Last Updated on December 1, 2025 by Bilal Hasdemir
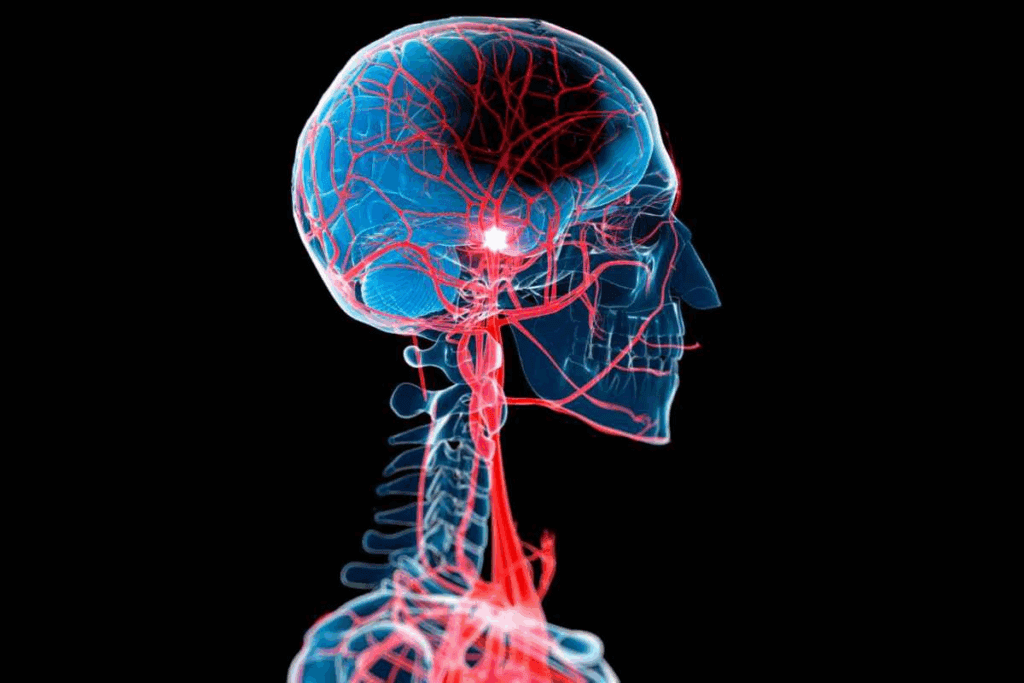
A cerebrovascular accident, or stroke, happens when the brain’s blood supply stops. This can be due to a blockage or a blood vessel rupture. Recent data shows a worrying trend: more young people are having strokes.Wondering why are young people having strokes? We explore the surprising root causes of cerebrovascular accidents in younger patients.
Understanding the causes of strokes is crucial for prevention and timely treatment. This knowledge helps prevent them and get treatment quickly. Stroke symptoms can be different but often include sudden weakness, confusion, or trouble speaking.
Spotting these symptoms early and getting stroke treatment fast can greatly improve recovery chances.
Key Takeaways
- Stroke incidence is rising among young adults.
- Understanding stroke causes is key to prevention.
- Recognizing stroke symptoms early is critical.
- Timely stroke treatment improves outcomes.
- Awareness and education can reduce stroke risk.
