Last Updated on December 3, 2025 by Bilal Hasdemir

Epilepsy affects millions worldwide, and its impact goes beyond the seizures themselves. Sudden Unexpected Death in Epilepsy (SUDEP) is a significant concern. It highlights the need to understand the risks associated with seizure disorders.
People with epilepsy face challenges beyond managing their condition with seizure medications. They also risk status epilepticus, a life-threatening condition that needs immediate medical attention. Status epilepticus is the most awful con of epilepsy. Our guide reveals the critical, devastating dangers of this life-threatening emergency.
Key Takeaways
- Epilepsy poses significant risks beyond seizures.
- SUDEP is a major concern for those with epilepsy.
- Managing epilepsy requires careful consideration of seizure medications.
- Understanding the risks can help in managing the condition effectively.
- Epilepsy management is key to prevent complications like status epilepticus.
Understanding Epilepsy and Its Impact
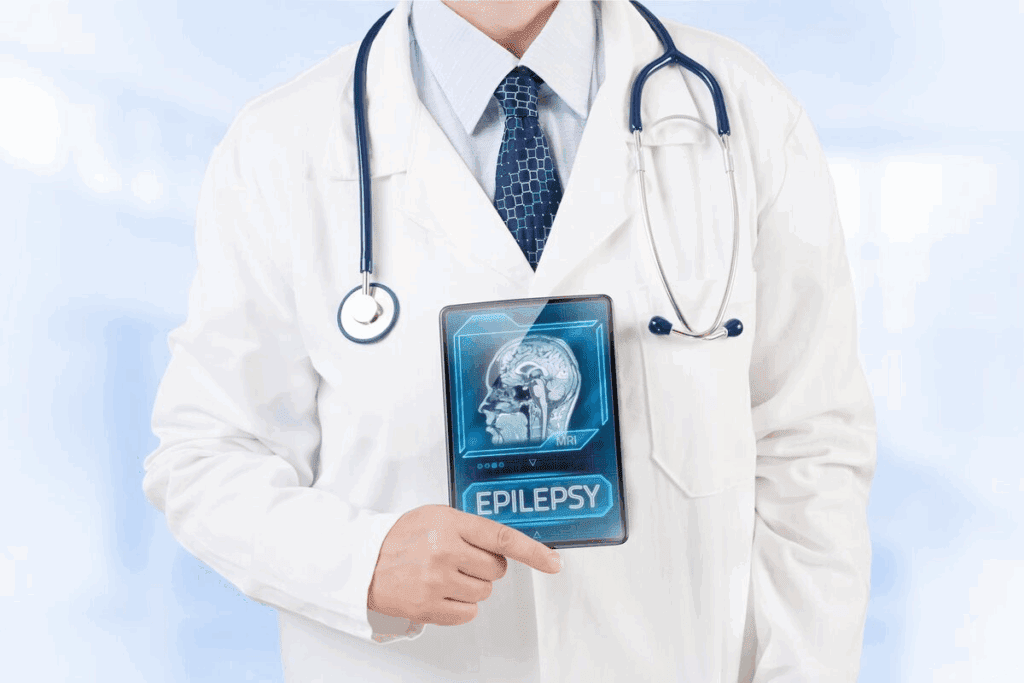
Epilepsy is a complex condition that affects not just the person diagnosed but also their family and community. It’s important to understand its definition, prevalence, and impact on society.
What Defines Epilepsy as a Neurological Disorder
Epilepsy is a neurological disorder that affects the brain’s electrical activity. This leads to recurrent seizures. These seizures can range from mild to severe convulsions.
The disorder is considered chronic, meaning it is a long-term condition. It requires ongoing management.
Prevalence and Statistics in the United States
The prevalence of epilepsy in the United States is a significant public health concern. About 3.4 million people in the U.S. are living with epilepsy. This includes about 470,000 children.
This makes epilepsy a substantial seizure disorder affecting a considerable portion of the population.
The Centers for Disease Control and Prevention (CDC) report that epilepsy affects people of all ages. It is more common among certain demographics. Understanding these statistics is key for healthcare providers, policymakers, and the general public to address the needs of those affected by epilepsy.
Physical Health Challenges of Living with Epilepsy
Epilepsy brings many physical health challenges. These include risks during seizures, recovery after seizures, and other health issues. People with epilepsy face many physical challenges that affect their daily lives and well-being.
