Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 900,000 Americans are affected by blood clots each year. Many cases could be prevented if warning signs are caught early. Learn the 5 alarming warning signs of blood clots stomach. Ignoring these symptoms can be a fatal mistake. Get the critical facts now.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
The condition can show up in different places, like the legs. This is called Deep Vein Thrombosis (DVT). Spotting DVT symptoms is important to avoid serious problems.
Key Takeaways
- Recognizing the signs of blood clots in the legs is crucial for saving lives.
- DVT symptoms include pain, swelling, and discoloration in the affected limb.
- A blood clot in leg can lead to severe complications if left untreated.
- The five warning signs will be discussed in detail in the following sections.
- Prompt medical attention is vital if symptoms get worse or don’t go away.
Understanding Blood Clots: Definition and Formation
It’s important to know what blood clots are and how they form. This knowledge helps us understand the risks they pose. Blood clots are a serious medical issue that needs quick attention.
What is a Blood Clot?
A blood clot, or thrombosis, is a mass of blood cells and platelets. It’s a natural response to injury to stop too much bleeding. But, if it happens the wrong way, it can cause big health problems.
The term “thrombosis definition” means a blood clot forms inside a blood vessel. This blocks blood flow in veins and arteries, causing health issues.
Recognizing the signs of blood clots in the legs is crucial for saving lives.

The blood clotting process starts with the body narrowing the blood vessel at an injury. Platelets stick to the injury, making a plug. Then, a series of chemical reactions creates a fibrin clot, making the plug stable.
The clotting stages are a series of chemical reactions. They lead to a stable clot. This is key to stop too much bleeding when a vessel is hurt.
Normal vs. Abnormal Blood Clotting
Blood clotting is normal when it happens after an injury. But, it can happen without an injury too. This can be because of genes, lifestyle, or health problems.
Abnormal clotting can cause serious problems like DVT, pulmonary embolism, or arterial thrombosis. Knowing the difference is key to spotting risks and preventing them.
- Normal blood clotting stops too much bleeding after an injury.
- Abnormal blood clotting happens without injury and can lead to serious health issues.
- Genetics, lifestyle, and health conditions can cause abnormal clotting.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Types of Blood Clots and Their Locations
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis happens when a blood clot forms in the deep veins, usually in the legs. Symptoms of DVT include swelling, pain, and discoloration of the affected limb. It’s key to spot these symptoms early to avoid serious issues.
DVT symptoms can be hard to notice, so it’s important to watch for any changes in the legs. Look for increased warmth or tenderness.
Pulmonary Embolism
A pulmonary embolism occurs when a blood clot travels to the lungs and blocks an artery. This is a serious condition that needs immediate medical help. Symptoms include shortness of breath, chest pain, and coughing up blood.
The severity of a pulmonary embolism can vary. But it’s critical to notice warning signs like sudden shortness of breath or chest pain that gets worse with deep breathing.