The Fundamentals of Cerebrovascular Accidents

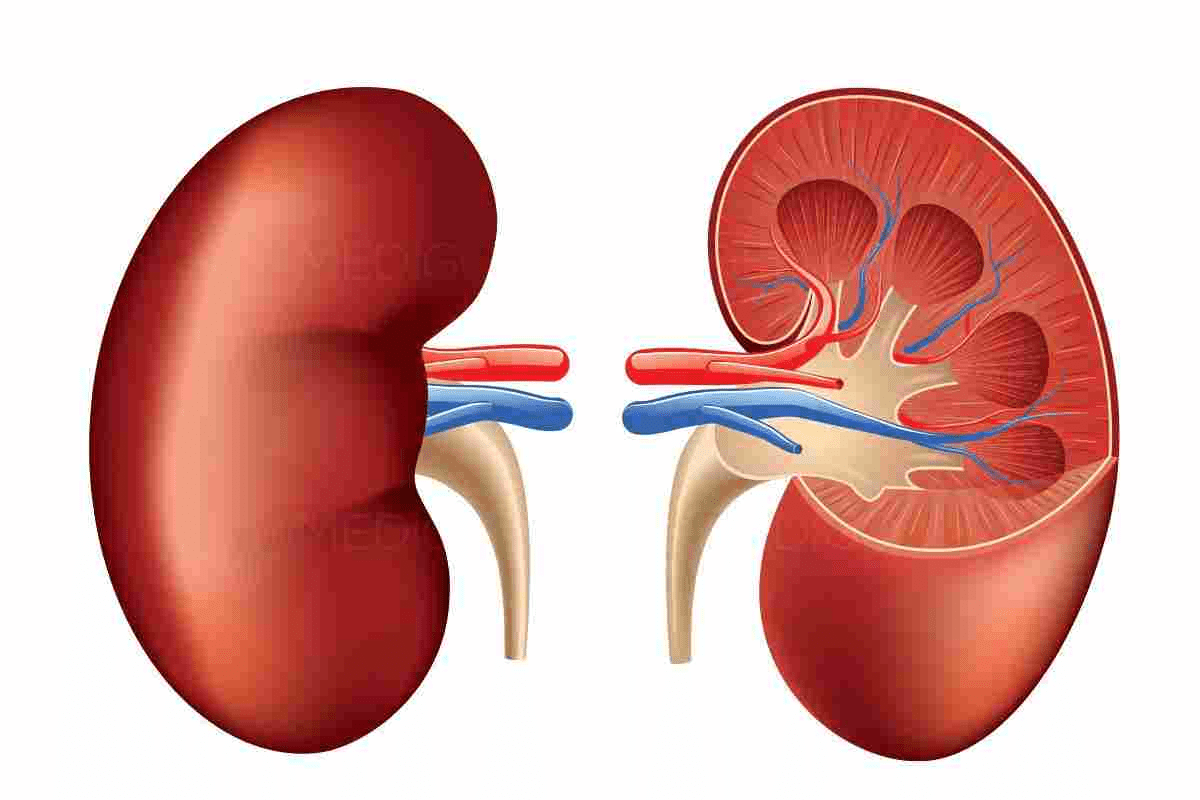
Exploring cerebrovascular accidents shows how strokes affect the brain. These accidents, or strokes, happen when blood flow to the brain stops or slows down. This prevents brain tissue from getting the oxygen and nutrients it needs.
Definition and Medical Terminology
A cerebrovascular accident is when brain function suddenly stops due to blood flow interruption. Terms like infarction and ischemia are used to describe brain tissue death and reduced blood flow, respectively.
Familiarity with these terms is essential for effective stroke treatment. Doctors use tools like CT and MRI scans to see how much damage there is. This helps them decide the best treatment.
How Strokes Affect the Brain
Strokes can deeply impact the brain, affecting thinking and movement. The damage’s location and severity determine the effects. For example, a stroke in the left hemisphere might mess with language, while a stroke in the right hemisphere could affect spatial skills and movement.
The brain’s anatomical structure is complex, with each area handling different tasks. Damage from a CVA can lead to symptoms like paralysis, speech problems, and thinking issues.
Types of Cerebrovascular Accidents
Understanding the causes of strokes is crucial for prevention and timely treatment.types of cerebrovascular accidents. These are also known as strokes. They can be divided into three main types: ischemic strokes, hemorrhagic strokes, and transient ischemic attacks. Each type has its own causes, symptoms, and treatment needs.
Ischemic Strokes: Blood Clots and Blockages
Ischemic strokes happen when a blood vessel in the brain gets blocked. This is the most common type of stroke, making up about 87% of cases. The blockage is usually a blood clot that forms in a vessel or travels from elsewhere in the body.
Ischemic strokes can be either thrombotic or embolic. Quick treatment with thrombolytic therapy can greatly improve outcomes for these patients.
Hemorrhagic Strokes: Bleeding in the Brain
Hemorrhagic strokes are caused by bleeding in or around the brain. This happens when a weak blood vessel bursts, causing bleeding in the brain. These strokes are less common but can be more severe.