Injury Risks During Seizures
One big worry for those with epilepsy is getting hurt during a seizure. Seizure injuries can be anything from small cuts to serious head injuries. This risk is higher for those who have tonic-clonic seizures, which can cause convulsions and loss of control.
To lower these risks, it’s key for people with epilepsy and their caregivers to take steps. This includes padding furniture corners, using safe bedding, and making sure there’s enough space to move without hitting things.
Physical Fatigue and Recovery
Another big challenge is physical fatigue after a seizure. Seizures can be very tiring, leaving the person feeling weak. Recovery from seizures takes time, and rest is very important.
To manage fatigue, it’s important to balance activity and rest. People with epilepsy should not push themselves too hard, and they need to rest well. Getting enough sleep and eating healthy foods also helps the body recover.
Comorbid Health Conditions
Those with epilepsy often face comorbid health conditions, or other health issues. These can include mental health problems like depression and anxiety, as well as other neurological conditions.
Handling these conditions requires a team effort with healthcare providers. It’s important to monitor and treat these conditions while managing epilepsy. By tackling these issues, people can improve their health and make their care easier.
Status Epilepticus: A Life-Threatening Complication
Status epilepticus is a serious medical emergency in epilepsy. It happens when seizures last too long or happen too often. This condition is very dangerous and needs quick medical help.
Definition and Types of Status Epilepticus
Status epilepticus is when a seizure lasts over 30 minutes or when seizures keep happening without a break. There are two main types: convulsive and non-convulsive status epilepticus.
Convulsive status epilepticus has seizures with shaking. Non-convulsive status epilepticus doesn’t have shaking but can also be very harmful. Knowing the type is key for the right treatment.
Emergency Treatment Protocols
First, doctors give benzodiazepines to stop the seizure. If it doesn’t work, they might use phenytoin or valproate.
The treatment plan is to stop the seizure fast. This helps avoid lasting brain damage.
“Prompt treatment of status epilepticus is critical to avoid long-term brain damage.” – Epilepsy Foundation
Long-term Neurological Damage
Not treating status epilepticus quickly can cause lasting brain damage. The long seizure can hurt brain cells. This might lead to problems with thinking and behavior.
| Potential Consequences | Description |
| Neurological Damage | Prolonged seizures can cause injury to neurons, potentially leading to long-term cognitive and behavioral issues. |
| Cognitive Impairment | Individuals may experience difficulties with memory, attention, and processing speed following status epilepticus. |
| Behavioral Changes | Some people may exhibit changes in behavior, including mood swings and irritability. |
Knowing the dangers of status epilepticus shows how urgent medical care is. It’s vital for those with epilepsy to have good management plans.
Medication Burdens and Side Effects
For people with epilepsy, anti-seizure meds are a mixed bag. They help control seizures but can also harm health. Finding the right balance is key.
Common Anti-Seizure Medications
Many meds are used to treat epilepsy. Levetiracetam (Keppra), lamotrigine (Lamictal), and valproate (Depakote) are common ones. Each works differently and is picked based on the type of seizures and the patient’s health.
- Levetiracetam is known for its relatively favorable side effect profile.
- Lamotrigine is often used for its efficacy in a broad range of seizure types.
- Valproate is effective but can have significant side effects, particular in women of childbearing age.
Short-term Side Effects
Short-term side effects include drowsiness, dizziness, and stomach problems. These usually get better as your body gets used to the medication.
| Medication | Common Short-term Side Effects |
| Levetiracetam (Keppra) | Irritability, Fatigue |
| Lamotrigine (Lamictal) | Rash, Dizziness |
| Valproate (Depakote) | Tremors, Weight Gain |
Long-term Health Implications
Long-term use of these meds can affect bone density, brain function, and metabolism. It’s important to monitor and manage these effects.
For example, long-term use of some meds may raise the risk of osteoporosis. Regular bone scans and treatments might be needed.
It’s vital to know the possible downsides of anti-seizure meds for effective epilepsy care. Doctors and patients work together to find the best treatment plan. This plan aims to control seizures while keeping quality of life high.
Cognitive Impairments Associated with Epilepsy
Cognitive challenges often come with epilepsy. They affect memory, how fast we process information, and our ability to make decisions. These issues can make daily tasks harder.
Types of Memory Loss
Memory loss is common in people with epilepsy. It can be short-term memory loss, making it hard to remember recent things or learn new stuff. Others might have long-term memory issues, finding it tough to recall past events or familiar words.
There are many reasons for memory loss in epilepsy. These include the condition itself, how often and what kind of seizures someone has, and the side effects of medicines to control seizures.
