Last Updated on December 1, 2025 by Bilal Hasdemir
Did you know nearly 100,000 people in the United States have brain surgery every year? These surgeries can change lives. It’s important to know what makes them successful for patients and their families. Get the hopeful, amazing facts on the skull surgery success rate. Discover the critical factors that influence patient outcomes.
The neurosurgery survival rate has gotten better thanks to new medical tech and methods. But, the success rate of skull surgery changes a lot. It depends on the surgery type, the condition, and the patient’s health.
Key Takeaways
- The success rate of skull surgery depends on various factors, including the type of procedure and the patient’s health.
- Recent medical advancements have improved brain surgery outcomes.
- Understanding the factors that influence neurosurgery survival rate is important for patients.
- The success rate of skull surgery can vary widely depending on the specific procedure.
- Patients’ overall health plays a big role in determining the outcome of brain surgery.
Understanding Skull Surgery: Types and Purposes
It’s important for patients to know about the different skull surgeries. Skull surgery, or craniotomy, means removing part of the skull to reach the brain. It’s used for many issues, like brain tumors, aneurysms, and head injuries.
Common Types of Cranial Procedures
Cranial procedures depend on the condition and the patient’s health. Craniotomy is common, where a skull part is removed to relieve brain pressure or remove tumors. Other methods include trephination, drilling a hole, and craniectomy, removing a skull part to let the brain expand.
Medical Conditions Requiring Skull Surgery
Skull surgery treats many medical issues. These include brain tumors, aneurysms that could bleed, and head injuries needing quick surgery. The success of these surgeries depends on the craniotomy success rate and neurological surgery advancements.
Evolution of Neurosurgical Techniques
Neurosurgery has made big strides, improving intracranial surgery outcomes. New methods, like less invasive surgery and better imaging, cut down recovery times. This means patients now have better open skull surgery results than before.
Skull Surgery Success Rate: Statistical Overview
The success rates of skull surgery give us important insights. They help both patients and doctors understand how well different surgeries work.

Success in neurosurgery can be seen in many ways. This includes how long patients live, if their symptoms get better, and if their life quality improves. Looking at national data and trends helps us see how well skull surgeries are doing overall.
Defining “Success” in Neurosurgery
Figuring out what makes a surgery successful is complex. It involves looking at how long patients live, if their symptoms get better, and if their life quality improves. Neurosurgery recovery statistics are key in this process, giving us data on how patients do.
For example, studies show that more patients are surviving brain surgery today. This is thanks to better technology and surgical methods.
Comparing Success Rates Across Different Facilities
Looking at how different places do in surgery helps us learn and improve. Things like the skill of the surgical team, the quality of care, and the availability of top-notch equipment all play a part. These factors can make success rates vary.
| Facility Type | Success Rate | Survival Rate |
| Specialized Neurosurgery Centers | 85% | 95% |
| General Hospitals | 75% | 90% |
| Research Hospitals | 80% | 92% |
By studying these numbers, healthcare teams can aim to make surgery outcomes better for everyone.
Factors Influencing Neurosurgical Outcomes
It’s important to know what affects neurosurgical results. Neurosurgery is complex and delicate. Many factors can change how well a surgery goes.
Patient-Related Factors
Things like age, health, and other health issues matter a lot. Older patients or those with health problems might face more risks. Preoperative evaluation helps find these issues and plan better.
Surgeon Experience and Hospital Volume
The neurosurgeon’s experience and the hospital’s volume also matter. Research shows that doctors who do more surgeries get better results. Also, hospitals that do more neurosurgery have better tools and teams.
| Factor | Impact on Outcome |
| Surgeon Experience | Higher experience correlates with better outcomes |
| Hospital Volume | Higher volume hospitals tend to have better outcomes |
| Technological Resources | Advanced technology improves precision and effectiveness |
Technological Resources and Equipment
Having the right technology is key. Modern neurosurgery uses innovative technologies like intraoperative MRI and neuro-navigation. These tools make surgeries more precise and effective.
Knowing these factors helps patients and doctors make better choices. This leads to better results for neurosurgery.