They can be either intracerebral hemorrhage or subarachnoid hemorrhage. Because of their severity, hemorrhagic strokes need immediate medical care to stop the bleeding and prevent more damage.
Transient Ischemic Attacks: Warning Signs
Transient ischemic attacks (TIAs), or “mini-strokes,” are short periods of stroke-like symptoms. They don’t cause permanent damage, lasting only a few minutes. But, they are a warning sign of a future stroke.
Recognizing the signs of a TIA can help prevent a full stroke. Symptoms include sudden weakness or numbness, trouble speaking or understanding, vision changes, dizziness, or loss of balance.
Anatomical Understanding of Stroke Locations
Knowing how the brain is structured helps us understand how strokes affect it. Strokes can happen in different spots, each with its own effects on the body and brain.
Cerebral Hemispheres and Their Functions
The brain’s biggest part is the cerebral hemispheres, split into left and right halves. Each half controls the opposite side of the body and handles different tasks. The left hemisphere deals with language, logic, and analysis. On the other hand, the right hemisphere is key for spatial skills, intuition, and creativity.
Strokes in these hemispheres can cause various symptoms. For example, a left hemisphere stroke might make speaking hard. A right hemisphere stroke could lead to trouble with spatial awareness.
Brainstem and Cerebellum Strokes
The brainstem links the cerebrum to the spinal cord. It controls vital functions like breathing and heart rate. Strokes here can be very dangerous. Symptoms might include swallowing trouble, dizziness, and coordination loss.
The cerebellum is at the brain’s back. It helps with movement and posture. A stroke here can cause coordination loss, speech troubles, and odd eye movements.
Basal Ganglia and Corona Radiata Infarcts
The basal ganglia are deep in the brain. They’re important for movement and thinking. Strokes here can cause Parkinson’s-like symptoms and thinking problems.
The corona radiata is a white matter area with important tracts. Strokes here can cause weakness or paralysis, depending on the tracts affected.
Knowing where a stroke happens is key for understanding its effects and treatment. Each brain area has unique roles. Damage can lead to many different problems with thinking, moving, and sensing.
Traditional Risk Factors for Cerebrovascular Accidents
Understanding the causes of strokes is crucial for prevention and timely treatment. factors for cerebrovascular accidents. These are often called strokes. They happen when the brain’s blood supply is cut off, either by blockage or vessel rupture.
Age and Gender Considerations
Age is a big risk factor for stroke, with most happening over 55. The risk doubles every decade after 55. While age can’t be changed, knowing it helps manage other risks. Gender also matters, with men at higher risk before menopause. Women’s risk goes up after menopause.
Hypertension and Cardiovascular Disease
Hypertension, or high blood pressure, is the top cause of stroke. It can make brain blood vessels burst or narrow arteries. Cardiovascular disease, like atrial fibrillation, also raises stroke risk.
Diabetes and Metabolic Disorders
Diabetes is a big risk for stroke, damaging blood vessels and nerves. Metabolic syndrome, with high blood pressure and sugar, also increases stroke risk. Managing these with lifestyle and treatment can lower stroke risk.
In summary, knowing and managing risks like age, gender, hypertension, and diabetes is key. By tackling these, people can lower their stroke risk.
Why Are Young People Having Strokes?
Young-onset strokes are a growing concern that needs urgent attention. The rise in cerebrovascular accidents among the young is a major public health issue.
Alarming Statistics on Young-Onset Strokes
Recent studies show a worrying trend in strokes among the young.
| Age Group | Stroke Incidence Rate (per 100,000) | Percentage Change |
| 18-34 | 10.2 | +15% |
| 35-44 | 25.5 | +20% |
| 45-54 | 50.1 | +12% |
The data shows a worrying increase in strokes across different age groups. The biggest jump was in the 35-44 age group.
Unique Risk Factors in Younger Populations
Young stroke patients often face different risks than older ones. Substance abuse, like recreational drugs and too much alcohol, is a big risk factor.
- Substance abuse
- Smoking and tobacco use
- Obesity and physical inactivity
- Genetic predispositions
Understanding these unique risks is vital for developing effective prevention strategies.
