Last Updated on December 1, 2025 by Bilal Hasdemir
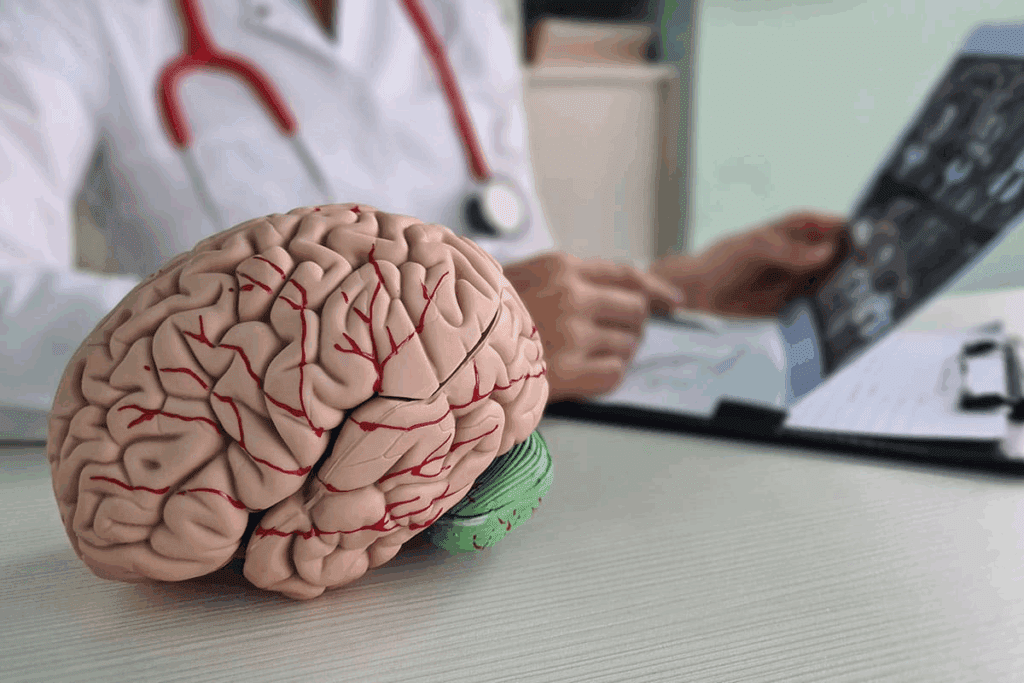
Getting a brain tumor diagnosis is very tough. Understanding the end-of-life timeline is essential for both patients and their families.
A brain tumor diagnosis hits not just the patient but also their loved ones hard. It’s vital to understand how the disease progresses.
The end-of-life timeline changes a lot from person to person. It depends on the tumor type, stage, and treatment choices.
What is the brain tumor end of life timeline? This guide explains the devastating final stages.
Key Takeaways
- Knowing the end-of-life timeline helps patients and families get ready for what’s ahead.
- The growth of a brain tumor impacts not just the patient but also their family.
- The end-of-life timeline varies a lot among people.
- Things like tumor type, stage, and treatment options affect the end-of-life timeline.
- Understanding how the disease moves is key for making smart choices.
Understanding Brain Tumor End of Life Progression
Brain tumor end-of-life progression varies a lot. It depends on the tumor type and the person’s health. The type of tumor and how aggressive it is also play a big role.
Types of Brain Tumors and Their Terminal Trajectories
Each brain tumor type has its own timeline for the end of life. For example, glioblastoma is very aggressive. It usually has a shorter timeline than other types of tumors.
“The prognosis for glioblastoma patients remains poor, with a median survival of approximately 15 months after diagnosis,” a study on glioblastoma treatment outcomes found.
Factors Affecting End-of-Life Timeline
Several things can affect how long a brain tumor patient has left. These include:
- Tumor type and grade: Higher-grade tumors grow faster.
- Patient’s age and overall health: Older patients or those with health issues may have less time left.
- Treatment response: How well treatments like surgery and chemotherapy work can change the disease’s progress.
Knowing these factors helps in giving the right care and support at the end of life.
