Every year, about 12,000 people in the U.S. get diagnosed with tumors in the cranial region. This shows how important it is to have special surgery options Skull base surgery.
Skull base surgery is a highly complex operation. It deals with the area where the brain, skull, and facial structures meet. This surgery needs a lot of skill and knowledge of the detailed anatomy.
Because of its complexity, skull base surgery needs a thorough approach. This article will cover its importance, the anatomy involved, and what patients can expect.
Key Takeaways
- Cranial surgery is a delicate procedure that requires precision.
- The skull base is a complex anatomical region.
- Skull base operations are critical for addressing various conditions.
- Understanding the anatomy is key for successful surgery.
- Patients should know the risks and benefits of the procedure.
Understanding Skull Base Surgery

Skull base surgery is a set of surgical techniques for treating problems at the skull’s base. This area includes the underside of the brain, the skull base, and the top few vertebrae of the spinal column.
Definition and Purpose
Skull base surgery is a neurosurgical procedure aimed at treating issues at the skull’s base. It focuses on removing or treating abnormalities while keeping important structures safe.
This surgery is used for both cancerous and non-cancerous growths. It also treats other problems in this delicate area.
Common Indications
Common reasons for skull base surgery include:
- Tumors, whether benign or malignant
- Abnormal growths or cysts
- Other abnormalities affecting the skull base
Goals of Treatment
The main goals of skull base tumor surgery are to:
- Remove or significantly reduce the size of tumors or abnormalities
- Relieve symptoms caused by these conditions, such as pain or neurological deficits
- Preserve the function of surrounding nerves and brain structures
Anatomy of the Skull Base
The skull base is made up of several bones. It protects the brain and supports cranial nerves. It’s the floor of the cranial cavity and has many important features.
Key Anatomical Structures
The skull base is split into three parts: the anterior, middle, and posterior. Each part has unique structures important for skull base surgery.
Anterior Skull Base
The front part includes the frontal bone and cribriform plate. It also has parts of the ethmoid and sphenoid bones. This area is key because it has the olfactory bulbs and is near the paranasal sinuses.
Middle Skull Base
The middle part is made of the sphenoid bone and parts of the temporal bone. It’s home to the cavernous sinus, internal carotid artery, and important nerves.
Posterior Skull Base
The back part is the occipital bone and parts of the temporal bone. It has the foramen magnum, where the brainstem meets the spinal cord. It’s also near the cerebellum.
Knowing these structures is key for skull base surgery. It helps surgeons plan and do surgeries better. The skull base’s complexity shows why many experts are needed for cranial surgery.
- The anterior skull base is near the paranasal sinuses.
- The middle skull base has vital neurovascular structures.
- The posterior skull base has the foramen magnum and is near the cerebellum.
A leading neurosurgeon said, “The skull base’s detailed anatomy is vital for effective surgery.” This shows how important it is to know the anatomy well in cranial surgery.
Conditions Requiring Skull Base Surgery
Many disorders, like tumors and cerebrospinal fluid leaks, affect the skull base. They need precise surgery. The skull base is complex and can be hit by various problems. Some need surgery to ease symptoms and stop more issues.
Benign Tumors
Benign tumors often need skull base surgery. They’re not cancerous but can cause big problems. This is because they’re in a tricky spot and might press on important areas.
Meningiomas
Meningiomas grow from the meninges, which protect the brain and spinal cord. They can happen at the skull base. Symptoms include headaches, vision problems, or nerve issues, based on where and how big they are. Surgery for skull base tumors like meningiomas needs a team for the best results.
Acoustic Neuromas
Acoustic neuromas, or vestibular schwannomas, are benign tumors on the vestibular nerve. They can lead to hearing loss, tinnitus, and balance issues. Skull base tumor surgery for these aims to take out the tumor. It tries to keep the facial nerve and hearing, if it can.
Pituitary Adenomas
Pituitary adenomas are benign tumors of the pituitary gland at the brain’s base. They can be active (making too much hormone) or not. Symptoms depend on the tumor’s hormone making and size. Surgery, like skull base tumor surgery, aims to take out the tumor. It tries to get the pituitary gland working right again.
Choosing to have surgery for skull base tumors comes after careful checks. This includes scans and looking at the patient’s health. Surgery’s goal is to remove the tumor, ease symptoms, and better the patient’s life.
Types of Skull Base Surgery
Skull base surgery varies based on the disorder’s nature and location. The choice of technique depends on the condition, the patient’s health, and the surgeon’s skills.
Based on Approach
Skull base surgery is divided into two main approaches: transcranial and transfacial. Each has its own uses and benefits.
Transcranial Approaches
Transcranial methods access the skull base through the cranium. They’re used for superior or posterior conditions. Endoscopic skull base surgery is a minimally invasive option within this category.
Transfacial Approaches
Transfacial methods access the skull base through the face. They’re best for anterior conditions, like nasal or sinus issues. The choice between these approaches depends on the condition’s location.
| Surgical Approach | Indications | Benefits |
| Transcranial | Superior or posterior skull base conditions | Direct access to complex areas |
| Transfacial | Anterior skull base conditions, nasal cavity, or sinuses | Less invasive, potentially fewer complications |
The table above highlights the differences between transcranial and transfacial skull base surgery. As minimally invasive surgery improves, so will the field of skull base surgery.
