Last Updated on December 1, 2025 by Bilal Hasdemir
Brain vascular diseaseDid you know that cerebrovascular disease affects millions of people worldwide? It often leads to a stroke. While related, they are not the same. Cerebrovascular disease includes conditions like stroke, aneurysms, and carotid artery disease, all affecting blood flow to the brain.
A stroke occurs when the blood supply to the brain is interrupted.
Key Takeaways
- Cerebrovascular disease is a broad term that encompasses various conditions affecting blood flow to the brain.
- A stroke occurs when the blood supply to the brain is interrupted.
- Cerebrovascular disease includes conditions such as aneurysms and carotid artery disease.
- Understanding the differences between cerebrovascular disease and stroke is crucial for proper diagnosis and treatment.
- Cerebrovascular disease and stroke are closely related, and managing one can impact the other.
Understanding Cerebrovascular Disease and Stroke
To grasp the impact of stroke, it’s key to know about cerebrovascular disease (CVD). CVD is about conditions that harm the blood vessels leading to the brain. This can cut down oxygen and cause damage.
Cerebrovascular disease is a big health issue worldwide. It often leads to stroke, which is a top cause of illness and death.
Defining Key Medical Terms
Cerebrovascular disease covers many conditions that harm the brain’s blood vessels. The CVD definition includes any issue with the brain’s blood vessels. This can lead to less oxygen and brain damage.
A cerebral vascular disorder is another name for brain blood vessel problems. Knowing these terms helps doctors diagnose and treat better.
| Term | Definition |
| Cerebrovascular Disease (CVD) | Conditions affecting the blood vessels supplying the brain. |
| Stroke | A stroke occurs when the blood supply to the brain is interrupted. |
| Cerebral Vascular Disorder | Conditions affecting the blood vessels in the brain. |
The Relationship Between CVD and Stroke
The link between CVD and stroke is complex. CVD is a wide term that includes stroke and other conditions. Stroke vs CVD is a common debate, as stroke is often a sign of CVD.
A stroke occurs when the brain is deprived of oxygen and nutrients. This is because of blockages or ruptures in blood vessels. These problems are often caused by CVD.
Answering the Title Question
To answer the question, “Is cerebrovascular disease the same as a stroke?” – they are related but not the same. CVD is a wider term that includes many brain blood vessel conditions, including stroke.
A stroke occurs when the blood supply to the brain is interrupted.