Early Signs of Entering the Terminal Phase
It’s important to spot early signs of the terminal phase for brain tumor patients and their caregivers. Knowing these signs helps manage symptoms better and prepare for end-of-life care.
Physical Symptoms Indicating Disease Progression
As brain tumor patients reach the terminal phase, physical symptoms get worse. These include:
- Increased fatigue and weakness
- Significant weight loss
- Changes in sleep patterns
- Seizures, which can become more frequent and severe
Managing these symptoms is key to keeping the patient comfortable. For example, seizures can be tough and might need changes in anti-seizure medications.
Cognitive and Neurological Changes
Cognitive and neurological changes also show disease progression. Patients might notice:
| Symptom | Description |
| Memory Loss | Difficulty recalling recent events or learning new information |
| Confusion | Disorientation to time, place, or person |
| Personality Changes | Alterations in behavior, mood, or emotional responses |
Such changes can be particularly challenging for both patients and their families. Knowing they’re part of the disease progression helps in coping.
As the disease gets worse, neurological symptoms like weakness, speech issues, and vision problems become more common. A full approach to palliative care is needed to manage these symptoms.
The 6-12 Month Timeline: Initial Terminal Stage
When patients reach the 6-12 month timeline, they enter the initial terminal stage of brain tumors. Palliative care becomes very important during this time. Patients and their families face big challenges as the disease gets worse.
Common Symptoms and Management
As brain tumors grow, patients face many symptoms that affect their life quality. Some common symptoms include:
- Pain: It’s key to manage pain well to keep patients comfortable.
- Fatigue: Finding a balance between rest and activity helps manage fatigue.
- Cognitive changes: Helping patients with memory and thinking skills is very important.
- Seizures: For some, seizures are a worry; managing them is essential.
Managing symptoms at this stage needs a team effort. This includes medicines, physical therapy, and counseling. The aim is to keep the patient’s life as good as possible.
| Symptom | Management Strategies |
| Pain | Medication, pain management clinics |
| Fatigue | Rest, physical therapy, activity planning |
| Cognitive changes | Cognitive rehabilitation, memory aids |
| Seizures | Anticonvulsant medication, seizure monitoring |
Treatment Decisions at This Stage
Decisions about treatment during the 6-12 month timeline are very important. They often involve weighing the benefits and drawbacks of treatment. Patients and their families need to think about:
- Palliative care: Focusing on easing symptoms and improving life quality.
- Life-sustaining treatments: Deciding whether to keep or stop treatments that keep patients alive.
- Hospice care: Thinking about hospice for full end-of-life care.
These decisions need careful thought and support from healthcare teams. It’s vital to make choices that match the patient’s values and goals.
The 3-6 Month Timeline: Disease Acceleration
As brain tumors grow, patients face a critical 3-6 month period. Symptoms worsen, and care needs change a lot. The focus shifts from trying to cure the disease to comfort care and palliative care. These aim to enhance the patient’s quality of life.
Increasing Symptom Burden
In this 3-6 month span, symptoms like pain, nausea, and weakness grow. These are due to tumor progression. It’s key to manage these symptoms well to keep the patient comfortable and improve their life quality.
Managing symptoms is done through palliative care. This includes adjusting medications, physical therapy, and other support. It’s important for healthcare teams to work with patients and their families. They need to create care plans that meet these changing needs.
Transitioning Care Approaches
As the disease gets worse, changing care approaches is vital. This might mean moving from aggressive treatments to more supportive care. Comfort care, like pain management and emotional support, is very important in this phase.
Healthcare providers should talk openly with patients and their families. They should discuss the disease’s outlook, treatment choices, and the need for advance care planning. This includes thinking about hospice care when it’s right. This ensures patients get the right support during this key time.
By adjusting care to meet the patient’s changing needs, healthcare teams can help keep dignity and quality of life. Even as the disease advances.
The Final 1-3 Months: Advanced Terminal Stage
When a brain tumor reaches its final stage, patients see a big drop in their abilities. This stage is marked by a quick worsening of the patient’s health. It’s key for families and caregivers to get ready for what’s coming.
