Last Updated on December 1, 2025 by Bilal Hasdemir
Millions of people worldwide face neurological conditions. Nearly 1 in 6 individuals suffer from a neurological disorder, says the World Health Organization.
Patients in a neuro unit or neuro ICU have severe or life-threatening conditions. They need close monitoring and specialized care. This includes those with traumatic brain injuries, stroke, brain infections, or needing care after neurosurgery.
The care in these units is vital. It greatly affects patient outcomes and recovery chances.
Key Takeaways
- Neurological disorders affect a significant portion of the global population.
- Neuro ICU patients often have severe or life-threatening conditions.
- Specialized neurological care is critical for patient recovery.
- Traumatic brain injuries and stroke are common conditions treated.
- Close monitoring and post-operative care are key components of neuro unit care.
Understanding Neuro Units in Modern Healthcare
Neuro units play a key role in today’s healthcare. They offer specialized care for those with neurological issues. These units focus on the complex needs of patients with various neurological disorders.
Definition and Purpose of Neuro Units
A neuro unit, also known as a neuroscience or neurological intensive care unit, is a special part of a hospital. It treats patients with severe or life-threatening neurological conditions. The main goal is to give close monitoring and specialized care. This is done with advanced technology and a team of neuroscience unit specialists.
Different Types of Neurological Care Settings
Neurological care happens in different places, from general wards to specialized neuro units. The care setting depends on the patient’s condition. For example, those with acute stroke or traumatic brain injury need the intense care of a neuro unit.
Evolution of Neurological Care in the US
Neurological care in the US has changed a lot over time. This change comes from new medical technology, treatment methods, and understanding of neurological conditions. These changes have led to better patient results and higher quality care.
| Aspect | Past | Present |
| Monitoring Technology | Limited to basic vital sign monitoring | Advanced neuromonitoring equipment |
| Treatment Approaches | Generalized care protocols | Personalized treatment plans based on condition and patient needs |
| Staff Specialization | General medical staff | Specialized neuroscience unit specialists and neurocritical care teams |
The creation of neuro units is a big step in neurological care. It gives patients the specialized treatment they need for the best results.
Common Types of Neuro Unit Patients
Neuro units care for many patients with different neurological disorders. These disorders are both acute and chronic. Each patient needs special care because of the complexity and severity of their condition.
Acute vs. Chronic Neurological Conditions
Patients in neuro units fall into two main groups: those with acute and those with chronic conditions. Acute conditions, like stroke or brain injury, need quick and intense care. Chronic conditions, such as epilepsy or multiple sclerosis, require ongoing management and monitoring.
Acute conditions have sudden symptoms that need fast diagnosis and treatment. For example, stroke patients benefit from quick thrombolytic therapy. Chronic conditions, on the other hand, need continuous care and adjustments to treatment plans.
Age Demographics in Neuro Units
The age of patients in neuro units varies a lot. This shows the wide range of neurological conditions treated. Both young children and older adults are treated, each needing special care.
| Age Group | Common Conditions | Care Considerations |
| Pediatric | Seizure disorders, congenital neurological conditions | Family-centered care, developmental support |
| Adult | Stroke, traumatic brain injury, multiple sclerosis | Rehabilitation, medication management |
| Geriatric | Dementia, stroke, Parkinson’s disease | Comprehensive geriatric assessment, fall prevention |
Stroke Patients: The Most Common Neuro Unit Admission
Neuro units play a key role in caring for stroke patients. They need quick and specialized care. A stroke happens when blood flow to the brain stops or slows down. This prevents the brain from getting the oxygen and nutrients it needs.
There are two main types of stroke: ischemic and hemorrhagic. Knowing the difference is key to treating them right.
Ischemic vs. Hemorrhagic Stroke
Ischemic strokes make up about 87% of all strokes. They happen when a blood vessel in the brain gets blocked. Hemorrhagic strokes, on the other hand, are caused by bleeding in or around the brain. This can be due to a burst aneurysm or high blood pressure.
| Stroke Type | Cause | Treatment Approach |
| Ischemic | Blood vessel obstruction | TPA, thrombectomy |
| Hemorrhagic | Bleeding in or around the brain | Surgical intervention, management of intracranial pressure |
Post-Stroke Rehabilitation Needs
Rehabilitation is vital for stroke patients. It helps them regain lost functions and adjust to any lasting changes. The process includes physical, occupational, speech, and cognitive therapy.