Craniotomy Success Rate and Recovery Statistics
Craniotomy success rates are key in neurosurgery. They look at survival, recovery, and long-term life quality. This surgery removes part of the skull to treat brain issues like tumors and injuries.
Survival Rates for Standard Craniotomies
Most patients do well after standard craniotomies. Studies show a 90% survival rate. But, this can change based on the condition treated.
| Condition | Survival Rate | Recovery Time |
| Brain Tumor | 85% | 6-12 months |
| Aneurysm | 90% | 3-6 months |
| Traumatic Injury | 80% | Varies |
Functional Outcomes After Recovery
Recovery from craniotomy depends on the patient’s pre-surgery health, the complexity of the operation, and post-operative care. Many patients experience significant improvements in mobility and cognitive function.
Long-term Quality of Life Considerations
Long-term life quality is very important for craniotomy patients. Many go back to their usual lives. But, some face ongoing issues like tiredness, thinking changes, or mood shifts. It’s vital to have ongoing support and care.
In summary, craniotomy success rates and recovery stats show the complex nature of neurosurgery. Knowing these details helps patients and doctors make better choices about treatment.
Brain Tumor Surgery Success by Type and Location
Understanding brain tumor surgery is key for patients. Success depends on the tumor type and where it is in the brain.
Benign vs. Malignant Tumor Outcomes
Benign tumors are non-cancerous and often have better surgery outcomes. They usually have a high success rate for removal. Patients with benign tumors often fully recover with little chance of the tumor coming back.
Malignant brain tumors are harder to deal with. They grow fast and can spread to other brain areas. Surgery can help, but the outlook is not as good.
Impact of Tumor Location on Success Rates
Where the tumor is also matters a lot. Tumors in easy-to-reach areas do better with surgery. But, tumors in hard-to-reach spots can make surgery riskier and less effective.
Recurrence Statistics and Secondary Procedures
Recurrence is a big worry, mainly for malignant tumors. How likely it is to come back depends on the tumor and surgery success. Some might need more treatments like surgery, radiation, or chemo to fight it back.
Knowing these details helps patients and doctors make better choices. It’s about understanding the tumor type, location, and chances of coming back. This way, patients can make informed decisions about their treatment.
Specialized Skull Procedures and Their Outcomes
Skull procedures like skull base surgery and brain aneurysm surgery are complex. They require precise techniques and are for life-threatening conditions.
Skull Base Surgery Success Rates
Skull base surgery is a delicate operation at the skull’s base. It has seen a big improvement in success rates. This is thanks to better surgical techniques and technology.
Studies show the success rate can be between 80% to 95%. This depends on the case’s complexity and the surgical team’s experience.
Brain Aneurysm Surgery Outcomes
Brain aneurysm surgery needs a lot of skill and precision. The success rate varies based on the aneurysm’s size, location, and the patient’s health. Generally, it has a high success rate, with some studies showing over 90% success.
Skull Reconstruction Success Statistics
Skull reconstruction is needed after injuries or tumor removals. Its success depends on the damage’s extent and the reconstruction materials. Modern methods and materials have greatly improved outcomes, with high patient satisfaction.
In conclusion, the success rates of skull procedures like skull base surgery, brain aneurysm surgery, and skull reconstruction vary. Understanding these factors and neurosurgical advancements helps patients and surgeons make better decisions.