Surgical Approaches to the Skull Base
Surgical methods for the skull base have seen big improvements. This brings new hope to those with complex conditions. The right surgery depends on where and what the problem is.
Traditional Open Approaches
Older open surgery methods were once the norm. Now, less invasive options are more common. But, knowing the old ways is important.
Subfrontal Approach
The subfrontal method gets to the skull base through the front. It’s great for tumors in the front part of the skull.
Pterional Approach
The pterional method helps with tumors in the sellar and suprasellar areas. It involves a cut near the pterion, where bones meet.
Retrosigmoid Approach
The retrosigmoid method is for tumors in the back of the skull. It gives good access with little brain movement.
These old methods have been improved and are used today, even with new, less invasive surgeries. They’re key for complex cases.
- Key benefits of traditional open approaches:
- Wide exposure of the surgical site
- Direct access to complex anatomical structures
- Flexibility in handling unexpected complications
Even though we’re moving towards less invasive surgeries, the old methods are sometimes the best choice.
Advanced Techniques in Skull Base Surgery
New surgical methods have changed skull base surgery a lot. They give patients more choices. These new ways have made recovery times shorter and results look better.
Minimally Invasive Procedures
Modern skull base surgery relies on small, precise methods. These techniques help surgeons work on hard-to-reach areas with less damage to nearby tissues. Endoscopic endonasal surgery and keyhole approaches are leading these changes.
Endoscopic Endonasal Surgery
This method uses a thin, flexible tube with a camera and light. It lets surgeons see the skull base through the nose. This way, there’s no need for big cuts outside the body, making healing faster and safer.
Keyhole Approaches
Keyhole surgery makes small cuts in the skull to get to the base. These small openings help surgeons work with great accuracy, causing less damage to the bone and tissue around it.
These new techniques offer many benefits. They make surgery less hard on the body and improve how things look after surgery. Here’s a quick look at some of the main advantages of these methods.
| Technique | Benefits | Outcomes |
| Endoscopic Endonasal Surgery | No external incisions, reduced risk of complications | Faster recovery, less scarring |
| Keyhole Approaches | Minimal disruption to surrounding tissues, precise interventions | Reduced trauma, quicker healing |
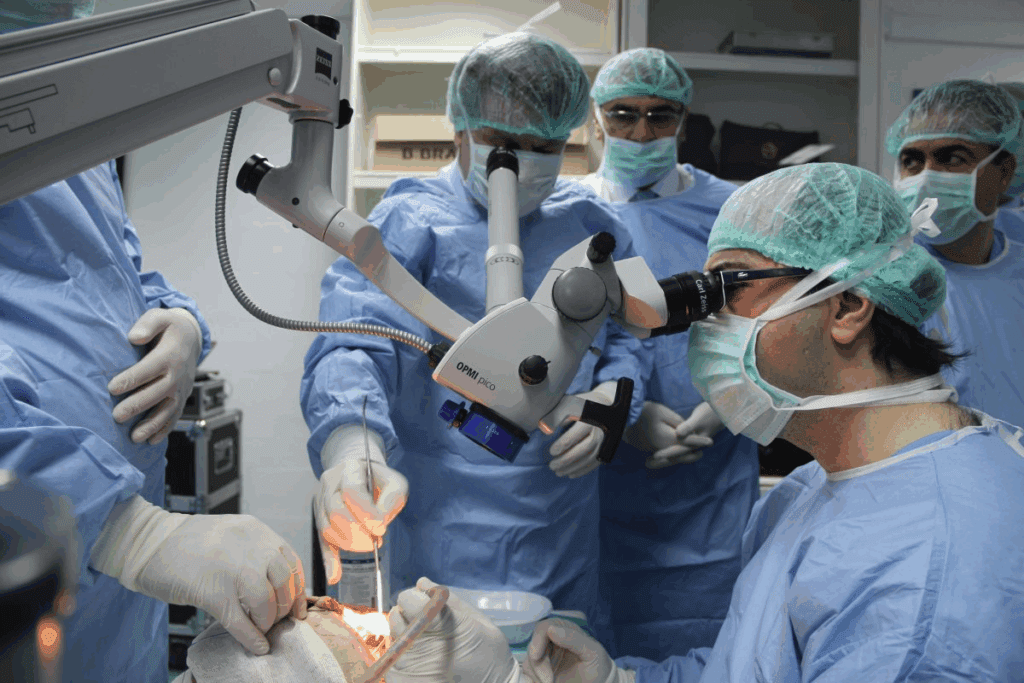
The Multidisciplinary Skull Base Surgery Team
Skull base surgery needs a team of experts working together. This team makes sure patients get the best care possible.
Key Specialists Involved
Many specialists are part of the skull base surgery team. Each one brings their own skills to help patients.
Neurosurgeons
Neurosurgeons are key in skull base surgery. They handle the brain’s complex structures. They remove tumors and fix damaged areas.