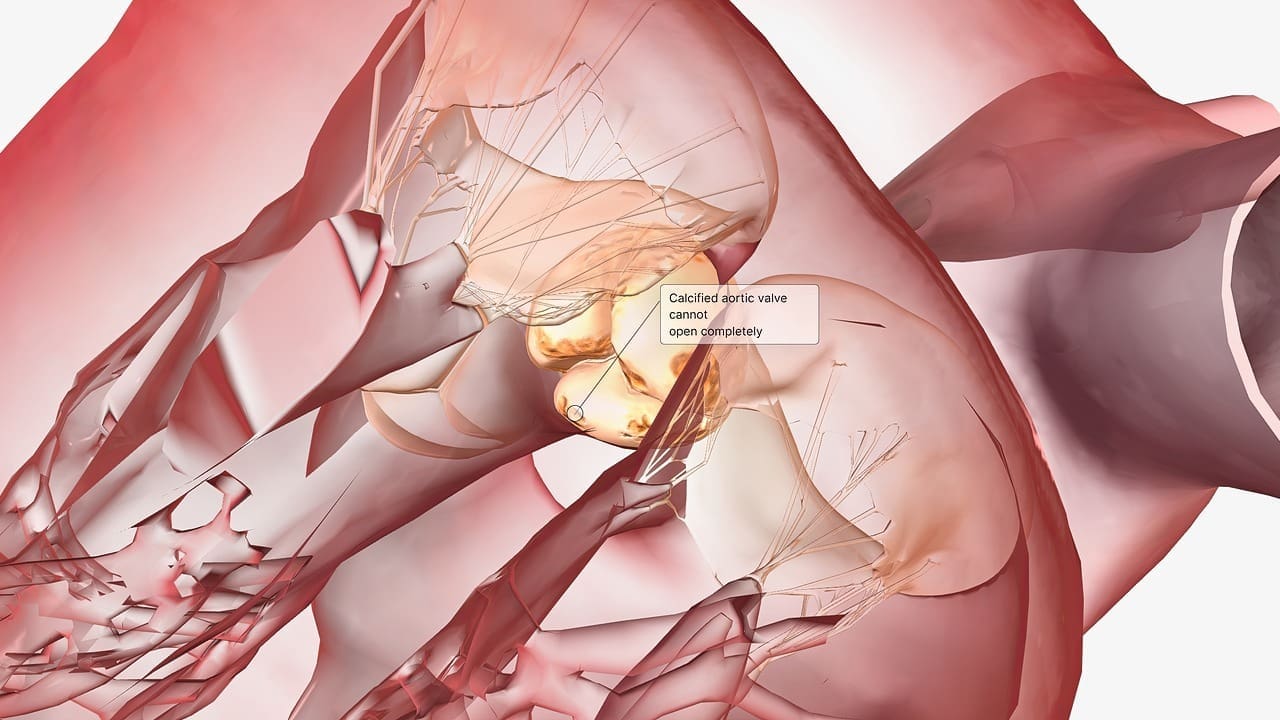
Arterial Thrombosis
Arterial thrombosis is when a blood clot forms in an artery. This can lead to serious issues like heart attack or stroke, depending on the artery’s location. Symptoms include severe pain, numbness, and coldness in the affected area.
Knowing the risk factors for arterial thrombosis, like high blood pressure and atherosclerosis, can help prevent and detect it early.
Superficial Thrombophlebitis
Superficial thrombophlebitis is a blood clot in a vein close to the skin’s surface. It causes pain, redness, and swelling along the vein. While less severe than DVT, it’s important to get medical evaluation.
Spotting the signs of superficial thrombophlebitis, like a tender or painful vein, is key. This helps in getting the right medical care.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Swelling in One Limb
Swelling in one limb, like a leg, is a common sign. This happens because the blood flow is blocked by the clot. If one leg or arm is much bigger than the other, it might mean you have a blood clot.
Pain or Tenderness
Pain or tenderness in a limb is another warning sign. The pain can feel like a dull ache or a sharp, intense pain. It’s often a cramping or soreness that doesn’t go away with rest. If the pain is bad or you have other symptoms, get medical help.
Skin Discoloration or Warmth
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Shortness of Breath
Shortness of breath is a serious sign. It means the clot might have moved to the lungs, causing a pulmonary embolism. This is very dangerous and needs quick medical help. If you suddenly can’t breathe well, call emergency services right away.
Knowing these signs can help you find a blood clot and get help fast. If you have any of these symptoms, see a doctor right away.
How to Recognize Blood Clots in Different Body Parts
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Location-Specific Symptoms
Recognizing the signs of blood clots in the legs is crucial for saving lives.
- Blood Clot in Leg: Swelling, pain, or tenderness in one leg.
- Blood Clot in Arm: Swelling, pain, or discoloration in one arm.
- Blood Clot in Lungs: Sudden shortness of breath, chest pain, or coughing.
Severity Indicators
Recognizing the signs of blood clots in the legs is crucial for saving lives.
- Intensity of pain or discomfort.
- Extent of swelling or redness.
- Presence of systemic symptoms such as fever.