Brain Vascular Disease: An Overview
Brain vascular disease includes many conditions that harm the brain’s blood vessels. These can greatly reduce a person’s quality of life. In severe cases, they can cause stroke or other brain problems. It’s important to know about these diseases to prevent and treat them.
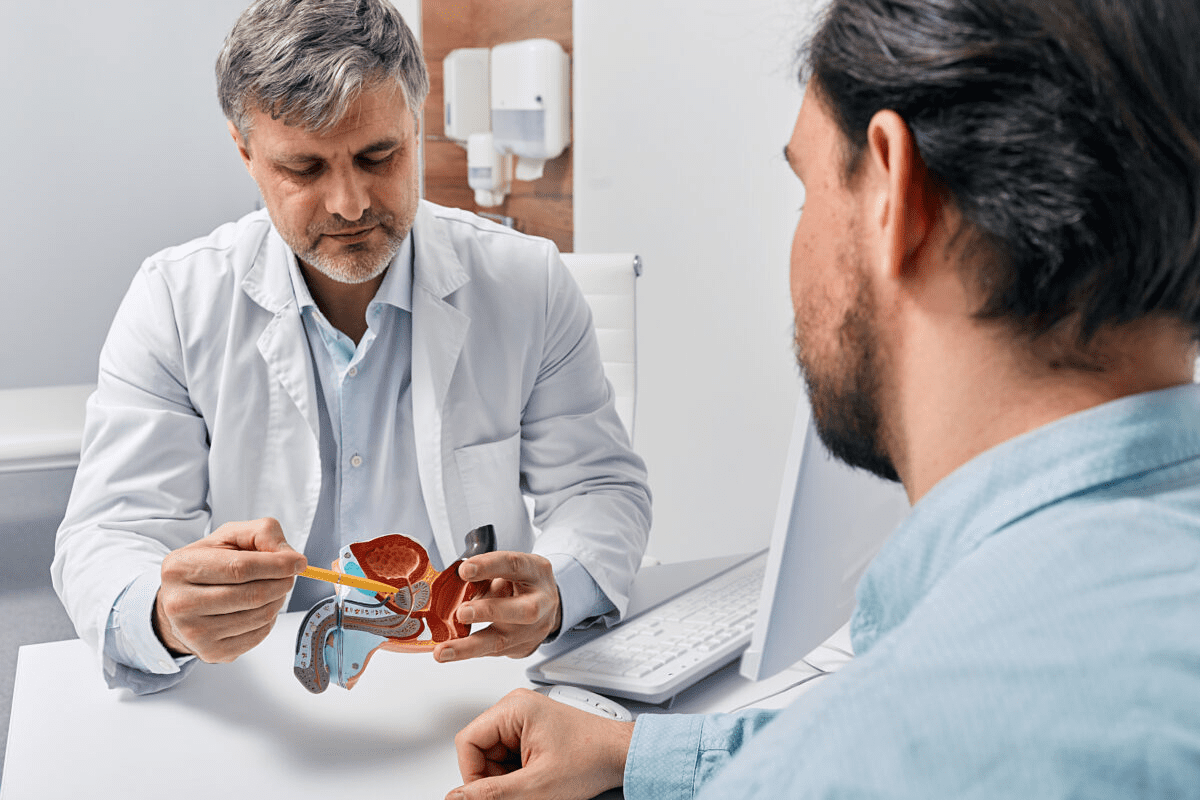
What Constitutes Cerebrovascular Disorders
Cerebrovascular disorders are a group of conditions that affect the brain’s blood supply. They include stenosis, or blood vessel narrowing, aneurysms, which are bulges, and vascular malformations, abnormal blood vessel formations. Each can reduce blood flow to the brain, leading to serious health problems.
Common Types of Brain Vascular Conditions
Some common brain vascular conditions are:
- Aneurysms: These are abnormal bulges in blood vessels that can rupture, leading to hemorrhagic stroke.
- Arteriovenous Malformations (AVMs): These are tangles of blood vessels that can disrupt normal blood flow.
- Stenosis: Narrowing of the blood vessels, often due to atherosclerosis, which can reduce blood flow to the brain.
These conditions show how complex brain vascular disease is. They highlight the need for detailed care.
The Cerebrovascular System Anatomy
A stroke occurs when the blood supply to the brain is interrupted.
Stroke as a Manifestation of Cerebrovascular Disease
A stroke occurs when the brain is deprived of oxygen and nutrients.
How Strokes Occur
Ischemic strokes occur when a blood clot or plaque blocks a brain blood vessel. This stops blood flow. Hemorrhagic strokes happen when a weak blood vessel bursts, bleeding into the brain.
Both types damage brain cells, leading to disability or death. Ischemic stroke is more common, making up 87% of all strokes. It’s often caused by a blood clot in the brain or elsewhere in the body.
Acute vs. Chronic Cerebrovascular Conditions
Cerebrovascular disease can be acute or chronic. Acute conditions, like stroke, need quick medical help because they can cause severe damage. Chronic conditions develop slowly and may not show symptoms right away.
Managing chronic cerebrovascular disease is key to prevent strokes. It’s important to control risk factors like high blood pressure, diabetes, and high cholesterol.
Stroke as a Medical Emergency
Stroke is a medical emergency that needs fast treatment. Quick care can greatly improve outcomes and reduce damage. Knowing the signs of stroke is vital for quick action.
Acting F.A.S.T. (Face, Arm, Speech, Time) can save lives. If you think someone is having a stroke, call emergency services right away.