Modern Lifestyle Factors Contributing to Early-Onset Strokes
Strokes are becoming more common among younger people. Examining the impact of lifestyle choices on stroke risk is essential. Things like diet, exercise, substance use, and stress levels play a big role in early-onset strokes.
Diet, Obesity, and Metabolic Syndrome
Eating too much processed food, saturated fats, and sugars can lead to obesity and metabolic syndrome. This increases stroke risk. Eating more fruits, vegetables, and whole grains can help. Also, managing weight through diet and exercise is key.
- Eating too much sodium can cause high blood pressure, a big stroke risk.
- Being overweight is linked to diabetes and high blood pressure.
- Metabolic syndrome, a group of conditions, raises the risk of heart disease and stroke.
Sedentary Behavior and Physical Inactivity
Being inactive is a big risk for stroke. Regular exercise keeps the heart healthy, lowers blood pressure, and boosts overall health. Adults should do at least 150 minutes of moderate or 75 minutes of vigorous exercise weekly.
- Regular exercise can lower stroke risk by improving heart health.
- Being inactive is linked to obesity, diabetes, and high blood pressure.
- Adding physical activity to daily life, like walking or cycling, can greatly reduce stroke risk.
Substance Use: Alcohol, Tobacco, and Recreational Drugs
Drinking alcohol, smoking, and using recreational drugs can increase stroke risk. It’s important to avoid or limit these substances to prevent strokes. Smoking harms blood vessels, raises blood pressure, and cuts off brain blood flow, all stroke risk factors.
- Drinking too much alcohol can cause high blood pressure, heart disease, and stroke.
- Smoking is a big risk for stroke because it damages the heart and blood vessels.
- Recreational drug use can harm heart health and increase stroke risk.
Chronic Stress and Sleep Deprivation
Chronic stress and not getting enough sleep are becoming major stroke risks. Managing stress and getting enough sleep are key to heart health. Chronic stress can cause high blood pressure and heart disease. Not sleeping well can affect blood pressure and overall health.
- Chronic stress can lead to high blood pressure and heart disease.
- Not sleeping enough increases stroke and heart disease risk.
- Using stress management techniques like meditation or yoga can lower stroke risk.
Genetic and Congenital Factors in Young Stroke Patients
Understanding the causes of strokes is crucial for prevention and timely treatment.th defects can lead to strokes in the young. While we know about high blood pressure and diabetes, genetics and birth defects also matter a lot.
Hereditary Conditions Affecting Blood Vessels
Some genetic conditions can harm blood vessels, raising stroke risk. For example, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) damages small brain blood vessels. This leads to strokes and dementia.
Hereditary hemorrhagic telangiectasia (HHT), or Osler-Weber-Rendu syndrome, causes AVMs. These can lead to bleeding strokes.
Congenital Heart Defects
Congenital heart defects are heart problems at birth. They can raise stroke risk due to abnormal blood flow. For instance, patent foramen ovale (PFO) or atrial septal defects (ASD) can let blood clots go straight to the body. This can cause a stroke.
Blood Clotting Disorders
Blood clotting disorders, or thrombophilias, increase ischemic stroke risk. Conditions like factor V Leiden and prothrombin G20210A mutation make blood clot more easily. This can lead to strokes.
| Condition | Description | Stroke Risk |
| CADASIL | Genetic disorder affecting small blood vessels in the brain | High risk of subcortical strokes |
| HHT | Formation of arteriovenous malformations (AVMs) | Increased risk of hemorrhagic strokes |
| PFO/ASD | Congenital heart defects allowing blood clots to bypass lungs | Increased risk of ischemic strokes |
| Factor V Leiden | Genetic disorder affecting blood clotting | Increased risk of ischemic strokes |
Understanding these unique risks is vital for developing effective prevention strategies.
Recognizing Stroke Symptoms: The Critical First Step
Familiarity with these terms is essential for effective stroke treatment.
The FAST Method for Stroke Identification
The FAST method is a well-known way to spot stroke symptoms. FAST stands for Face, Arm, Speech, and Time.
- Face: Ask the person to smile. Does one side of their face droop?