Processing Speed and Executive Function
People with epilepsy may also struggle with processing speed and executive function. Processing speed is how fast we can handle and react to information. Executive function includes skills like planning, making decisions, and solving problems.
- Difficulty in quickly processing visual information
- Challenges in making decisions or planning tasks
- Struggling with multitasking or following instructions
Strategies for Cognitive Support
There are ways to help with cognitive issues from epilepsy. These include:
- Cognitive Rehabilitation: Special training programs can improve memory, attention, and decision-making skills.
- Compensatory Strategies: Using tools like calendars, reminders, and notes can help with memory problems.
- Lifestyle Modifications: Regular exercise, a healthy diet, and enough sleep can help keep the brain healthy.
Understanding and addressing cognitive challenges from epilepsy can improve life quality. By using the right support strategies, people can manage their condition better.
Psychological Impact of Seizure Disorders
The psychological impact of epilepsy is a big concern for those with the disorder. It affects their quality of life. Living with epilepsy means managing seizures and dealing with mental health challenges.
Depression and Anxiety
People with epilepsy are more likely to have depression and anxiety than others. Seizures can be unpredictable, causing stress. This stress can lead to these mental health issues.
A study found that depression in people with epilepsy is much higher than in those without. This shows the need for mental health support.
- Depression can show as sadness, loss of interest, and changes in appetite or sleep.
- Anxiety can be seen as too much worry, fear, or avoiding things because of seizures.
Post-Ictal Psychological States
After a seizure, some people feel confused, agitated, or even psychotic. These feelings are usually short-lived but can be hard for both the person and their caregivers.
| Post-Ictal State | Characteristics | Duration |
| Confusion | Disorientation, trouble understanding surroundings | Minutes to hours |
| Agitation | Restlessness, aggression | Variable |
| Psychosis | Hallucinations, delusions | Hours to days |
Epilepsy-Related Psychosis
Epilepsy-related psychosis is a serious issue for some. It makes people feel disconnected from reality, with hallucinations or delusions.
Managing epilepsy-related psychosis often means using antipsychotic drugs and adjusting seizure meds. A healthcare professional should guide this.
It’s key to understand the psychological effects of epilepsy for better care. Recognizing mental health challenges helps healthcare providers offer more support to those with epilepsy.
SUDEP: Sudden Unexpected Death in Epilepsy
It’s important for people with epilepsy to know about SUDEP. SUDEP is when someone with epilepsy dies suddenly and unexpectedly. Even after a full investigation, including an autopsy, the cause is not found.
Risk Factors for SUDEP
There are certain factors that can raise the risk of SUDEP. These include:
- Seizure frequency and severity: People with many or severe seizures are at higher risk.
- Poor adherence to anti-seizure medication: Not following the medication plan can increase the risk.
- History of generalized tonic-clonic seizures: This type of seizure is linked to a higher risk.
Warning Signs and Prevention
Even though SUDEP can happen without warning, there are signs and ways to prevent it:
- Monitoring seizure activity: Tracking seizures can help spot patterns or changes.
- Adherence to treatment plans: Following the treatment plan is key.
- Lifestyle adjustments: Changes like getting enough sleep and managing stress can lower seizure risk.
Support for Families Affected by SUDEP
It’s very hard to lose a loved one to SUDEP. Families can get support in many ways:
- Counseling and therapy: Professional help offers emotional support.
- Support groups: Meeting others who have lost loved ones can be helpful.
- Education and awareness: Learning about SUDEP helps families cope and may reduce risk for others.
By understanding the risks and taking steps, people with epilepsy and their families can lower the chance of SUDEP.
Sleep Disruptions and Nocturnal Seizures
For those with epilepsy, sleep is key. It can affect how often and how severe seizures are. The link between sleep and epilepsy creates a cycle of disruptions and seizures.
Identifying Nocturnal Seizure Symptoms
Nocturnal seizures happen when you’re asleep. They’re hard to spot. Look out for convulsions, strange noises, or odd movements while you’re sleeping.
Some signs of nocturnal seizures include:
- Unusual bedtime behaviors
- Unexplained injuries
- Daytime fatigue
- Confusion or disorientation upon waking
Sleep Deprivation as a Seizure Trigger
Not getting enough sleep can trigger seizures. It can make seizures more frequent and severe. Knowing how sleep affects epilepsy is key to managing it.
“Sleep disturbances are common among individuals with epilepsy, and addressing these disturbances is critical for improving overall quality of life.”