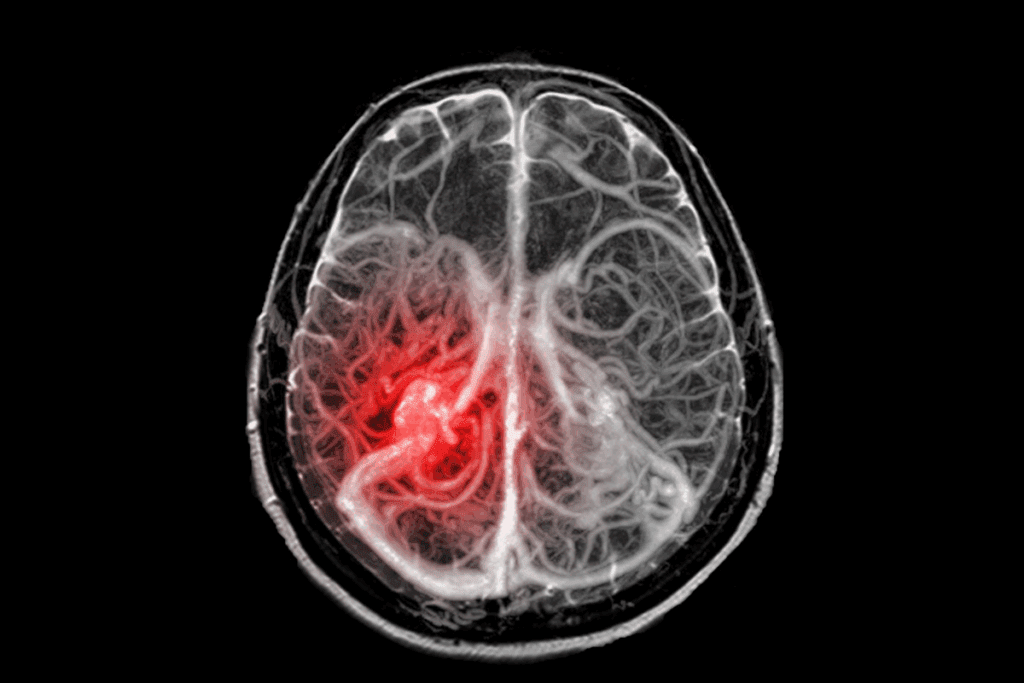
Ischemic Stroke: When Blood Flow Is Blocked
A stroke occurs when the blood supply to the brain is interrupted.
Mechanisms of Ischemic Stroke
Ischemic strokes happen when something blocks a blood vessel to the brain. This blockage is often a blood clot or atherosclerosis. Atherosclerosis is when plaque builds up in arteries, narrowing or blocking them.
This blockage stops brain tissue from getting oxygen and nutrients. It can cause damage or death to brain cells. The stroke’s impact depends on where and how much the blood flow is blocked, and for how long.
Subtypes of Ischemic Stroke
Ischemic strokes can be split into different types based on their cause. The main types are:
- Thrombotic Stroke: A blood clot forms in a brain vessel.
- Embolic Stroke: A clot or particle from elsewhere in the body blocks a brain vessel.
- Lacunar Stroke: Small arteries are blocked, often due to high blood pressure and diabetes.
Knowing these types helps doctors choose the best treatment for each stroke. This can lead to better results for patients.