- Arm: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple sentence. Is their speech slurred or hard to understand?
- Time: Time is of the essence. If the person shows any of these symptoms, call for emergency services right away.
Beyond FAST: Additional Warning Signs
While the FAST method is great for spotting many symptoms, there are more signs to watch for. These include:
- Sudden numbness or weakness in the face, arm, or leg, on one side of the body
- Sudden confusion, trouble speaking, or trouble understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination
- Severe headache with no known cause
Symptoms Specific to Different Stroke Types
Familiarity with these terms is essential for effective stroke treatment.
| Stroke Type | Common Symptoms |
| Ischemic Stroke | Sudden weakness, numbness, or paralysis in the face, arm, or leg; trouble speaking or understanding speech |
| Hemorrhagic Stroke | Severe headache, vomiting, altered consciousness, and sometimes seizures |
| Transient Ischemic Attack (TIA) | Temporary symptoms like ischemic stroke, often go away within 24 hours |
Spotting these symptoms and acting fast can greatly help stroke patients. It’s vital to know the warning signs and get medical help right away if you see any.
Why Strokes Are Often Misdiagnosed in Young People
Diagnosing strokes in young people is tricky. Younger folks are not seen as high-risk for strokes. This can cause delays or wrong diagnoses.
Atypical Presentation in Younger Patients
Young people often show different stroke symptoms. Unlike older adults, they might not have the usual signs like facial drooping or arm weakness. Instead, they might have headaches or seizures.
This makes it hard for doctors to diagnose. It’s important for doctors to know how strokes can show up differently in young people.
Healthcare Provider Bias: “Too Young for a Stroke”
Doctors sometimes think young people can’t get strokes. This thinking can make them miss the signs in this age group.
Research shows young patients are often misdiagnosed in emergency rooms. This delay can make their condition worse.
It’s key to recognize that young people can have strokes too.
When to Advocate for Emergency Care
If you or someone you know has stroke symptoms, get help right away. Use the FAST method to check for symptoms: Facial drooping, Arm weakness, Speech issues, and Time to call for help.
Other signs like sudden vision changes or severe headaches also need quick medical checks.
Don’t wait to get emergency care if you’re unsure. It’s safer to be cautious with stroke symptoms.
Diagnostic Procedures for Cerebrovascular Accidents
Diagnosing a stroke requires a mix of clinical checks, imaging, and lab tests. It’s key to get the diagnosis right and fast. This helps in treating and managing strokes well.
Imaging Techniques: CT, MRI, and Angiography
Imaging is a big help in finding out about strokes. It shows where and how big the stroke is. The main imaging tools are:
- Computed Tomography (CT): It quickly spots bleeding and decides if urgent action is needed.
- Magnetic Resonance Imaging (MRI): It gives detailed views of the brain. This helps find ischemic strokes and see how much damage there is.
- Angiography: It looks at the blood vessels. It finds blockages or odd shapes like aneurysms.
Laboratory Tests for Stroke Evaluation
Lab tests are key to finding out why a stroke happened and the patient’s health. These tests might include:
- Blood glucose tests
- Lipid profiles
- Coagulation studies
- Complete blood count (CBC)
Comprehensive Neurological Examinations
A thorough neurological check looks at the patient’s brain health. It finds problems and helps decide on treatment. This check looks at:
| Examination Component | Description |
| Mental Status | Checks how awake, aware, and thinking the patient is. |
| Cranial Nerves | Looks at how well nerves like vision and hearing are working. |
| Motor and Sensory Function | Checks muscle strength and feeling. |
| Coordination and Balance | Sees how well the brain controls movement and balance. |
By using all these methods, doctors can accurately find out about strokes. They can then make treatment plans that fit each patient’s needs.
Acute Treatment Approaches for Stroke
Acute stroke treatment has changed a lot. It now focuses on quick action to save lives and brain function. The main goal is to get blood flowing again to the brain’s affected areas. This helps reduce damage.
Time-Critical Interventions: The Golden Hour
The first hours after a stroke are very important. Quick medical help can greatly improve results. The “golden hour” idea shows how fast action is key.