Symptom Progression Timeline
The timeline for symptom progression can vary. Some people may have symptoms suddenly, while others may notice them gradually. Knowing how symptoms progress is key for getting medical help on time.
Symptoms can get worse quickly, sometimes in just hours or days. In other cases, symptoms may take weeks to appear. Being aware of this can help you get medical attention fast.
Blood Clots in Legs: Signs and Symptoms
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Early Stage DVT Symptoms
Recognizing the signs of blood clots in the legs is crucial for saving lives.
- Mild swelling in one leg
- A feeling of heaviness or aching in the leg
- Slight pain or tenderness, often described as a cramp or soreness
Watching for these symptoms is key, as they can get worse fast.
Advanced Symptoms of Leg Blood Clots
As DVT gets worse, symptoms get more serious. Advanced symptoms include:
- Significant swelling of the affected leg
- Increased pain or tenderness
- Warmth or redness of the skin around the affected area
- Visible veins
If you see these symptoms, get medical help right away.
How to Check for a Blood Clot in Your Leg
To check for a blood clot, look for symptoms and do a self-exam. Here’s how:
- Compare both legs to check for any differences in swelling.
- Feel for tenderness or pain along the veins.
- Check for warmth or redness.
If you’re unsure or notice anything odd, talk to a doctor.
| Symptom | Early Stage | Advanced Stage |
| Swelling | Mild | Significant |
| Pain/Tenderness | Slight | Increased |
| Skin Warmth/Redness | Minimal | Noticeable |
Recognizing the signs of blood clots in the legs is crucial for saving lives. If you notice any symptoms, get medical help right away.
Blood Clots in Lungs: Recognizing Pulmonary Embolism
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Unique Symptoms of Pulmonary Embolism
Symptoms of pulmonary embolism can differ from person to person. Common signs include shortness of breath, which can get worse over time. You might also feel chest pain when you breathe deeply, cough, or laugh.
Emergency Warning Signs
In serious cases, pulmonary embolism can be deadly. Look out for severe difficulty breathing, rapid or irregular heartbeat, and intense chest pain. If you see these signs, call emergency services right away.
Differences from Other Respiratory Conditions
Pulmonary embolism can be hard to diagnose because its symptoms are similar to other lung problems. But, if you suddenly start feeling shortness of breath and chest pain without a clear reason, it might be pulmonary embolism. Doctors usually use CT scans to make a correct diagnosis.
Recognizing the signs of blood clots in the legs is crucial for saving lives. can save lives. If you’re at risk for blood clots or have symptoms that worry you, talk to a doctor.
Blood Clots Stomach: Symptoms and Complications
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Mesenteric Venous Thrombosis Symptoms
Mesenteric venous thrombosis brings severe symptoms like abdominal pain, nausea, vomiting, and diarrhea. The pain is often worse than what a doctor finds during an exam.
Early recognition of these symptoms is key. It helps manage the condition and avoid serious problems like intestinal ischemia or infarction.
Abdominal Pain Patterns
Recognizing the signs of blood clots in the legs is crucial for saving lives.
- Pain may get worse with eating or moving.
- It can also be tender to the touch.
- In some cases, the pain may spread out, making it hard to find where it is.
Digestive Symptoms Associated with Stomach Blood Clots
People with mesenteric venous thrombosis may also have digestive symptoms. These include:
- Nausea and vomiting, which can sometimes be bloody.
- Diarrhea or constipation.
- Bloating and abdominal distension.
- Loss of appetite.
These symptoms can cause dehydration and electrolyte imbalances. It’s important to get medical help quickly to avoid long-term damage and complications.
Blood Clots in Heart and Brain: Life-Threatening Signs
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Cardiac Thrombosis Warning Signs
A blood clot in the heart, called cardiac thrombosis, can block blood flow. This can cause a heart attack. Look out for these symptoms:
- Chest pain or discomfort
- Shortness of breath
- Lightheadedness or dizziness
- Pain or discomfort in one or both arms, the back, neck, jaw, or stomach
It’s important to recognize these signs early. This can help treat the problem and reduce damage.