TPA and Interventional Treatments
Tissue Plasminogen Activator (TPA) is a drug used to dissolve clots in ischemic stroke patients. It must be given quickly after symptoms start. Other treatments, like mechanical thrombectomy, may also be used to remove the clot.
TPA treatment works best when given fast. This shows how important quick medical action is in stroke cases.
Traumatic Brain Injury Patients
Understanding traumatic brain injuries is key to giving good neurological care. TBI patients face unique challenges because of the injury’s complexity and variability.
Severity Classifications
The Glasgow Coma Scale (GCS) is used to measure TBI severity. Scores range from 3 to 15, with higher scores showing less severe injuries. Mild TBI (GCS 14-15) might cause brief loss of consciousness. On the other hand, moderate (GCS 9-13) and severe (GCS 3-8) TBI can lead to longer unconsciousness or more serious cognitive issues.
Common Causes
Falls, car accidents, sports injuries, and physical assaults are common causes of TBI in the U.S. Young adults and the elderly are at higher risk.
Recovery Expectations and Challenges
Recovery from TBI varies a lot. It depends on the injury’s severity and the patient’s individual factors. Some patients recover quickly, while others face long-term challenges in cognition, emotions, and physical health. A team of specialists works together to help these patients.
Intracranial Pressure Monitoring
Monitoring intracranial pressure (ICP) is vital for severe TBI. High ICP can cause more brain damage. So, constant monitoring helps doctors act fast. They use intraventricular catheters and intraparenchymal monitors for this.
Spinal Cord Injury Patients
Spinal cord injuries are tough for patients, families, and doctors. They can change a person’s life a lot. They need a lot of care and support.
Types of Spinal Cord Injuries
There are two main types of spinal cord injuries. Complete spinal cord injuries mean no function below the injury. Incomplete injuries allow some function or feeling.
Knowing if an injury is complete or incomplete helps doctors plan treatment and rehabilitation.
Rehabilitation Approaches for SCI Patients
Rehab for spinal cord injuries aims to help patients live better lives. It includes physical therapy, occupational therapy, and assistive technology for daily tasks.
| Rehabilitation Approach | Description | Benefits |
| Physical Therapy | Improves mobility and strength | Boosts physical function and lowers risks |
| Occupational Therapy | Teaches skills for daily living | Helps with independence in daily tasks |
| Assistive Technology | Includes devices for mobility and communication | Improves life quality and independence |
Long-term Care Considerations
Long-term care for spinal cord injury patients is key. It involves managing health issues, preventing new problems, and giving ongoing support. This includes regular doctor visits, physical therapy, and mental health support.
Assistive Technology for SCI Patients
Assistive technology is very important for spinal cord injury patients. Tools like wheelchairs, prosthetics, and communication aids help them live more independently and improve their quality of life.
Understanding spinal cord injuries and using full care strategies can greatly help patients. Healthcare providers can make a big difference in their lives.
Patients with Seizure Disorders
Seizure disorders, like epilepsy, are tough for patients and doctors in neuro units. They need a detailed plan for managing and treating these conditions.
Epilepsy and Other Seizure Conditions
Epilepsy is a brain disorder that causes seizures to happen again and again. Other seizure conditions can come from injuries or infections. Knowing the cause is key to managing them well.
Acute Seizure Management
Acute seizure management means acting fast to stop seizures and protect the brain. Doctors use medicines and supportive care to help.
Long-term Monitoring and Treatment
Long-term care involves medication management and watching for seizures. Treatment plans are changed based on how the patient does. The goal is to reduce seizures and improve life quality.
Status Epilepticus Cases
Status epilepticus is a serious condition that needs quick medical help. It’s when seizures last a long time or keep happening without breaks. Fast treatment is vital to avoid lasting brain damage.
Brain and Spinal Tumor Patients
Patients with brain and spinal tumors face complex challenges. They need a detailed care plan from start to finish. This plan covers diagnosis, treatment, and recovery.
Pre-operative Care
Before surgery, patients get thorough checks and prep. This includes imaging studies like MRI and CT scans. These help find the tumor’s size and location.