- Rapid assessment and diagnosis
- Immediate imaging studies (CT or MRI)
- Activation of stroke protocols
Doctors must quickly check the patient and decide the best treatment. This time is critical for giving urgent treatments.
Medication Options: Thrombolytics and Anticoagulants
Medicines are very important in treating strokes. Thrombolytics, like alteplase, break up clots in ischemic strokes. Anticoagulants, such as heparin or Plavix (clopidogrel), stop new clots and prevent big ones.
Key medication considerations:
- Thrombolytics must be given within 4.5 hours of symptoms starting
- Anticoagulants prevent more clotting
- Choosing the right patient is key to avoid risks
The role of Plavix as an antiplatelet drug is important. Plavix drug classification shows it stops platelets from sticking together.
Endovascular and Surgical Procedures
Along with medicines, endovascular and surgical methods are vital for some strokes. These methods help get blood flowing again and lower brain damage risk.
| Procedure | Description | Indications |
| Mechanical Thrombectomy | Removal of a blood clot from the cerebral arteries | Large vessel occlusion strokes |
| Angioplasty and Stenting | Opening narrowed arteries and placing a stent | Severe stenosis or occlusion |
| Surgical Clipping or Coiling | Treating aneurysms or arteriovenous malformations | Hemorrhagic strokes due to aneurysms or AVMs |
These complex procedures need a lot of skill. They are usually done in specialized stroke centers.
Rehabilitation and Recovery After Stroke
The journey to recovery after a stroke is complex. It involves many steps to help regain lost abilities. Each person’s needs are unique, and rehabilitation is key to adapting to changes.
Physical and Occupational Therapy
Physical therapy helps patients regain strength and mobility. Occupational therapy focuses on daily activities and tasks.
- Physical therapists work on improving balance and coordination.
- Occupational therapists help patients relearn skills such as dressing and cooking.
Speech and Language Rehabilitation
Speech and language therapy is vital for those struggling with communication after a stroke. It helps patients speak clearly and understand language better.
Key aspects of speech and language rehabilitation include:
- Improving articulation and pronunciation.
- Enhancing comprehension and expression of language.
Cognitive Rehabilitation Strategies
Cognitive rehabilitation helps patients recover from stroke-related cognitive impairments. It includes memory training, attention exercises, and problem-solving activities.
Cognitive rehabilitation can significantly improve a patient’s quality of life by enabling them to perform daily tasks independently.
Emotional and Psychological Support
Emotional and psychological support are essential in stroke rehabilitation. Patients often need counseling or therapy to deal with emotional challenges.
- Support groups can provide a sense of community and understanding.
- Counseling can help patients manage feelings of anxiety or depression.
Rehabilitation after a stroke is a detailed process. It addresses physical, cognitive, and emotional needs. By using various therapies and support systems, individuals can make significant progress and enhance their quality of life.
Comprehensive Prevention Strategies for Young Adults
Teaching young adults about stroke prevention is vital. It helps lower the number of strokes. By knowing and using prevention strategies, young adults can greatly reduce their stroke risk.
Regular Health Screenings and Risk Assessments
Regular health checks are key to spotting stroke risks. These include blood pressure, cholesterol, and diabetes tests. Early detection lets young adults manage their health better.
Risk assessments look at family history, lifestyle, and health signs. They give a full picture of stroke risk.
Lifestyle Modifications for Stroke Prevention
Changing your lifestyle is important for preventing strokes. Eating a healthy diet with lots of fruits and veggies is a must. Also, aim for at least 150 minutes of physical activity weekly.
- Maintaining a healthy weight
- Avoiding smoking and limiting alcohol
- Managing stress with mindfulness or therapy
Managing Medical Conditions That Increase Risk
For young adults with health issues like high blood pressure or diabetes, managing them is key. Stick to your meds, see your doctor often, and make lifestyle changes.
By being proactive and informed about health, young adults can lower their stroke risk. This helps them stay healthy overall.
Emerging Research on Young-Onset Strokes
New research on young-onset strokes is growing our understanding. It’s also bringing new hope for treatments and prevention. Recent studies have uncovered the complex factors behind strokes in younger people.