Stroke Symptoms from Blood Clots
A stroke happens when a blood clot blocks the brain’s blood supply. Or when a blood vessel in the brain bursts. Watch for these symptoms:
- Sudden numbness or weakness in the face, arm, or leg, on one side
- Confusion, trouble speaking, or understanding speech
- Sudden trouble seeing in one or both eyes
- Dizziness, loss of balance, or trouble walking
Acting F.A.S.T. can help you remember stroke signs:
- F – Face: Ask the person to smile. Does one side of their face droop?
- A – Arm: Ask the person to raise both arms. Does one arm drift downward?
- S – Speech: Ask the person to repeat a simple sentence. Is their speech slurred?
- T – Time: Time is critical. If symptoms show, call 911 right away.
When to Call 911 Immediately
If you or someone else has heart attack or stroke symptoms, call 911 or your local emergency number right away. Quick medical help can greatly improve outcomes.
| Condition | Key Symptoms | Action |
| Cardiac Thrombosis | Chest pain, shortness of breath, lightheadedness | Call 911 |
| Stroke | Numbness, confusion, vision trouble, dizziness | Call 911, Act F.A.S.T. |
Risk Factors for Developing Blood Clots
Many things can increase your chance of getting blood clots. These include your genes, lifestyle, and some health conditions. Knowing these risks can help you prevent them and get help if you notice any symptoms.
Genetic Predispositions
Genetics are a big part of blood clot risk. Some genetic conditions can make your blood clot more easily. For example, Factor V Leiden thrombophilia can raise your risk of deep vein thrombosis (DVT).
Key genetic risk factors include:
- Factor V Leiden thrombophilia
- Antithrombin deficiency
- Protein C deficiency
- Protein S deficiency
Lifestyle Factors
What you do every day can also affect your risk. Being inactive, overweight, and smoking can all increase your risk.
“Maintaining a healthy lifestyle, including regular physical activity and a balanced diet, can help reduce the risk of blood clots.”
Medical Conditions that Increase Risk
Some health issues can also raise your risk. These include cancer, heart disease, and problems with blood clotting.
| Medical Condition | Increased Risk |
| Cancer | Some cancers can increase clotting factors in the blood. |
| Heart Disease | Conditions like atrial fibrillation can lead to clot formation. |
| Clotting Disorders | Conditions that affect the blood’s ability to clot properly. |
Smoking and Blood Clots Connection
Smoking is a big risk for blood clots, mainly in the legs and lungs. It damages blood vessel linings, making them more likely to clot.
Quitting smoking can greatly lower your risk of blood clots and heart disease. There are many resources and support groups to help you quit.
Treatment Options for Blood Clots
Treating blood clots involves many factors, like where the clot is and the patient’s health history. A good treatment plan is made just for the person, taking into account their unique situation.
Anticoagulant Medications
Anticoagulant drugs are key in treating blood clots. They stop the clot from getting bigger and prevent new ones. Drugs like heparin and warfarin are common. Newer drugs, like rivaroxaban and apixaban, don’t need blood tests as often.
Thrombolytic Therapy
For serious blood clots, like pulmonary embolism or stroke, thrombolytic therapy is used. It involves drugs that break down the clot. Starting this treatment quickly is very important.
Surgical Interventions
Surgery might be needed for some blood clots. Thrombectomy is a procedure to remove the clot. Sometimes, a vena cava filter is put in to stop clots from reaching the lungs.
Recovery and Follow-up Care
Getting better from a blood clot takes more than just treatment. It also means ongoing care to stop it from happening again. This includes watching the anticoagulant therapy, making lifestyle changes, and managing health issues that might have caused the clot. Regular check-ups with a doctor are key to adjust the treatment and handle any issues.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Prevention Strategies for Blood Clots
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Lifestyle Modifications
Changing your lifestyle can help prevent blood clots. Regular physical activity boosts circulation and lowers clot risk. Aim for 30 minutes of moderate exercise daily.
