Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, millions of people worldwide suffer from a stroke. This is a medical emergency caused by a blockage of blood flow to the brain. It’s very important to get medical help fast to avoid serious brain damage or death.Stroke disease is an emergency. Learn the critical steps to take to help stop a stroke in progress. This guide is essential.
Understanding the urgency of stroke treatment can save lives. Quick action can greatly improve a patient’s chances of recovery. We will look at the key steps to stop a stroke and save a life.
Spotting the signs of a CVA (Cerebrovascular Accident), or stroke, is the first step. Acting quickly to seek medical help is essential. This is key for effective tpa stroke treatment and better stroke recovery chances.
Key Takeaways
- Recognize the signs of a stroke to act quickly.
- Timely medical intervention is crucial for preventing complications.
- Understanding stroke treatment options is vital.
- TPA stroke treatment can significantly improve recovery chances.
- Prompt action enhances stroke recovery prospects.
Understanding Stroke Disease: The Brain Under Attack

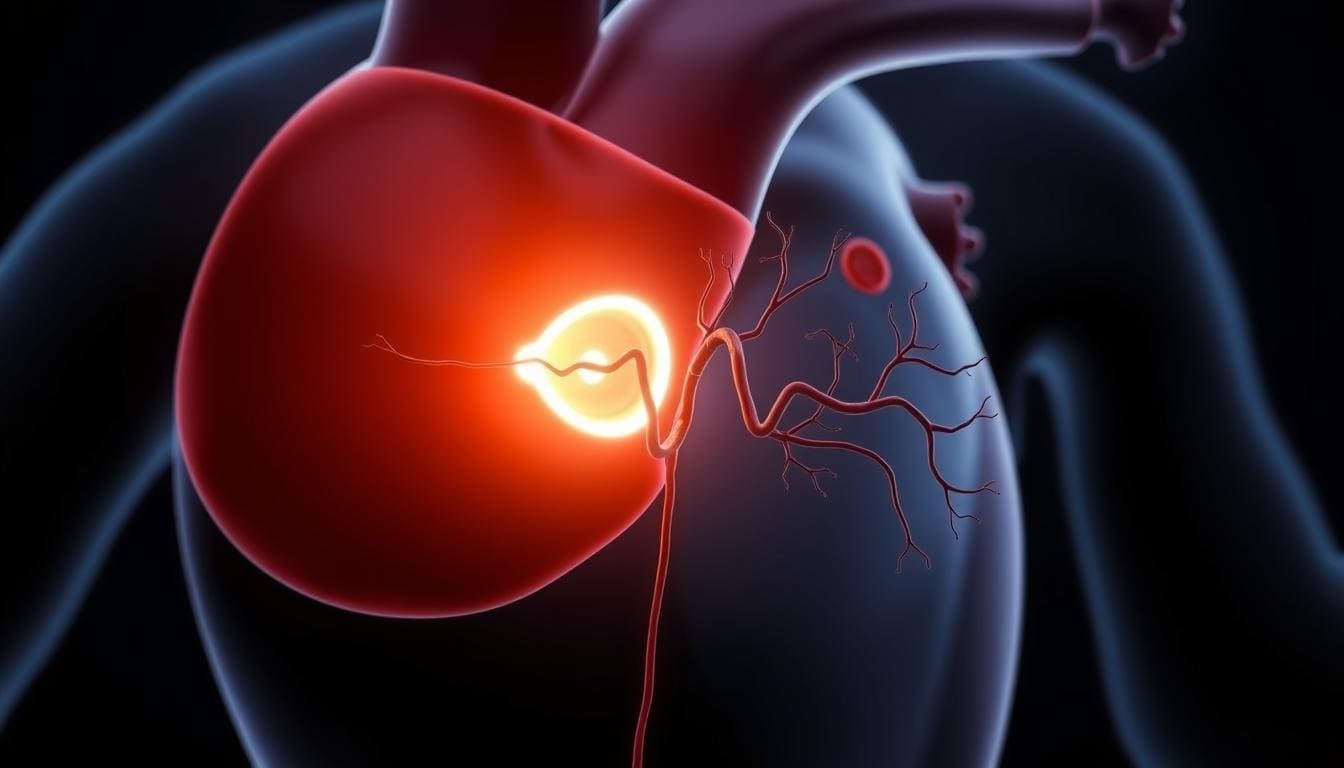
When the brain doesn’t get enough blood, a serious problem can start. This is called a stroke. It happens when a blood vessel in the brain either gets blocked or bursts. Knowing how stroke works is key to treating it well.