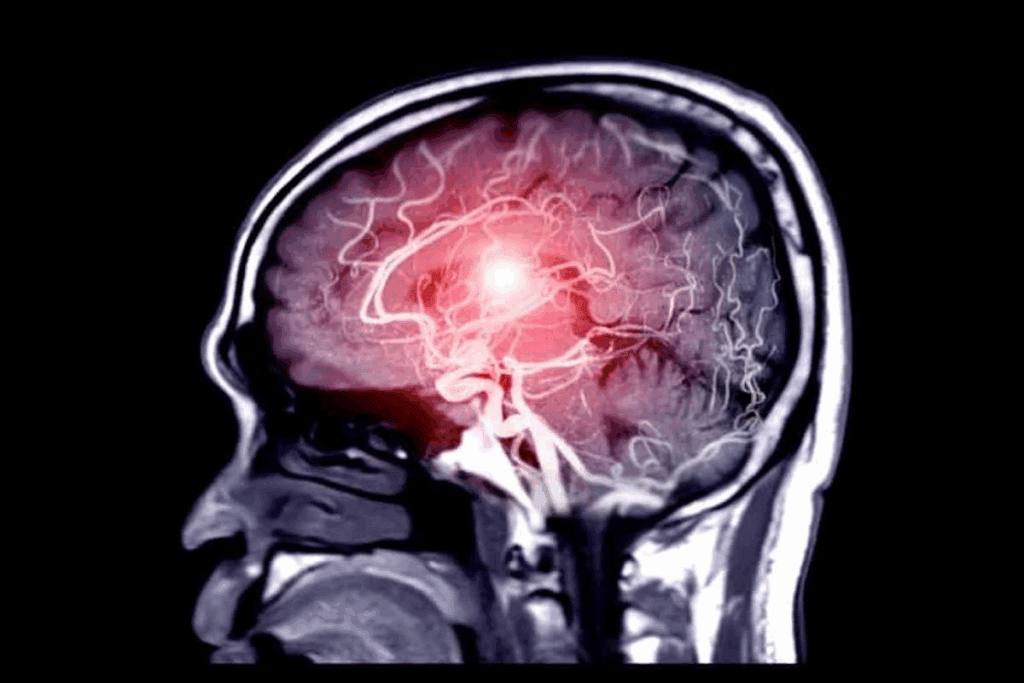
Hemorrhagic Stroke: When Blood Vessels Rupture
A stroke occurs when the brain is deprived of oxygen and nutrients.
Intracerebral Hemorrhage
Intracerebral hemorrhage is when a blood vessel in the brain bursts. This leads to bleeding into the brain tissue around it. It’s often linked to high blood pressure, vascular brain disorders, and anticoagulant use. Symptoms include sudden headache, nausea, vomiting, and decreased consciousness.
To diagnose, doctors use CT scans or MRI. Treatment aims to control blood pressure and manage brain pressure. Sometimes, surgery is needed to remove the blood clot or fix the cause.
Subarachnoid Hemorrhage
Subarachnoid hemorrhage is when bleeding happens in the space between the brain and its covering. It’s often due to an aneurysm rupture. Symptoms include a sudden, severe headache, nausea, vomiting, and sometimes loss of consciousness.
Diagnosis uses CT scans or lumbar puncture. Treatment involves fixing the aneurysm, managing brain swelling, and preventing more bleeding.
Comparing Hemorrhagic and Ischemic Strokes
Hemorrhagic strokes make up about 13% of all strokes but are more deadly than ischemic strokes. Ischemic strokes are caused by blood flow blockage, while hemorrhagic strokes are due to blood vessel rupture. Knowing the difference is key for stroke prevention cvd and treatment.
- Hemorrhagic Strokes: Caused by blood vessel rupture, often linked to high blood pressure and aneurysms.
- Ischemic Strokes: Caused by blood flow blockage, often due to blood clots and atherosclerosis.
Managing neurological vascular issues needs a full approach. This includes changing risk factors, quick diagnosis, and right treatment. By understanding hemorrhagic strokes, we can tackle these challenges better and improve patient care.
Transient Ischemic Attack: The “Mini-Stroke”
TIAs, or ‘mini-strokes,’ are brief disruptions in brain blood flow. They are important warning signs. If a TIA happens, it means there’s a temporary issue with the brain’s blood supply. This could lead to a more serious stroke. It’s key to understand TIAs to get medical help quickly and prevent future strokes.