Maintaining a healthy weight is key, as extra weight strains the circulatory system. Eating a balanced diet with fruits, veggies, whole grains, and lean proteins helps keep a healthy weight.
Also, staying hydrated by drinking lots of water is important. Dehydration can increase clot risk. Limit alcohol and avoid smoking to keep circulation and heart health good.
Preventive Medications
Preventive meds might be needed for those at high risk of blood clots. Anticoagulant medications prevent clots and lower risks of DVT and pulmonary embolism.
It’s vital to follow your doctor’s advice on these meds. They can have side effects and interact with other drugs. Regular check-ups are needed to ensure they’re working safely and effectively.
Special Considerations for High-Risk Individuals
People with certain health conditions or risk factors need extra care to prevent blood clots. For instance, those with DVT or pulmonary embolism history should take precautions seriously.
Compression stockings are helpful for some, like during long immobility periods. They improve leg circulation and lower clot risk.
“For individuals at high risk, preventive measures can significantly reduce the risk of blood clot-related complications.”
Travel-Related Prevention Tips
Travel, like long flights or car rides, raises blood clot risk due to sitting for long. To lower this risk, stay active by stretching and moving regularly during travel.
Choose an aisle seat for easier movement. Wear loose, comfy clothes. Consider compression stockings for long trips.
Being aware of travel risks and taking steps can help avoid blood clots. This makes travel safer and healthier.
Conclusion: When to Seek Medical Help for Suspected Blood Clots
It’s important to know the signs of a blood clot and get medical help fast. Symptoms like swelling, pain, or trouble breathing mean you should see a doctor right away.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
If you’re at risk or notice something odd, talk to a doctor. Being informed and taking action can lower your risk. It also makes sure you get the right care if you do get a blood clot.
FAQ
What is a blood clot and how does it form?
A blood clot is a gel-like mass made of blood cells and platelets. It forms when an injury or other factors start the clotting process.
What are the symptoms of a blood clot in the leg?
Symptoms of a blood clot in the leg include swelling and pain. You might also see tenderness, skin discoloration, and warmth. Sometimes, there are no symptoms at all.
How do I check for a blood clot in my leg?
To check for a blood clot, look for swelling, redness, or warmth in your leg. Check for tenderness or pain when you stand or walk. If you think you have a blood clot, get medical help right away.
What is deep vein thrombosis (DVT)?
Recognizing the signs of blood clots in the legs is crucial for saving lives.
What are the risk factors for developing blood clots?
Risk factors for blood clots include genetic predispositions and lifestyle factors like smoking and obesity. Medical conditions like cancer and heart disease also increase the risk. Certain medications can also be a factor.
Recognizing the signs of blood clots in the legs is crucial for saving lives.
Yes, blood clots can be prevented. You can do this through lifestyle changes like regular exercise and maintaining a healthy weight. Avoiding prolonged immobility is also key. High-risk individuals may be prescribed preventive medications.
What are the treatment options for blood clots?
Treatment for blood clots includes anticoagulant medications and thrombolytic therapy. Surgical interventions and recovery care are also options. The best treatment depends on the blood clot’s location and severity.
What are the symptoms of a pulmonary embolism?
Symptoms of a pulmonary embolism include shortness of breath and chest pain. You might also cough up blood and have a rapid heart rate. It’s a serious condition that needs immediate medical attention.
Can a blood clot cause a stroke?
Yes, a blood clot can cause a stroke if it travels to the brain. Symptoms include sudden weakness, numbness, or paralysis. You might also have trouble speaking or understanding speech, and experience sudden vision changes.
What is the connection between smoking and blood clots?
Smoking damages blood vessel linings, making them more prone to clotting. Quitting smoking can help lower your risk of blood clots.
How can I reduce my risk of developing blood clots when traveling?
To lower your risk of blood clots while traveling, stay hydrated and move regularly. Avoid crossing your legs or ankles for long periods. Wearing compression stockings or taking preventive medications can also help if you’re at high risk.