New Understanding of Underlying Mechanisms
Researchers are learning more about what causes young-onset strokes. They’re looking at genetic predispositions, environmental factors, and lifestyle choices. For example, some genetic conditions can greatly raise a young person’s stroke risk.
Research into stress granules and cell death in diseases like stroke is exciting. It could lead to new treatments.
Innovative Treatment Approaches for Young Patients
New treatments are being made for young stroke patients. These include advanced thrombolytic therapies and endovascular procedures. They aim to cut down recovery time and improve results.
Stem cell therapy and rehabilitation technologies are also being explored. They might help young stroke survivors recover faster and avoid long-term disabilities.
Predictive Models and Prevention Strategies
Creating predictive models is key to spotting high-risk individuals for young-onset strokes. By looking at risk factors and genetic markers, doctors can focus on prevention.
Prevention plans are being made for young people. They include lifestyle changes and managing health conditions. Public health efforts aim to teach young adults about stroke risks and the need for a healthy lifestyle.
Conclusion
Cerebrovascular accidents, or strokes, are a big health issue. They affect both the elderly and the young. Understanding the causes of strokes is crucial for prevention and timely treatment.tors, and symptoms to catch them early.
We talked about the different types of strokes and how they harm the brain. We also discussed the warning signs and symptoms. These can change based on the type of stroke.
A stroke happens when blood flow to the brain stops. This can be due to a blockage or a burst blood vessel. This stop can damage or kill brain cells, leading to loss of brain function. The increase in strokes among the young is a big concern.
Living a healthy lifestyle and managing health conditions can help prevent strokes. Young people need to take steps to prevent strokes. Healthcare providers must also be quick to diagnose and treat strokes in the young.
FAQ
What is a cerebrovascular accident (CVA)?
A cerebrovascular accident, or stroke, happens when the brain’s blood supply stops. This can be due to a blockage or a blood vessel rupture. It leads to brain cell damage or death.
What are the main types of strokes?
There are three main types of strokes. Ischemic strokes are caused by blood clots or blockages. Hemorrhagic strokes are due to bleeding in the brain. Transient ischemic attacks, or “mini-strokes,” are temporary.
What are the symptoms of a stroke?
Stroke symptoms include sudden weakness or numbness in the face, arm, or leg. You might have trouble speaking or understanding speech. Sudden vision changes, dizziness, or loss of balance are also signs.
The FAST method helps spot these symptoms: Face drooping, Arm weakness, Speech difficulties, and Time to call for emergency services.
Why are young people having strokes?
Young people are having more strokes due to lifestyle choices and genetics. Diet, lack of exercise, substance use, and stress play a role. These factors contribute to the rising number of strokes.
What are the traditional risk factors for stroke?
Traditional stroke risk factors include age, gender, and certain health conditions. Hypertension, cardiovascular disease, diabetes, and metabolic disorders increase stroke risk.
How can strokes be prevented?
Preventing strokes involves regular health screenings and lifestyle changes. Eating well and exercising regularly are key. Managing health conditions and avoiding substance use also help.
What is the importance of timely medical intervention in stroke treatment?
Timely medical help is vital in treating strokes. Quick action can reduce brain damage and improve outcomes. The first hour after a stroke is the most critical time for treatment.
What are the treatment options for stroke?
Stroke treatments include medications and endovascular procedures. Surgery may also be necessary. Rehabilitation helps regain lost functions and improve quality of life.
Can genetic factors contribute to stroke risk?
Yes, genetics can increase stroke risk. Conditions affecting blood vessels, congenital heart defects, and blood clotting disorders are examples. These can raise the chance of having a stroke.
How can young adults reduce their risk of having a stroke?
Young adults can lower their stroke risk by living a healthy lifestyle. This includes eating well, exercising regularly, not smoking, and managing stress. Regular health check-ups can also identify risk factors.
What is the role of rehabilitation after a stroke?
Rehabilitation is key in recovering from a stroke. It helps regain lost functions and adapt to changes. It includes physical, occupational, speech, and language therapy, as well as cognitive and emotional support.
References
National Center for Biotechnology Information. Stress association with cerebrovascular disease in United States. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6126243/