Significant Functional Decline
In the last 1-3 months, patients with advanced brain tumors show many signs of decline. These include:
- Increased fatigue and weakness
- Difficulty with mobility and balance
- Loss of appetite and weight loss
- Cognitive changes, such as confusion and disorientation
Table: Common Symptoms and Their Management
| Symptom | Management Approach |
| Fatigue | Conserve energy, rest as needed |
| Difficulty with Mobility | Use assistive devices, physical therapy |
| Loss of Appetite | Small, frequent meals, nutritional supplements |
Preparing for End-of-Life Care
It’s vital to prepare for end-of-life care at this time. This means making choices about the patient’s care, like considering hospice. Hospice care aims to make the patient’s life as comfortable as possible.
Families should talk to healthcare providers about:
- Pain management strategies
- Symptom control measures
- Emotional and psychological support
- Advance directives and DNR orders
By knowing what to expect and how to support their loved ones, families can offer meaningful care in the final stages of a brain tumor.
The Last Weeks of Life with a Brain Tumor
Knowing the signs of the end for brain tumor patients is key. It helps in giving the right care and support in their final days. As the disease gets worse, patients face many physical and brain changes. These can be hard for them and their families.
Physical Changes and Symptoms
In the last weeks, brain tumor patients often get much weaker. They might feel very tired and have trouble doing things. Some may even need help with basic tasks or stay in bed.
It’s important to manage symptoms like pain, nausea, and trouble breathing. This helps keep the patient comfortable. Healthcare teams might change medicines to help with these symptoms.
Neurological Changes and Awareness
Brain tumor patients also see changes in their brain. These can include seizures, confusion, and altered levels of consciousness. Seizures are serious and need quick medical help. Doctors might adjust medicines to stop seizures.
As the brain weakens, patients might not be as aware or responsive. They could be clear for a bit or not respond at all. It’s important to support them and their families during these times.
Families need to know these changes are part of the disease’s progress. Healthcare teams can help manage these changes. They also offer support to both the patient and their loved ones.
The Final Days: What to Expect
When a brain tumor patient is nearing the end, it’s important to know what to expect. Recognizing end-of-life symptoms and using comfort measures are key. This helps families support their loved ones and make informed choices.
Common End-of-Life Symptoms
In the final days, patients may show signs like increased sleepiness, trouble swallowing, and breathing changes. It’s vital to watch these symptoms closely and get advice from healthcare professionals.
Some symptoms include:
- Drowsiness or increased sleep
- Reduced appetite or trouble swallowing
- Changes in breathing, such as Cheyne-Stokes respiration
- Decreased response to words or visual cues
| Symptom | Possible Interventions |
| Drowsiness | Ensure a comfortable environment, adjust pain management as needed |
| Difficulty Swallowing | Modify diet to softer foods, consider hydration support |
| Changes in Breathing | Provide oxygen if prescribed, maintain a calm environment |
Comfort Measures in the Final Hours
In the final days, comfort is key. This means managing pain, keeping the patient hydrated, and ensuring they’re comfortable. Emotional support is also essential for both the patient and their family.
Comfort measures include:
- Administering pain medication as prescribed
- Using gentle positioning to reduce discomfort
- Providing emotional reassurance and support
In conclusion, knowing what to expect in the final days of a brain tumor patient’s life is important. By recognizing symptoms and using comfort measures, caregivers can support their loved ones in a peaceful passing.
Brain Tumor End of Life: Special Considerations
The final stages of a brain tumor bring unique challenges. Managing seizures and steroid use complications are key. Healthcare providers must focus on comfort and symptom management as patients near the end.
Seizure Management in Terminal Stages
Seizures are common in brain tumor patients. Managing them is vital as the disease advances. “
To manage seizures, a mix of antiepileptic drugs (AEDs) and supportive measures is used. Adjusting AEDs as the patient’s condition changes is important. This requires close monitoring and teamwork with a neurologist.
Steroid Use and Complications
Steroids are used to reduce tumor swelling and ease symptoms like headache and confusion. But long-term use can cause muscle weakness, osteoporosis, and increase infection risk.