Post-operative Recovery
After surgery, watching for complications and pain is key. Patients stay in the ICU. This is to catch any signs of brain issues or other problems.
Ongoing Treatment Protocols
Treatment might include radiation therapy, chemotherapy, or both. The plan is made just for the patient and the tumor’s type.
Awake Craniotomy Patients
Awake craniotomy is a special surgery for tumors close to important brain areas. Patients stay awake during part of the surgery. This helps surgeons avoid harming key brain functions.
| Treatment Aspect | Description | Considerations |
| Pre-operative | Neurological assessment and imaging | Accurate diagnosis and surgical planning |
| Post-operative | Monitoring for complications and pain management | ICU care for close observation |
| Ongoing Treatment | Radiation, chemotherapy, or combined therapy | Tailored to tumor type and patient needs |
Neurodegenerative Disease Patients
Neurodegenerative diseases are a big challenge in healthcare, affecting millions globally. These diseases cause neurons to break down, leading to loss of brain and body functions. Patients need special care to manage their symptoms and live better lives.
Alzheimer’s Disease
Alzheimer’s is the main cause of dementia in older adults, making up 60-80% of cases. It affects memory, thinking, and behavior. Treatment includes medications, cognitive training, and family support.
Parkinson’s Disease
Parkinson’s mainly affects movement, causing tremors, stiffness, and slow movement. Treatment includes dopamine therapy and other therapies to help with movement and mobility.
Multiple Sclerosis
Multiple sclerosis is an autoimmune disease that harms the central nervous system. It causes many neurological symptoms. Care focuses on managing relapses, slowing disease progress, and treating symptoms like fatigue and mobility issues.
ALS and Other Motor Neuron Diseases
Amyotrophic lateral sclerosis (ALS) quickly damages nerve cells that control muscles. Care for ALS patients aims to manage symptoms, keep function, and offer respiratory support as needed.
In summary, patients with neurodegenerative diseases need a detailed care plan. This plan addresses their medical, physical, and emotional needs. Understanding each disease’s unique challenges helps healthcare providers offer better care.
Neuro Unit Patients with Infectious Diseases
Neuroinfectious diseases are tough for healthcare providers. They need quick diagnosis and treatment to avoid lasting brain damage.
Meningitis and Encephalitis
Meningitis and encephalitis are serious infections of the brain and spinal cord. Meningitis causes inflammation of the brain’s protective membranes. Encephalitis is inflammation of the brain tissue itself. Both can cause severe problems if not treated quickly.
Brain Abscesses
A brain abscess is a pocket of pus in the brain, often from a bacterial or fungal infection. Symptoms include headache, fever, and neurological problems. Treatment usually involves antibiotics and sometimes surgery.
Post-Infectious Neurological Complications
Some people get neurological problems after an infection. These can include Guillain-Barré Syndrome or transverse myelitis.
Isolation Protocols for Neuroinfectious Diseases
To stop infectious diseases from spreading, neuro units have strict rules. These include wearing PPE, using isolation rooms, and cleaning more often.
Neurovascular Condition Patients
Patients with neurovascular diseases face complex challenges. These conditions affect the blood vessels in the brain and spinal cord. They need detailed care plans.
Aneurysms and AVMs
Aneurysms and arteriovenous malformations (AVMs) are serious issues. Aneurysms are swollen blood vessels that can burst. This can cause bleeding. AVMs are abnormal blood vessel tangles that can also lead to bleeding or brain problems.
Carotid Artery Disease
Carotid artery disease narrows or blocks the carotid arteries. These arteries carry blood to the brain. If not treated, it can cause a stroke.
Post-Intervention Care
After treatments like coiling or clipping, patients need close watch. The goal is to prevent problems and help them heal.
Vasospasm Monitoring
Vasospasm is a risk after bleeding in the brain. It’s when blood vessels get too narrow. Watching for vasospasm is key to avoid brain damage.
Handling neurovascular conditions well needs a team effort. Neurologists, neurosurgeons, and neuroradiologists work together. They aim to give the best care to these complex cases.
Coma and Altered Consciousness Patients
Caring for coma or altered consciousness patients is a big challenge in healthcare today. They need a detailed plan to manage their condition and help them recover.