TIA Symptoms and Duration
The symptoms of a TIA are similar to a stroke. They can include sudden weakness or numbness in the face, arm, or leg. Also, trouble speaking or understanding speech, sudden vision changes, dizziness, or loss of balance. These symptoms usually last from a few minutes to a few hours and go away within 24 hours.
Recognizing TIA symptoms quickly is very important. They show a higher risk of having a stroke. TIAs are not just minor events. They are warning signs that need immediate medical attention.
TIA as a Warning Sign
A TIA is a big warning sign that you might have a full-blown stroke. Studies show people who have a TIA are more likely to have a stroke within 90 days. The biggest risk is in the first 48 hours. So, a TIA means you need to see a doctor right away to prevent a stroke.
Getting medical help quickly after a TIA is crucial. If you think you’re having a TIA, go to the hospital right away. This way, doctors can check your risk factors and help lower them.
Diagnostic Criteria for TIAs
To diagnose a TIA, doctors do a detailed check-up. This includes a medical history, physical exam, and tests like MRI or CT scans. They also do vascular studies, like carotid ultrasound. The goal is to find out why the TIA happened and how likely you are to have another stroke.
Knowing how to diagnose TIAs is important for doctors. It helps them figure out how risky you are and what to do next. A complete check-up is key to finding the right treatment and preventing future strokes.
Cerebral Aneurysms and Vascular Malformations
Types of Brain Aneurysms
A brain aneurysm is a weak spot on a brain artery that balloons and fills with blood. There are different types, like saccular (berry) aneurysms and fusiform aneurysms. Saccular aneurysms are the most common and often found at artery branch points.
“Aneurysms can be silent for years,” says a top neurosurgeon. “It’s key to spot risk factors and watch people with a family history or other risk factors.”
Arteriovenous Malformations (AVMs)
Arteriovenous malformations (AVMs) are odd connections between arteries and veins in the brain. They can cause seizures, headaches, and brain problems. AVMs are usually born with us but can also happen after trauma or other issues.
AVMs are dangerous because they can burst, causing a hemorrhagic stroke. The chance of bursting depends on the size and where the AVM is.
Risk of Rupture and Stroke
Both aneurysms and AVMs can burst, leading to a hemorrhagic stroke. The risk depends on the size and location of the problem, plus the person’s health and medical history.
- Risk factors for aneurysm rupture include size, location, and family history.
- AVM rupture risk is influenced by size, location, and venous drainage patterns.
Knowing these risks helps us create good treatment plans and prevent strokes. We’ll look at new ways to diagnose and treat cerebrovascular disease next.
Vascular Dementia: Cognitive Decline from Poor Blood Flow
Vascular dementia is a growing health issue. It often comes from multiple strokes or small vessel disease. We will look at how it develops, its differences from Alzheimer’s, and its subtypes.
Development of Vascular Dementia
Vascular dementia happens when blood flow to the brain is reduced. This damages brain tissue and affects thinking. It can come from multiple strokes or small vessel disease.
Factors like high blood pressure, diabetes, and atherosclerosis increase the risk. Managing these is key to preventing vascular dementia.
Differences from Alzheimer’s Disease
Vascular dementia and Alzheimer’s both affect thinking, but in different ways. Alzheimer’s is caused by amyloid plaques and tau tangles. Vascular dementia is caused by poor blood flow.
Vascular dementia’s symptoms and progression are different. It often gets worse in steps after strokes. Alzheimer’s decline is more gradual.
Subtypes of Vascular Dementia
There are two main types of vascular dementia. Multi-infarct dementia comes from large strokes. Subcortical vascular dementia is from small vessel disease. It affects deeper brain areas, causing planning, decision-making, and memory problems.
| Subtype | Causes | Symptoms |
| Multi-infarct Dementia | Multiple large strokes | Significant cognitive decline, stepwise progression |
| Subcortical Vascular Dementia | Small vessel disease | Difficulties with planning, decision-making, memory |
Knowing the differences between these subtypes is crucial. It helps doctors create better treatment plans. This way, they can meet the unique needs of patients with vascular dementia.