Important considerations in steroid use include:
- Monitoring for signs of steroid-induced myopathy
- Implementing measures to prevent osteoporosis
- Vigilance for infections and prompt treatment when necessary
As patients near the end of life, the focus shifts to comfort and quality of life. Steroid use should be tailored to meet these goals. Dosage should be adjusted based on symptoms and overall condition.
Palliative Care Approaches for Terminal Brain Tumors
Palliative care helps patients with terminal brain tumors feel better. It focuses on making their life as good as possible.
Palliative care is a full approach for patients with terminal brain tumors. It covers physical, emotional, social, and spiritual needs.
Pain Management Strategies
Managing pain is key in palliative care for terminal brain tumor patients. It uses many methods. This includes medicines and non-medical ways like relaxation and therapy.
| Pain Management Method | Description | Benefits |
| Pharmacological Interventions | Use of medications like opioids and adjuvant analgesics | Effective pain relief, improved quality of life |
| Non-Pharmacological Methods | Techniques such as relaxation, cognitive-behavioral therapy | Reduced pain perception, enhanced patient coping |
Managing Neurological Symptoms
Managing neurological symptoms is vital in palliative care for terminal brain tumor patients. Symptoms like seizures and weakness can really affect a patient’s life.
Managing these symptoms might include medicines for seizures and swelling. Other treatments aim to ease specific symptoms.
With a full palliative care approach, healthcare can greatly improve life for patients with terminal brain tumors.
Hospice Care for Brain Tumor Patients
When brain tumor patients near the end of life, hospice care becomes a key support. It offers end-of-life care that meets physical, emotional, and spiritual needs. This care is for those with terminal illnesses.
Hospice teams include doctors, nurses, social workers, chaplains, and volunteers. They work together to manage pain and symptoms. They also offer emotional support and spiritual care that fits the patient’s needs.
When to Consider Hospice
Choosing when to start hospice care can be tough. It’s usually when treatments no longer work, and life expectancy is six months or less. For brain tumor patients, this often happens when the disease has grown a lot, and the focus is on quality of life.
Signs it might be time for hospice include:
- More or worse symptoms like seizures, headaches, or memory loss
- Significant weight loss or health decline
- Harder to do daily tasks
- Frequent hospital stays or ER visits
What Hospice Provides for Brain Tumor Patients
Hospice care offers many services for brain tumor patients and their families. These include:
- Pain and Symptom Management: Managing pain, seizures, and other symptoms to keep the patient comfortable.
- Emotional and Spiritual Support: Counseling and support for patients and families to deal with the emotional and spiritual challenges of terminal illness.
- Assistance with Daily Activities: Help with bathing, dressing, eating, and other daily tasks.
- Respite Care: Temporary relief for caregivers, so they can rest and recharge.
- Bereavement Support: Support for families before and after the loss of their loved one.
Hospice care helps brain tumor patients live their final days with dignity and comfort. They are surrounded by their loved ones.
Supporting Family Members Through the End-of-Life Journey
Caring for a loved one with a terminal brain tumor is tough on family members. As the disease gets worse, they often take on caregiving duties. They face tough medical choices and emotional hurdles.
Emotional and Psychological Support
Family members need emotional and psychological help during this hard time. Counseling services offer a safe place to talk about feelings. Support groups, online or in-person, connect them with others facing similar issues.
- Encourage open communication about feelings and fears.
- Provide resources for counseling and support groups.
- Emphasize the importance of self-care for caregivers.
Self-care is key for family members to stay well. Simple things like walking, reading, or hobbies can help reduce stress.
Practical Caregiving Guidance
Family members need practical guidance to care for their loved ones well. This includes knowing the patient’s needs, managing symptoms, and handling medical visits.
- Understand the patient’s medication regimen and possible side effects.
- Learn to manage symptoms like pain, nausea, and tiredness.
- Keep track of medical appointments and talk to healthcare providers.
By giving emotional and practical support, family members can help their loved ones through the end-of-life journey. Hospice care can also provide extra help and advice during this time.