Types of Altered Consciousness States
Altered consciousness can show up in different ways, like coma, vegetative state, and minimally conscious state. Each one needs its own care plan.
- Coma: A deep sleep where patients don’t react to anything around them.
- Vegetative State: Patients might have some basic reflexes but no thinking skills.
- Minimally Conscious State: Patients might show some awareness but can’t really interact.
Care Approaches for Minimally Conscious Patients
Helping minimally conscious patients involves many strategies. This includes checking their brain health, making sure they move right, and supporting their thinking.
| Care Approach | Description |
| Neurological Assessment | Regular checks on brain health to adjust care plans. |
| Mobility and Positioning | Special care to avoid problems like bed sores. |
| Cognitive Support | Ways to help with thinking and talking. |
Ethical Considerations in Prolonged Unconsciousness
Dealing with long-term unconsciousness brings up tough ethical questions. Decisions about keeping patients alive and their quality of life are very important. Healthcare workers must handle these with care and respect for everyone involved.
The Specialized Care Needs of Neuro Unit Patients
Neuro unit patients need care that is both precise and caring. Their conditions are complex, requiring a detailed treatment plan. This plan must be tailored to each patient’s needs.
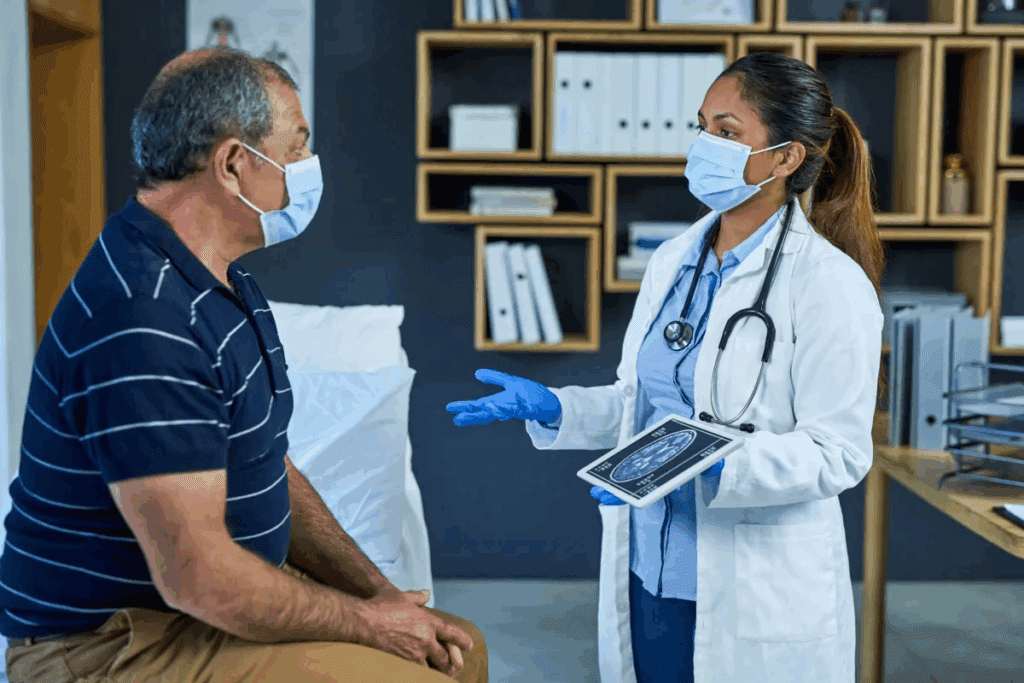
Neurological Assessment Protocols
Regular neurological checks are key for these patients. These checks track how their condition changes and if treatments work. Neurological assessment protocols look at consciousness, eye response, movement, and feeling.
Tools like the Glasgow Coma Scale (GCS) and the National Institutes of Health Stroke Scale (NIHSS) are used. They help doctors understand a patient’s status and make better decisions.
Mobility and Positioning Requirements
Moving patients right and keeping them in good positions is vital. It prevents issues like bed sores and blood clots. Regular changes in position and exercises help keep muscles flexible.
For those who can’t move much, special beds or therapy tables are helpful. They help avoid skin problems and improve blood flow.