Management Strategies for Better Sleep
Good sleep is essential for those with epilepsy. Here are some ways to improve sleep:
| Strategy | Description |
| Establishing a bedtime routine | Having a regular bedtime routine helps your body know it’s time to sleep. |
| Creating a sleep-conducive environment | Make your bedroom dark, quiet, and cool to help you sleep better. |
| Avoiding stimulants before bedtime | Stay away from caffeine and screens before bed to sleep better. |
Using these strategies can help reduce nocturnal seizures. It can also improve your life quality.
Social and Relationship Challenges
People with epilepsy face many social and relationship challenges. The unpredictable nature of epilepsy can make them feel isolated and stigmatized. This affects many areas of their lives.
Stigma and Misconceptions
Even with better understanding, stigma and misconceptions about epilepsy remain. Many think it’s a mental or contagious disorder. This leads to social exclusion and discrimination.
Education and awareness are key to fighting these myths. By teaching the public about epilepsy, we can reduce stigma and create a more welcoming place.
Impact on Personal Relationships
Epilepsy can strain personal relationships. The fear of seizures and the need for constant care can put a lot of pressure on family and friends. Partners may feel overwhelmed by the responsibilities and uncertainties of caring for someone with epilepsy.
It’s important to have open communication and emotional support in relationships. Support groups offer a place for people to share their experiences and find understanding from others who face similar challenges.
Building Support Networks
Creating a strong support network is vital for those with epilepsy. This network can include family, friends, healthcare providers, and support groups. Having a supportive community can improve an individual’s quality of life, providing emotional support and practical help.
- Joining epilepsy support groups can connect individuals with others who understand their challenges.
- Educating family and friends about epilepsy can help alleviate fears and strengthen relationships.
- Professional counseling can provide individuals and families with the tools to cope with the emotional aspects of epilepsy.
Lifestyle Limitations and Restrictions
Living with epilepsy means making big changes to stay safe and healthy. People with epilepsy face many restrictions. These can affect their daily life, from driving to work and play.
Driving Regulations for People with Epilepsy
Driving is a big challenge for those with epilepsy. Rules about driving vary by state. But, most say you must be seizure-free for a while before you can drive.
- Seizure-free period: This time can be 3 to 12 months, depending on where you live.
- Medical clearance: Some places need a doctor’s okay before you can drive.
- Reporting seizures: You might have to tell the DMV about your seizures.
These rules help keep everyone safe. But, they can also limit your freedom and how you get around.
Employment Challenges
Jobs can be tough for people with epilepsy. Laws like the ADA help, but there are barriers.
- Job restrictions: Some jobs, like working high up or with heavy machines, might not be safe.
- Disclosure: It’s hard to know if to tell your employer about epilepsy. It might affect your job chances.
- Accommodations: Employers must make reasonable changes, like flexible hours for doctor visits.
Recreational Activity Restrictions
Fun activities can be limited for those with epilepsy. But, many are safe with some care. Some activities might be too risky.
- Swimming and bathing: It’s best not to swim alone. Showers are safer than baths.
- Sports and exercise: Some sports are too risky. But, many non-contact sports are okay and good for health.
- Travel: Traveling alone is hard. Tell your friends about your epilepsy and have a plan for emergencies.
Knowing these limits and taking steps to stay safe can help people with epilepsy enjoy life fully.
Special Considerations for Children with Epilepsy
Managing epilepsy in children is complex. It involves many aspects of their lives. Children with epilepsy face unique challenges that affect their development, education, and family life.
Educational Challenges
Children with epilepsy often face educational challenges. Their condition can affect their thinking and require frequent doctor visits. Schools can help by providing the right support and understanding.
These challenges include problems with memory, attention, and speed. Teachers and parents can create individualized education plans. This ensures the child gets the help they need to do well in school.
Behavioral Problems and Management
Children with epilepsy may have behavioral issues. These can include hyperactivity, impulsivity, or emotional problems. Managing these behaviors requires medication, therapy, and lifestyle changes.
Parents and caregivers should work with doctors to find triggers and manage these problems. This might involve behavioral modification techniques and creating a stable environment.
Family Dynamics and Caregiver Stress
Epilepsy in a child can change family dynamics. It can cause stress for caregivers. The emotional and physical demands of caring for a child with epilepsy can be tough.
Families should seek help from healthcare providers, support groups, and counseling. This helps manage caregiver stress. By taking care of themselves, caregivers can support their child better, creating a positive family environment.