Risk Factors for Cerebrovascular Disease
Several factors can increase your chance of getting cerebrovascular disease. These include genetics, lifestyle, and the environment. Knowing these risks is key to preventing and managing the disease.
Modifiable Risk Factors
Some risk factors can be changed through lifestyle or medicine. These include:
- Hypertension: High blood pressure can harm blood vessels in the brain.
- Diabetes: Diabetes can damage blood vessels and nerves, raising the risk.
- Smoking: Smoking harms the heart and raises blood pressure.
- High Cholesterol: High LDL cholesterol can clog arteries, increasing stroke risk.
- Obesity and Physical Inactivity: Being overweight or inactive can lead to other risks like high blood pressure and diabetes.
Changing these risk factors can lower your chance of cerebrovascular disease. This can be done by eating well, exercising, quitting smoking, and managing conditions like high blood pressure and diabetes.
Non-Modifiable Risk Factors
Some risk factors can’t be changed, but knowing them is still important. These include:
| Risk Factor | Description |
| Age | The risk of cerebrovascular disease goes up with age, especially over 55. |
| Family History | Having a family history of stroke or cerebrovascular disease raises your risk. |
| Genetic Predisposition | Some genetic conditions can make you more likely to get cerebrovascular disease. |
Knowing these non-modifiable risk factors helps us take steps to manage the ones we can change. It also helps healthcare providers keep a close eye on your health.
By tackling both modifiable and non-modifiable risk factors, we can lower the number of cases of cerebrovascular disease. This helps both individuals and communities.
Diagnosing Cerebrovascular Disorders
Healthcare professionals use many methods to diagnose cerebrovascular disorders. These include clinical evaluation, neurological examination, and diagnostic imaging. They aim to understand the extent of the disease and identify risk factors.
Clinical Evaluation and Neurological Examination
Diagnosing cerebrovascular disorders starts with a detailed medical history. They look at risk factors like hypertension and diabetes. A neurological examination checks for cognitive, motor, and sensory deficits.
The neurological examination is key. It helps pinpoint the lesion and assess its severity. Tools and techniques used include checking cranial nerve function, muscle strength, reflexes, and coordination.
Imaging Techniques
Imaging is crucial in diagnosing cerebrovascular disease. Computed Tomography (CT) scans quickly spot hemorrhagic strokes in emergencies. Magnetic Resonance Imaging (MRI) offers detailed brain tissue images, useful for ischemic strokes and other conditions.
- CT scans are great for acute hemorrhage detection.
- MRI is good at catching early brain tissue changes, spotting ischemic strokes.
- Angiography, including CT and MR angiography, shows blood vessel issues like aneurysms or stenosis.
Laboratory Tests and Biomarkers
Laboratory tests are vital for assessing risk factors and finding causes. They include blood glucose, lipid profiles, and inflammation markers. Biomarkers like troponin and D-dimer help gauge stroke and heart event risks.
Tests also monitor treatment effects and manage risk factors. For instance, regular blood pressure checks are key for hypertension patients, a major stroke risk factor.
Treatment Approaches for Cerebrovascular Disease
Treating cerebrovascular disease is complex. It involves emergency care, surgery, and rehab. Each step is crucial and must fit the person’s needs.
Acute Stroke Interventions
Quick action is key in treating strokes. Thrombolysis is a main treatment for ischemic strokes. It uses drugs to clear blood clots.
“Time is brain” in stroke care. This means getting help fast is vital.
“The sooner thrombolysis is administered after stroke onset, the better the outcomes for patients.”
Mechanical thrombectomy is another option. It removes the clot from the artery. This is for patients with big blockages.
Surgical Interventions
Surgery is key for some cerebrovascular issues. For example, clipping or coiling can stop aneurysms from bursting. Surgery can also help with moyamoya disease or severe carotid stenosis.