Cognitive and Communication Support
Helping patients with thinking and talking is important. Many face challenges like memory loss after brain injuries.
Speech therapists are key in treating these issues. They teach patients new ways to communicate, improving their life and care involvement.
Swallowing and Nutritional Considerations
Many neuro unit patients struggle with swallowing, often due to stroke or brainstem issues. Swallowing assessments help find those at risk and plan their meals.
| Nutritional Consideration | Importance | Intervention |
| Adequate Caloric Intake | Supports healing and recovery | Tailored nutritional plans |
| Hydration | Prevents dehydration and promotes circulation | Monitoring fluid intake |
| Nutritional Supplements | Enhances nutritional status | Oral or enteral supplements |
Good nutrition is key for neuro unit patients’ recovery. A team of dietitians, speech therapists, and doctors works together. They ensure patients get the nutrients they need.
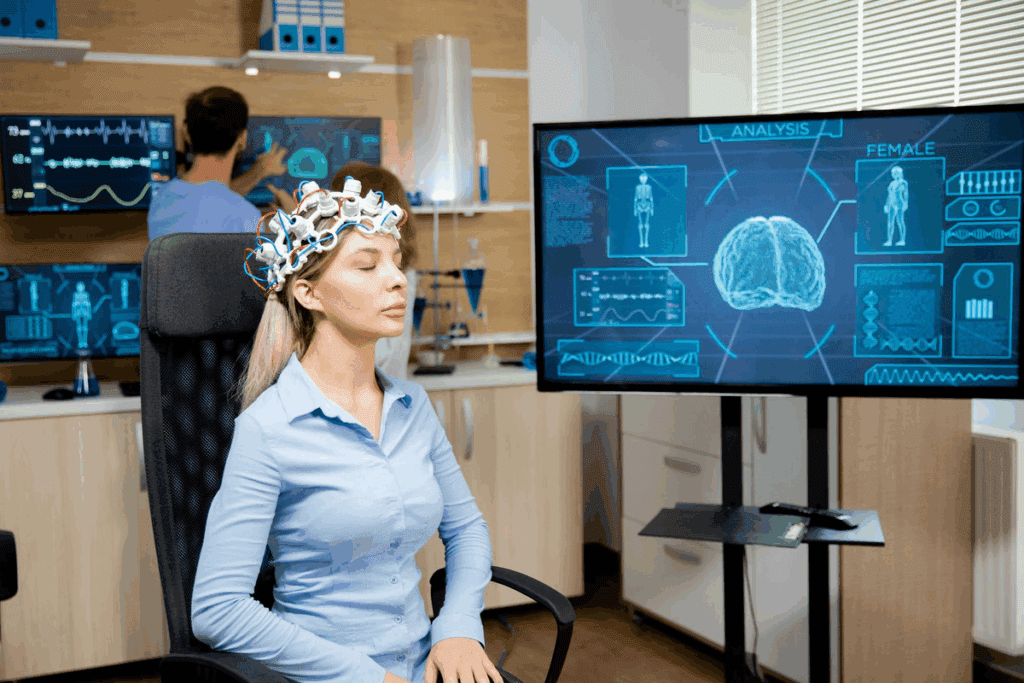
Advanced Technologies in Neuro Unit Care
Advanced technologies are key in improving patient care in neuro units. They bring new ways to treat neurological conditions. This has made care better for patients.
Neuromonitoring Equipment
Neuromonitoring tools are essential in neuro units. They help keep track of patients’ brain health. Tools like intracranial pressure monitors and EEG machines are used.
These tools help doctors make better decisions for their patients.
| Device | Purpose | Benefits |
| Intracranial Pressure Monitors | Monitor pressure inside the skull | Helps in managing patients with traumatic brain injuries |
| EEG Machines | Record electrical activity in the brain | Aids in diagnosing and managing seizure disorders |
| Cerebral Oximeters | Measure oxygen saturation in the brain | Assists in optimizing cerebral perfusion |
Robotic Rehabilitation Tools
Robotic tools are used in neuro units to help patients recover. They help patients regain motor skills and improve mobility.
Examples include: robotic exoskeletons and automated therapy devices. These tools offer personalized therapy, making recovery better.