Definition and Pathophysiology of Cerebrovascular Accidents (CVA)
A CVA, or cerebrovascular accident, is when brain function suddenly stops because of no blood. It’s caused by complex problems at the cellular and molecular levels. For example, not enough oxygen and glucose can lead to cell death.
Ischemic vs. Hemorrhagic Stroke: Critical Differences
Strokes are mainly two types: ischemic and hemorrhagic. Ischemic strokes block a blood vessel, cutting off brain blood flow. Hemorrhagic strokes happen when a blood vessel bursts, causing bleeding in or around the brain. Knowing these differences helps doctors choose the right treatment.
Transient Ischemic Attacks (TIAs): Warning Signs
TIAs, or transient ischemic attacks, are short disruptions in brain blood flow. They are often called “mini-strokes.” TIAs show symptoms like a stroke but go away in 24 hours. Spotting TIAs early is important to stop a big stroke.
It’s important to know the risks and signs of stroke. By understanding what a stroke is, its types, and warning signs, we can help prevent and treat them.
Recognizing Stroke Symptoms: The BE-FAST Approach
Knowing the signs of a stroke is key to getting help fast. Strokes can cause a lot of harm, but quick action can help a lot.
Classic Warning Signs of Stroke
There are common signs of a stroke that everyone should know. These include sudden weakness or numbness in the face, arm, or leg. Also, trouble speaking or understanding speech, sudden vision changes, dizziness, or loss of balance.
The BE-FAST Acronym Explained
Use the BE-FAST acronym to remember stroke signs. BE-FAST stands for:
- B – Balance: Sudden dizziness or loss of balance.
- E – Eyes: Sudden vision changes or loss of vision.
- F – Face drooping: One side of the face drooping or numbness.
- A – Arm weakness: Sudden weakness or numbness in one arm.
- S – Speech difficulty: Slurred speech or difficulty speaking.
- T – Time to call 911: If someone shows these symptoms, call for emergency services right away.
Left-Sided vs. Right-Sided Stroke Symptoms
Stroke symptoms can differ based on the brain side affected. Left-sided stroke symptoms often include trouble with language, like aphasia, and right-sided weakness. On the other hand, right-sided stroke symptoms might include problems with spatial awareness and left-sided weakness. Knowing these differences is important for the right care and recovery.
By knowing the BE-FAST acronym and the differences in left-sided and right-sided stroke symptoms, people can react quickly. This can save lives and prevent long-term damage.
The Golden Hour: Why Time is Critical in Stroke Treatment
The ‘time is brain’ mantra shows how fast we must act in acute stroke cases. Every minute counts because delays can cause a lot of brain cell loss. When a stroke hits, the brain is in danger, and quick medical help is key to avoid lasting harm.
Brain Cell Loss Timeline During Acute Stroke
Understanding the urgency of stroke treatment can save lives.
Time-Dependent Treatment Options
There are several treatments for acute stroke, and they work best if done quickly. These include using tPA and mechanical thrombectomy for certain patients. The sooner these treatments start, the better the patient’s chances of recovery.
The “Time is Brain” Concept Explained
The “time is brain” idea shows how crucial time is during a stroke. Every minute without treatment means more brain tissue is lost. This isn’t just a saying; it’s a real measure of how brain function decreases with time delays in treatment.
| Time Elapsed | Brain Cells Lost | Potential Outcome |
| 0-3 hours | Significant loss begins | Best window for tPA treatment |
| 3-6 hours | Continued loss accelerates | Mechanical thrombectomy may be considered |
| 6+ hours | Severe loss, potential for extensive damage | Limited treatment options, focus on prevention of further strokes |
Grasping the urgency of time in stroke treatment helps both doctors and the public act fast. This can save lives and lessen the stroke’s long-term effects.
Immediate Actions to Take When Someone is Having a Stroke
A stroke is a serious medical emergency that needs quick action. Knowing what to do can save someone’s life. Every second is critical for their recovery.
Call911: The First Critical Step
If you think someone is having a stroke, call 911 right away. Don’t try to drive them to the hospital or let them sleep. Emergency responders are trained to help and can give important care on the way.
Proper Positioning and Support Techniques
While waiting for help, make sure the person is comfortable. Gently help them sit or lie down with their head up a bit. Also, loosen tight clothes around their neck to help them breathe better.