Otolaryngologists
Otolaryngologists, or ENT doctors, focus on ear, nose, and throat issues. They play a big role in skull base surgery.
Other Specialists
Other important team members include maxillofacial surgeons and radiologists. Maxillofacial surgeons know a lot about facial structures. Radiologists use images to help make surgical plans.
Risks and Outcomes of Skull Base Surgery
It’s important for patients to know about the risks and outcomes of skull base surgery. This surgery is needed for many conditions but is complex. It involves delicate areas of the skull, which means there are risks.
Potential Complications
Skull base surgery can lead to several complications. These include neurological problems, cerebrospinal fluid leaks, and infections. These risks can greatly affect how well a patient does after surgery.
Neurological Deficits
Neurological problems are a big risk in skull base surgery. These can be motor weakness, sensory disturbances, and cognitive impairments. The surgery’s complexity and the close location to important nerves increase these risks.
Cerebrospinal Fluid Leaks
Cerebrospinal fluid (CSF) leaks are another issue. These leaks can cause meningitis or other infections. It’s vital to quickly find and treat these leaks. To reduce this risk, surgeons use careful closure and watch patients closely after surgery.
Infection and Other Risks
Infection is a risk with any surgery, including skull base surgery. Other risks include bleeding, vascular injury, and problems with anesthesia. A team of experts works together to lower these risks. They plan carefully before surgery and care for patients well after.
The risks of skull base surgery highlight the need for a skilled team. To reduce risks, doctors choose patients carefully, use advanced techniques, and provide good care after surgery.
- Neurological deficits
- Cerebrospinal fluid leaks
- Infection
- Bleeding and vascular injury
By knowing these risks and taking steps to lessen them, doctors can help patients have better outcomes from skull base surgery.
Recovery and Rehabilitation After Skull Base Surgery
Recovering well after skull base surgery is very important. It needs a team effort to help the patient get better. This team works together to manage the patient’s care after surgery.
Immediate Postoperative Care
Right after surgery, it’s vital to watch for any problems. The patient’s vital signs and brain function are closely checked. This helps prevent any serious issues.
Intensive Care Management
Patients usually stay in the ICU right after surgery. Intensive care management means a team of experts keeps a close eye on them. They handle any problems that might come up.
Early Mobilization
Early mobilization helps avoid serious issues like blood clots. It also helps the patient get back to doing things they normally do. Healthcare workers help the patient move around and get back to their daily activities.
The main goal of care after surgery is to keep the patient safe and help them get back to normal. By focusing on careful management in the ICU and helping the patient move early, doctors can greatly improve how well patients do.
Conclusion
Skull base surgery has made big strides, leading to better lives for those with complex issues. It aims to fix various problems and tumors at the skull base. This area is key because it holds important structures.
The surgery’s benefits are wide-ranging. It can remove harmless tumors or fix complex blood vessel problems. Thanks to advanced techniques, doctors can offer treatments that change lives.
In summary, skull base surgery is a complex field needing teamwork. By working together, doctors from different fields can give patients the best care. This shows how important this medical area is for improving lives.
FAQ
What is skull base surgery?
Skull base surgery is a complex procedure. It involves operating on the base of the skull. This area is where the brain meets the spinal cord. It treats various conditions, like tumors and abnormalities.
What are the common indications for skull base surgery?
Skull base surgery treats benign tumors and other conditions. This includes meningiomas and acoustic neuromas. The goal is to remove the tumor while keeping other areas safe.
What are the different types of skull base surgery?
There are different types of skull base surgery. They depend on the approach used. This includes transcranial and transfacial approaches. The choice depends on the condition and the patient’s health.
What is endoscopic endonasal surgery?
Endoscopic endonasal surgery is a minimally invasive method. It uses an endoscope through the nose to access the skull base. This method leads to faster recovery and better looks.
What are the benefits of minimally invasive skull base surgery?
Minimally invasive surgery has many benefits. It leads to quicker recovery, less damage, and better looks. It also lowers the risk of complications and aids in faster healing.
Who is involved in the multidisciplinary skull base surgery team?
The team includes neurosurgeons, otolaryngologists, and radiologists. They work together for the best care. This teamwork ensures patients get the best treatment.
What are the possible complications of skull base surgery?
Complications can include neurological issues, infection, and leaks. Careful planning and precise surgery help avoid these. Close monitoring after surgery is also key.
What is the recovery process like after skull base surgery?
Recovery starts with care in an intensive care unit. Then, early movement and rehabilitation follow. The aim is to avoid complications and ensure a smooth recovery.
How is cranial surgery related to skull base surgery?
Cranial and skull base surgeries are closely related. Skull base surgery focuses on the base of the skull. Cranial surgery is broader, covering more areas.
What is the role of tumor removal surgery in skull base surgery?
Tumor removal is key in skull base surgery. It treats many conditions by removing tumors. The goal is to remove the tumor safely, preserving other areas.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11881544/




