Conclusion: Living Well Despite Epilepsy’s Challenges
Living with epilepsy comes with many challenges. These include physical health risks and social and psychological impacts. But, by understanding these challenges and using effective management strategies, people with epilepsy can live fulfilling lives.
Managing epilepsy needs a complete approach. This includes taking medication, making lifestyle changes, and having a support network. Using these tools helps reduce seizure risks and complications like status epilepticus and SUDEP.
Epilepsy support is key to coping with the condition. This support can come from family, friends, support groups, and healthcare providers. Together, people with epilepsy can handle the condition’s complexities and improve their quality of life.
In the end, living well with epilepsy requires medical treatment, lifestyle changes, and emotional support. By taking this holistic approach, individuals can overcome epilepsy’s challenges and enjoy a better life.
FAQ
What is epilepsy, and how is it defined as a neurological disorder?
Epilepsy is a brain disorder that causes seizures. These seizures happen when the brain’s electrical activity gets out of balance. Many things can trigger seizures, like genetics, head injuries, infections, and other health issues.
How common is epilepsy in the United States?
In the United States, about 3.4 million people have epilepsy. Every year, around 150,000 new cases are diagnosed.
What are the risks associated with seizures, and how can they be prevented?
Seizures can lead to injuries like head trauma, fractures, and burns. To stay safe, people with epilepsy should wear protective gear and avoid dangerous activities. They should also have a plan ready for when a seizure happens.
What is status epilepticus, and how is it treated?
Status epilepticus is a serious condition where seizures last too long without breaks. Doctors treat it with benzodiazepines and other medicines. People with this condition need to go to the hospital for care.
What are the common side effects of anti-seizure medications?
Anti-seizure medicines can make people feel drowsy, dizzy, and nauseous. They can also change how someone eats or feels. But, some medicines can cause serious side effects like allergic reactions, liver damage, or problems with blood cells.
Can epilepsy cause cognitive impairments, such as memory loss?
Yes, epilepsy can affect memory and thinking skills. This can happen because of the seizures themselves, the medicines, or the reason for the epilepsy. People might have trouble remembering things, processing information, or making decisions.
What is SUDEP, and how can its risk be reduced?
SUDEP stands for Sudden Unexpected Death in Epilepsy. It’s a rare but serious condition that can happen to people with epilepsy. To lower the risk, it’s important to control seizures well, get enough sleep, and watch for warning signs. Some medicines can also increase the risk, so it’s key to work with a doctor to find the right treatment.
How can sleep disruptions and nocturnal seizures be managed?
To manage sleep and seizures, try going to bed and waking up at the same time every day. Make your bedroom a place for sleep. Using devices that can detect seizures can also help. Also, talk to your doctor about your medicines and any sleep problems you might have.
How does epilepsy affect personal relationships and social interactions?
Epilepsy can make it hard to connect with others because of stigma and misunderstandings. But, by building a support network and educating others, you can overcome these challenges. Raising awareness about epilepsy can also help.
What lifestyle limitations and restrictions are associated with epilepsy?
Epilepsy can limit what you can do, like driving or working. But, with the right care and support, many people with epilepsy can live full lives. It’s all about finding ways to manage your condition and get the help you need.
How does epilepsy affect children, and what are the unique challenges for families?
Kids with epilepsy might struggle in school, have behavioral issues, and find it hard to make friends. Families may feel stressed and worried about their child’s future. But, with help from doctors, teachers, and support groups, families can face these challenges together.
Can anxiety cause convulsions or seizures?
Anxiety itself doesn’t cause seizures. But, for some people with epilepsy, it can trigger a seizure. Finding ways to manage stress, like through meditation or therapy, can help.
What are the warning signs of SUDEP, and how can it be prevented?
Signs of SUDEP can be hard to spot, but look out for changes in seizure frequency or severity, sleep problems, and heart rhythm issues. To lower the risk, focus on controlling seizures, getting enough sleep, and staying healthy. Watching for warning signs is also important.
How can memory loss associated with epilepsy be addressed?
To deal with memory loss, use tools like calendars and reminders. Try to stick to routines and practice brain exercises. Also, talk to your doctor about your medicines and any cognitive problems you’re facing.
Can people with epilepsy die from seizures, and what are the risks?
Yes, in rare cases, seizures can be fatal, either directly or through complications like SUDEP or status epilepticus. To stay safe, follow your treatment plan, watch for warning signs, and manage your seizures well. This can help reduce the risks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7079690/