Rehabilitation After Stroke
Rehab is a big part of stroke care. It helps patients get back lost skills and adjust to changes. A team of therapists works together to support recovery.
Rehab plans are made just for each person. They focus on moving better, doing daily tasks, and improving thinking or speaking skills.
With a full treatment plan, we can greatly improve life for those with cerebrovascular disease. This includes quick care, surgery when needed, and thorough rehab.
Preventing Cerebrovascular Disease and Stroke
To stop cerebrovascular disease and stroke, knowing the risks and taking steps to prevent them is key. This disease harms the brain’s blood vessels, leading to a lot of illness and death globally.
Lifestyle Modifications
Making lifestyle changes is vital in preventing cerebrovascular disease. Regular physical activity, a balanced diet full of fruits, veggies, and whole grains, and keeping a healthy weight are essential. Also, quitting smoking and cutting down on alcohol can greatly lower CVD risk.
Exercise boosts heart health by improving blood flow, lowering blood pressure, and bettering lipid levels. Aim for 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly.
Medical Management of Risk Factors
Controlling risk factors through medicine is also key in preventing cerebrovascular disease and stroke. This involves managing hypertension, diabetes, and high cholesterol with meds and lifestyle changes.
| Risk Factor | Management Strategy |
| Hypertension | Antihypertensive medication, lifestyle changes |
| Diabetes | Glycemic control through medication and diet |
| High Cholesterol | Statins, lifestyle modifications |
Antiplatelet and Anticoagulant Therapies
For those at high stroke risk or with stroke history, antiplatelet and anticoagulant therapies may be needed. These prevent blood clots. Antiplatelet drugs like aspirin and anticoagulants like warfarin are used to lower ischemic stroke risk.
It’s important for patients to team up with their doctors to find the best prevention plan. This plan should match their risk factors and medical history.
Living with Cerebrovascular Disease
Getting a cerebrovascular disease diagnosis starts a lifelong journey. It’s about managing and adapting to the condition. Understanding how to live with it is key.
Long-term Management Strategies
Managing cerebrovascular disease long-term means using medicine, changing our lifestyle, and keeping an eye on our health. We need to work with our doctors to create a plan that fits us.
Important strategies include:
- Medication Adherence: Taking our medicines as told to control risks and avoid problems.
- Lifestyle Modifications: Eating right, staying active, and quitting smoking to lower stroke risk.
- Regular Check-ups: Seeing our doctors often to check on our health and adjust our treatment if needed.
Support Systems and Resources
Dealing with cerebrovascular disease can be tough, both physically and emotionally. Having a strong support system is crucial.
Support can come from:
- Family and friends who offer emotional support and help with daily tasks.
- Support groups, online or in-person, where we can share our stories and connect with others.
- Healthcare professionals who guide and treat us.
Psychological Impact and Coping Mechanisms
Cerebrovascular disease can affect our minds, causing anxiety, depression, and frustration. It’s important to recognize these feelings and find ways to cope.
Ways to handle the mental side include:
- Cognitive-behavioral therapy (CBT): Helps change negative thoughts and behaviors.
- Stress Management Techniques: Like meditation, yoga, or deep breathing to calm down.
- Social Engagement: Keeping in touch with loved ones and the community to fight loneliness.
By managing cerebrovascular disease well, we can live better and avoid more problems.
Recent Advances in Cerebrovascular Research
New discoveries in cerebrovascular research are changing how we treat stroke and other brain diseases. We’re seeing big improvements thanks to better medical tools, research methods, and understanding of the causes.
Emerging Treatments and Technologies
New treatments for stroke are being developed. Mechanical thrombectomy has greatly improved care for big blockages in the brain. Also, research on clot-busting drugs is ongoing, aiming for safer and more effective options.
Telestroke networks are also growing. They help doctors treat stroke patients from far away. This technology is crucial for getting timely care to those who need it most.