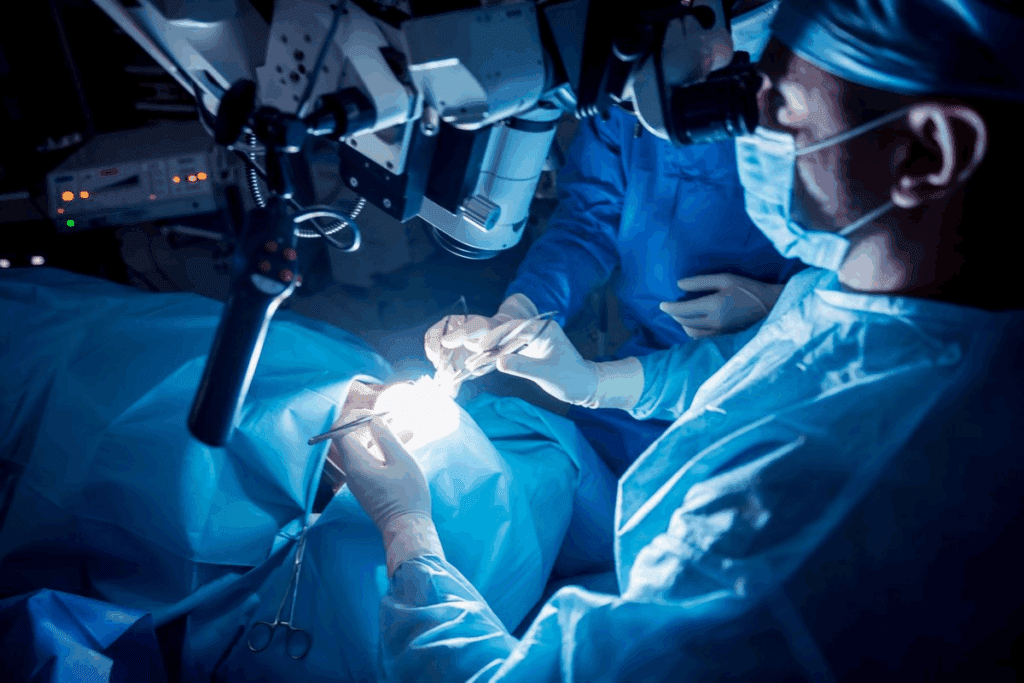
Minimally Invasive Brain Surgery: Improved Outcomes
The field of neurosurgery has seen a big change towards less invasive brain surgery. This change has made recovery better and reduced complications. It has also given patients safer options with fewer risks.
Advantages of Endoscopic Approaches
Endoscopic skull base surgery is a key example of less invasive brain surgery. It uses a thin, flexible tube with a camera and light. This lets surgeons work through small cuts. Studies show it has lower risks and faster recovery times than old surgery methods.
Key Benefits of Endoscopic Surgery:
- Smaller cuts mean less damage to tissue
- Less chance of infection and problems
- Less pain after surgery
- Shorter stays in the hospital and quicker to get back to normal
Innovations in Laser Ablation and Focused Ultrasound
Laser ablation and focused ultrasound are big steps forward in brain surgery. Laser ablation uses a laser to kill targeted brain tissue. Focused ultrasound uses sound waves to do the same without cuts. Both are great for treating some brain tumors and conditions like essential tremor.
“The precision and non-invasive nature of focused ultrasound has opened new avenues for treating neurological disorders that were previously challenging to address surgically.”
Comparing Traditional and Minimally Invasive Approaches
Traditional open surgery and minimally invasive techniques are very different. Traditional surgery needs bigger cuts and more tissue damage. This leads to longer recovery times and more risks. On the other hand, less invasive methods aim to cause less damage, have shorter recovery times, and lower risks.
| Aspect | Traditional Surgery | Minimally Invasive Surgery |
| Incision Size | Larger | Smaller |
| Recovery Time | Longer | Shorter |
| Risk of Complications | Higher | Lower |
As technology and techniques improve, we can expect even better results from less invasive brain surgery. This will bring new hope to those needing neurosurgery.
Skull Surgery Complications and Risk Assessment
Skull surgery is often a lifesaver but comes with big risks. Patients and doctors must think carefully about these risks. Knowing about these complications helps figure out the surgery’s overall risk.
Common Complications and Their Frequencies
Skull surgery can lead to infections, bleeding, nerve problems, and leaks of cerebrospinal fluid (CSF). How often these happen depends on the surgery type, patient health, and how the surgery is done.
| Complication | Frequency Range |
| Infection | 2-5% |
| Bleeding | 1-3% |
| Neurological Deficits | 5-15% |
| CSF Leaks | 1-2% |
Risk Stratification Models
Risk models help find out who might face more problems. They look at age, health issues, and how complex the surgery is.