Telemedicine in Neurological Care
Telemedicine is a big help in neurological care. It allows for remote consultations and monitoring. It’s great for patients in remote areas or those who can’t move easily.
Brain-Computer Interfaces
Brain-computer interfaces (BCIs) are a new technology. They let patients control devices with their thoughts. BCIs could greatly improve life for those with severe brain injuries.
These advanced technologies are changing neurology. They offer new hope and better care for patients.
Challenges and Experiences of Neuro Unit Patients
Patients in neuro units face many challenges. These go beyond their medical issues, affecting their body and mind. Their journey through neurological care is complex and involves many aspects.
Physical and Emotional Impact
Neurological conditions can deeply affect a person’s body. They can change how someone moves, feels, and thinks. Emotional distress is also a big concern, as patients deal with the mental side of their illness.
Anxiety and depression are common among these patients. They need strong mental health support as part of their care.
Family Dynamics and Support Systems
Family support is key for neuro unit patients. The emotional and practical help from family can greatly affect a patient’s recovery.
Navigating Recovery and Rehabilitation
Recovery for neuro unit patients involves many steps. It includes physical, occupational, and speech therapy. The journey is long and needs a well-planned care approach.
Patient Stories and Perspectives
Patient stories show the unique experiences in neuro units. These stories give insight into the challenges and the strength of patients.Conclusion: The Future of Neurological Patient Care
The world of neurological care is changing fast. This is thanks to new tech, research, and care that puts patients first. We see that new ways to care for the brain will help patients with tough conditions a lot.
New trends like artificial intelligence, robotics, and telemedicine are changing how we care for patients. These tools make care better, more available, and tailored to each person. For example, brain-computer interfaces and robotic tools help patients with brain and spinal cord injuries get better faster.
As care for the brain keeps evolving, doctors and nurses need to keep up. By using these new tools and focusing on the patient, we can make a big difference. This way, we can help those with brain conditions and shape the future of care.
FAQ
What is a neuro unit, and what kind of patients are treated there?
A neuro unit, or neurological intensive care unit, is a special part of a hospital. It cares for patients with severe brain problems. These include stroke, brain injury, spinal cord injury, and seizures.
What are the most common types of neurological conditions treated in a neuro unit?
In a neuro unit, common conditions are stroke, brain injury, spinal cord injury, and seizures. Also, brain tumors and diseases like Alzheimer’s and Parkinson’s are treated.
How are patients with traumatic brain injury classified, and what are their recovery expectations?
Patients with brain injury are sorted by how severe it is. Recovery hopes vary. Some might fully recover, while others face lasting brain, emotional, and physical issues.
What is the typical recovery timeline for stroke patients, and what rehabilitation needs do they have?
Stroke recovery times differ based on the stroke’s severity and the patient’s health. They often need physical, occupational, and speech therapy. This helps them regain lost skills and adapt to any lasting effects.
How are patients with spinal cord injuries treated and rehabilitated in a neuro unit?
Patients with spinal cord injuries get full care, from acute treatment to ongoing support. They might do physical and occupational therapy. They also learn about managing their condition.
What is status epilepticus, and how is it treated in a neuro unit?
Status epilepticus is a serious condition with long or repeated seizures. In a neuro unit, it’s treated with medicines, airway and breathing management, and finding the cause of the seizures.
What kind of care do patients with brain and spinal tumors receive in a neuro unit?
Patients with brain and spinal tumors get special care. This includes pre- and post-surgery care, and treatments like chemotherapy and radiation. Some may have awake craniotomy procedures.
How are patients with neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, cared for in a neuro unit?
Patients with neurodegenerative diseases get supportive care. This includes managing symptoms, medicines, and education on managing their disease. The goal is to improve their quality of life and keep them functional.
What is the role of advanced technologies, such as neuromonitoring equipment and brain-computer interfaces, in neuro unit care?
Advanced technologies are key in neuro unit care. They help monitor patients closely, spot changes, and act quickly. Technologies like brain-computer interfaces help in rehabilitation and improving outcomes.
How do neuro units support the physical and emotional needs of patients and their families?
Neuro units offer full care for patients and their families. They provide education, emotional support, and connect families with resources. This helps with physical and emotional needs.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2817554