Promising Areas of Study
Research on atherosclerosis and its brain effects is very promising. It’s helping us find new ways to prevent and treat brain diseases. Studies on inflammatory pathways in atherosclerosis could lead to new treatments.
Genetic studies are also advancing our understanding of brain diseases. They might help us tailor treatments to each patient’s needs.
Telemedicine and Stroke Care
Telemedicine is key in stroke care, especially in areas far from hospitals. Telestroke programs help doctors quickly assess and treat patients. This makes sure patients get the right care fast.
“Telemedicine has been a game-changer in stroke care, enabling us to reach patients in remote areas and provide them with the same level of care as those in urban centers.”
| Advancements | Impact on Stroke Care |
| Mechanical Thrombectomy | Improved outcomes for large vessel occlusions |
| Telestroke Networks | Enhanced access to stroke care in underserved areas |
| Research into Atherosclerosis | Potential for novel therapeutic targets |
As we keep moving forward in cerebrovascular research, these changes will greatly help patients. New technologies and treatments will improve how we manage brain diseases. This will make a big difference in people’s lives.
Conclusion
A stroke occurs when the blood supply to the brain is interrupted.
A cerebral aneurysm is when a blood vessel in the brain bulges. If it bursts, it can cause a hemorrhagic stroke. Knowing the risks and symptoms can help catch these problems early.
We’ve looked at different parts of cerebrovascular disease. This includes ischemic and hemorrhagic strokes, transient ischemic attacks, and vascular dementia. To manage these, we need a full plan. This includes changing our lifestyle, managing risk factors, and acting quickly when needed.
Learning about cerebrovascular disease and its link to stroke helps us deal with it better. This knowledge lets us take steps to keep our blood vessels healthy. It also helps us lower the chance of having a stroke.
FAQ
Is cerebrovascular disease the same as a stroke?
No, cerebrovascular disease (CVD) is a broader term. It includes many conditions affecting the brain’s blood vessels, including stroke. But not all CVD leads to a stroke.
What is the difference between ischemic and hemorrhagic stroke?
Ischemic stroke happens when a brain blood vessel is blocked. This reduces blood flow. Hemorrhagic stroke is when a brain blood vessel bursts, causing bleeding.
What are the risk factors for cerebrovascular disease?
Risk factors for CVD include things you can change like high blood pressure and smoking. Also, things you can’t change like age and family history.
What is a Transient Ischemic Attack (TIA)?
A TIA, or “mini-stroke,” is a short-term blockage of brain blood flow. It’s often a warning sign for a future stroke.
How is cerebrovascular disease diagnosed?
Doctors use clinical evaluation and imaging like MRI or CT scans to diagnose CVD. They also check blood flow and look for vascular disorders.
What are the treatment options for acute stroke?
Acute stroke treatment includes dissolving clots with thrombolytic therapy. It also includes removing clots with mechanical thrombectomy. Supportive care helps manage symptoms and prevent complications.
Can cerebrovascular disease be prevented?
Yes, you can prevent CVD. Lifestyle changes like a healthy diet and regular exercise help. Managing risk factors like high blood pressure and diabetes is also key.
What is vascular dementia?
Vascular dementia is a decline in cognitive function due to reduced brain blood flow. It often results from CVD or stroke.
How does a cerebral aneurysm relate to stroke?
A cerebral aneurysm is a weak spot in a blood vessel that can rupture. This leads to hemorrhagic stroke. Even unruptured aneurysms can cause symptoms by pressing on brain tissue.
What is the role of antiplatelet and anticoagulant therapies in CVD management?
These therapies prevent blood clots from forming or growing. They reduce the risk of ischemic stroke in people with CVD.
How can individuals cope with the psychological impact of cerebrovascular disease?
To cope, seek support from family and friends. Join support groups and do stress-reducing activities. Keeping a positive outlook also helps.
References
National Center for Biotechnology Information. Cerebrovascular Disease and Stroke Overlap and Distinction. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK431070/