Strategies for Complication Prevention
To avoid problems, planning is key. Surgeons use careful techniques and focus on recovery. They might use antibiotics, manage blood pressure, and get patients moving early.
Questions to Ask Your Neurosurgeon About Success Rates
To make informed decisions, patients must ask the right questions about neurosurgery success rates. Knowing what affects outcomes is key to better care and recovery.
Understanding Your Personal Risk Factors
Talking about your personal risk factors with your neurosurgeon is vital. These include your age, health, and any other health issues. Asking how these can affect brain surgery patient survival rates is important.
Surgeon-Specific Experience and Outcomes
Knowing your surgeon’s experience with your procedure can give you peace of mind. Ask about their success rate and how many times they’ve done it. Understanding surgeon-specific experience helps predict a good outcome.
Hospital Resources and Support Systems
The hospital’s quality of care also affects neurosurgery recovery statistics. Inquire about the hospital’s resources, like ICU and rehab services. A well-equipped hospital can greatly improve your chances of a good recovery.
| Category | Questions to Ask | Importance |
| Personal Risk Factors | How do my age and health status affect my surgery? | High |
| Surgeon Experience | What is your success rate with this procedure? | High |
| Hospital Resources | What post-operative care services are available? | Medium |
By asking these questions, patients can better understand what to expect. This helps them make more informed decisions about their care.
Conclusion: Making Informed Decisions About Skull Surgery
It’s important for patients to know about the success rates and risks of skull surgery. The skull surgery success rate changes based on the procedure, the medical condition, and the patient’s health.
Looking at neurosurgery survival rate stats and brain surgery outcomes helps patients choose their treatment. This article covered skull surgery’s different aspects, like types, purposes, complications, and results.
Patients should talk to their neurosurgeon about their risks and expected results. This way, they can make smart choices about their care. With the right info, patients can face skull surgery with confidence, knowing what to expect and how to get the best results.
FAQ
What is the overall success rate of skull surgery?
Skull surgery success rates vary. They depend on the procedure type, the medical condition, and the patient’s health. Success rates usually range from 80% to 95% for many surgeries, like craniotomies and brain tumor surgeries.
How do neurosurgical techniques impact skull surgery success rates?
New neurosurgical techniques have greatly improved success rates. These include minimally invasive methods and better imaging. They help surgeons work more precisely, leading to fewer complications and faster healing.
What factors influence the success rate of craniotomy procedures?
Several factors affect craniotomy success rates. These include the medical condition, patient age, and overall health. Surgeon experience, hospital volume, and technology also play key roles.
What are the survival rates for patients undergoing brain tumor surgery?
Brain tumor surgery survival rates vary. They depend on the tumor type and location, and the patient’s health. Patients with benign tumors generally have better survival rates than those with malignant tumors.
How do minimally invasive brain surgery techniques compare to traditional approaches?
Minimally invasive brain surgery offers advantages. It includes less recovery time, less tissue damage, and fewer complications. This is compared to traditional methods.
What are the possible complications of skull surgery, and how can they be prevented?
Skull surgery complications include infection, bleeding, and neurological damage. To prevent these, careful patient selection, precise surgical technique, and post-operative monitoring are key.
How can patients assess their personal risk factors for skull surgery?
Patients can assess their risk by talking to their neurosurgeon. They should discuss their medical history and undergo thorough evaluations before surgery.
What questions should patients ask their neurosurgeon about success rates and outcomes?
Patients should ask about the surgeon’s experience with the procedure. They should also inquire about the hospital’s resources and the surgery’s risks and complications.
What is the impact of surgeon experience on skull surgery success rates?
Surgeon experience greatly affects success rates. More experienced surgeons tend to have better outcomes. They have honed their skills and can handle complex cases more effectively.
How do hospital resources and support systems affect skull surgery outcomes?
Hospital resources and support systems are critical. They include intensive care units and rehabilitation services. Hospitals with strong resources and support tend to have better outcomes and lower complication rates.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1916268