Making Critical Decisions: Medical Interventions and DNR Orders
Understanding end-of-life care for brain tumor patients is key. It involves advance directives and making tough medical choices. As the disease gets worse, patients and families face hard decisions that affect their quality of life.
Navigating End-of-Life Medical Decisions
Deciding on end-of-life care for brain tumor patients is a tough balance. Decisions on medical interventions must consider the patient’s wishes and how likely they are to get better.
- It’s important to know the patient’s advance directives.
- Talking to healthcare providers about the patient’s future is vital.
- Looking at the good and bad of ongoing medical care is necessary.
Advance Directives and Their Importance
Advance directives are legal documents that state a patient’s medical wishes if they can’t speak for themselves. Having clear advance directives helps families and doctors make decisions.
Important parts of advance directives include:
- A living will, which says what treatments the patient wants or doesn’t want.
- A durable power of attorney for healthcare, which lets someone else make medical choices for the patient.
- Do Not Resuscitate (DNR) orders, which tell doctors not to do CPR if the patient’s heart stops or they stop breathing.
With these documents, patients can make sure their care matches their values, even when they can’t speak for themselves.
Conclusion: Finding Peace in the Brain Tumor End-of-Life Journey
Dealing with a loved one’s end-of-life journey due to a brain tumor is tough. It’s important to focus on peaceful passing. This means giving them the best end-of-life care possible. It should cover their physical, emotional, and mental health.
Family support is key during this time. Family members can offer comfort, help with daily tasks, and make important care decisions. This support is vital for those facing a brain tumor end of life.
Knowing about the disease’s progression and care options helps families support their loved ones better. Services like palliative care and hospice are essential. They help manage symptoms and offer comfort in the final stages.
In the end, peace comes from a mix of medical care, emotional support, and practical advice. By focusing on these, families can make a caring and supportive space for their loved ones.
FAQ
What is the typical end-of-life timeline for a brain tumor patient?
The time left for a brain tumor patient varies a lot. It depends on the tumor type, its stage, and the patient’s health. It can be from a few months to a couple of years after finding out.
How do different types of brain tumors affect the end-of-life timeline?
Different tumors have different effects on life’s end. For example, glioblastoma grows fast and can shorten life. This is unlike slower-growing tumors.
What are the early signs that a brain tumor patient is entering the terminal phase?
Early signs include getting weaker, trouble swallowing, and breathing changes. Also, confusion, disorientation, and less response are signs.
How can symptoms be managed during the 6-12 month timeline after entering the terminal stage?
Managing symptoms in this time involves palliative care. This includes controlling pain, seizures, and other symptoms to improve life quality.
What changes can be expected in the 3-6 month timeline before the end of life?
In this time, symptoms get worse, and physical and neurological decline increases. Care needs to focus on comfort and support.
How should care be adapted for a brain tumor patient in the final 1-3 months of life?
Care should focus on comfort, managing pain, and emotional support. This is for the patient and their family.
What physical and neurological changes occur in the last weeks of life?
Patients get much weaker, less responsive, and breathing changes. These signs show life’s end is near.
How can seizure management be effectively handled at the end of life?
Seizures are managed with anticonvulsants and other methods. This helps prevent or lessen seizures, which are distressing.
What is the role of palliative care in managing terminal brain tumors?
Palliative care is key in managing pain and symptoms. It aims to improve life quality for patients with terminal tumors.
When should hospice care be considered for brain tumor patients?
Hospice care is for when life expectancy is six months or less. It shifts focus to comfort care, not curing.
How can family members be supported through the end-of-life journey?
Family support includes emotional help, caregiving tips, and resources. This helps them cope with caring for a loved one with a terminal brain tumor.
What are the key considerations when making decisions about medical interventions and DNR orders?
Decisions should follow the patient’s wishes, as stated in advance directives. Healthcare providers should be involved to ensure care matches the patient’s preferences.
How can steroid use be managed effectively at the end of life?
Steroid use must be managed to avoid muscle weakness, mood changes, and infection risks. It should help reduce swelling and improve symptoms.
Reference
National Center for Biotechnology Information. Brain Tumor End of Life Timeline Variability. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33034905/