
| Treatment Option | Description |
| Surgery | Having surgery again might be an option for tumors that can be safely removed. |
| Radiation Therapy | More radiation might be used, if the tumor is in a spot that wasn’t hit before. |
| Chemotherapy | There are different chemotherapy plans, based on the tumor type and past treatments. |
Knowing about recurrence risk and treatment choices helps patients and their families make better decisions about care.
Long-Term Survival Statistics and Quality of Life
Patients with brain tumors worry about survival and quality of life. Many factors affect these outcomes. Thanks to medical progress, more patients are living longer and better.
5-Year and 10-Year Survival Rates
Survival rates for brain tumor patients depend on the tumor type, grade, and location. They also depend on the patient’s health. 5-year and 10-year survival rates are key metrics for long-term survival.
- For some tumors, like meningiomas, the 5-year survival rate is high, often over 90%.
- But, aggressive tumors like glioblastoma have much lower 5-year survival rates, usually under 10%.
- Thanks to new treatments, 10-year survival rates for some tumors have improved, though they’re low for very aggressive ones.
Quality of Life After Brain Tumor Treatment
Quality of life after treatment is very important. It’s not just about living longer but also about living well. Several factors affect quality of life, including:
- Neurological Function: How well the brain works after treatment greatly affects quality of life.
- Cognitive Outcomes: How well the brain thinks and remembers is key to doing everyday things.
- Emotional and Psychological Support: Getting help from therapists and support groups can really improve life after treatment.
Neurological Function and Cognitive Outcomes
The effects of brain tumor treatment on the brain can vary a lot. Some people face big challenges, while others have few problems.
| Factor | Influence on Quality of Life |
| Neurological Function | Directly affects physical capabilities and independence. |
| Cognitive Outcomes | Impacts ability to work, engage in social activities, and perform daily tasks. |
Knowing about these factors can help patients and their families make better choices about care.
Neurorehabilitation and Functional Recovery After Treatment
Recovering from brain tumor treatment is not just about medical care. It also includes neurorehabilitation. This process helps patients regain their abilities, manage symptoms, and improve their life quality.
Physical Rehabilitation Approaches
Physical rehabilitation is key in neurorehabilitation. It focuses on getting patients back to their physical strength, mobility, and coordination. Physical therapists create exercise plans that meet each patient’s needs, like walking, balance, or fine motor skills.
Rehabilitation may also use assistive devices and technologies. For example, canes, walkers, or wheelchairs can help with mobility. Some patients learn to use prosthetic limbs or orthotics.
Cognitive Rehabilitation Strategies
Cognitive rehabilitation is vital for those recovering from brain tumors or their treatment. It aims to improve memory, attention, language, and executive functions. Programs are customized to address each patient’s cognitive challenges.
These programs mix cognitive training, compensatory strategies, and assistive technology. Patients might use calendars or reminders on phones for memory help. They also learn new ways to organize information.
Emotional and Psychological Support
Emotional and psychological support is essential in neurorehabilitation. Patients often face emotional challenges during recovery. Support helps them manage anxiety, depression, and other feelings, promoting well-being.
Support groups, online or in-person, offer a sense of community. They allow patients to share and learn from others. Individual counseling or therapy provides personalized support, helping patients cope with their emotional needs.
Conclusion: Navigating Brain Tumor Recovery with Realistic Expectations
Knowing about brain tumor recovery chances is key for patients and their families. The path to getting better is complex. It depends on the tumor type, grade, where it is, and the treatments available. Understanding these helps people better handle their diagnosis and treatment plan.
Good follow-up care is essential to track recovery and catch any signs of the tumor coming back. Regular visits and tests help doctors change treatment plans if needed. This can lead to better treatment outcomes and improved quality of life for patients.
Every person’s recovery from a brain tumor is different. But, knowing about new treatments and rehab methods can really help. By keeping expectations realistic and staying active, patients can make their recovery better.
FAQ
What are the chances of recovering from a brain tumor?
Recovery chances from a brain tumor depend on several factors. These include the tumor’s type and grade, its location, and the patient’s health. Generally, benign tumors have a better chance of recovery than malignant ones.
How does the brain tumor grading system affect recovery chances?
The brain tumor grading system is key in determining recovery chances. Higher-grade tumors are more aggressive and have a poorer prognosis. Lower-grade tumors are less aggressive and have a better outlook.
What is the survival rate for meningioma patients?
Meningioma patients usually have a high survival rate. Most meningiomas are benign, which means they have a good prognosis. The 5-year survival rate for benign meningioma is around 90-100%.
How effective is surgical treatment for brain tumors?
Surgical treatment can be very effective for brain tumors, depending on the situation. The success rate depends on the tumor type, location, and the patient’s health.
What are the benefits of radiation therapy for brain tumors?
Radiation therapy can be effective for brain tumors, even if surgery is not possible. It helps control tumor growth and can improve survival rates.
How does chemotherapy work for brain tumor treatment?
Chemotherapy uses medications to kill cancer cells. It can be used alone or with other treatments like surgery and radiation therapy for brain tumors.
What are the emerging treatments for brain tumors?
New treatments for brain tumors include targeted therapies and immunotherapy. These aim to improve treatment outcomes and reduce side effects.
What is the risk of recurrence for brain tumors?
The risk of recurrence for brain tumors varies. Higher-grade tumors have a higher risk, while lower-grade tumors have a lower risk.
How does neurorehabilitation help after brain tumor treatment?
Neurorehabilitation is vital after brain tumor treatment. It helps patients regain physical, cognitive, and emotional function. This improves their quality of life.
What are the long-term survival statistics for brain tumor patients?
Long-term survival for brain tumor patients depends on the tumor type and grade. Patients with benign tumors generally have a better long-term survival rate than those with malignant tumors.
How do genetic markers impact brain tumor recovery chances?
Genetic markers can significantly affect brain tumor recovery chances. Certain genetic mutations can influence treatment outcomes and prognosis.
What is the role of follow-up care in brain tumor recovery?
Follow-up care is critical in brain tumor recovery. It allows healthcare providers to monitor for recurrence and manage long-term treatment side effects.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37119627/