What NOT to Do During a Suspected Stroke
It’s also key to know what not to do. Don’t give them any medicine, food, or water. It could make things worse or mess up treatment. Also, don’t leave them alone or try to drive them to the hospital yourself.
Information to Gather for Emergency Responders
Having the right info can help responders give the best care. Try to remember: when the symptoms started, any health conditions, and their current medicines. This info is vital for the right treatment.
By acting fast, you can greatly improve someone’s chances during a stroke. Remember, time is brain, and quick action is key.
Emergency Medical Response to Stroke
When a stroke happens, every second is crucial. Emergency medical services (EMS) are key in acting fast and right. They spot stroke signs, start care, and take patients to the best hospitals.
The emergency response to stroke has many important parts. EMS workers follow special steps for stroke patients.
EMS Protocols for Suspected Stroke
For suspected strokes, EMS uses the BE-FAST tool. It checks for stroke signs. They also:
- Check vital signs and start care
- Give oxygen if needed
- Set up IVs for medicine
- Call the hospital about the stroke patient
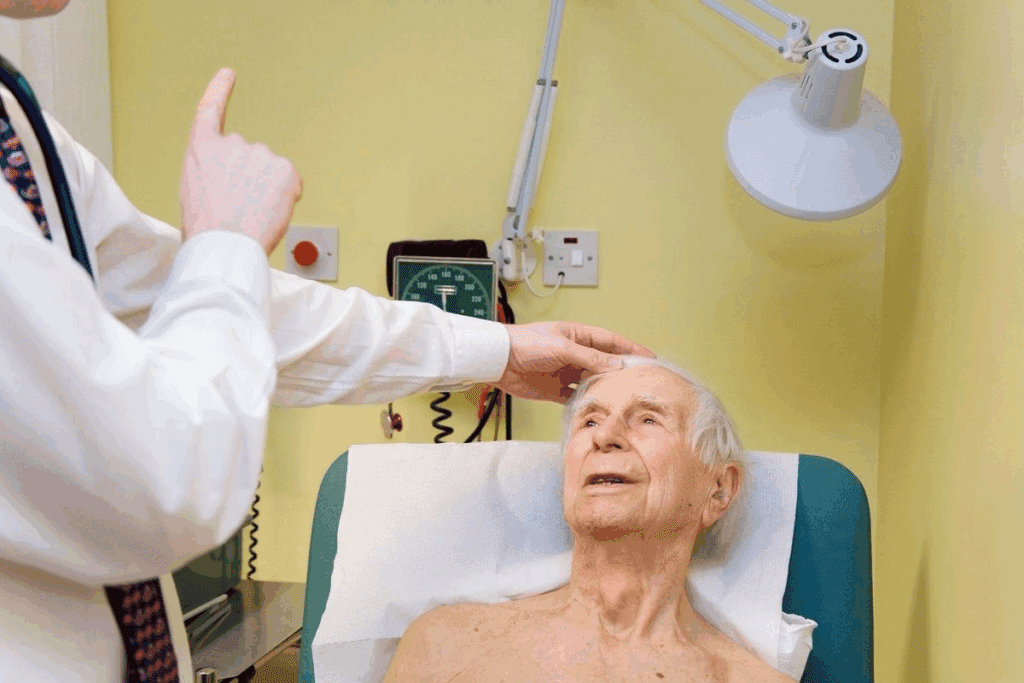
National Institutes of Health Stroke Scale (NIHSS) Assessment
The NIHSS helps check how bad a stroke is. It looks at:
- How awake the person is
- Eye and arm function
- Talking and language skills
- Other brain problems
Transport Decisions: Comprehensive vs. Primary Stroke Centers
EMS must choose where to take a stroke patient. They can go to a Primary Stroke Center (PSC) or a Comprehensive Stroke Center (CSC). PSCs start care, but CSCs have more advanced treatments.
- 24/7 endovascular therapy
- Advanced imaging
- Neurosurgery services
Going straight to a CSC can be lifesaving for those needing advanced care.
Knowing about EMS steps, NIHSS, and transport choices shows how complex and vital stroke response is.
Hospital Arrival: The Stroke Code Process
When you arrive at the hospital, the stroke code process starts. It’s a fast and detailed way to find and treat strokes. This is key to making sure patients get the right care fast.
Stroke Team Activation and Roles
The stroke team gets ready to work as soon as you arrive. This team has doctors, nurses, and other experts. They all work together to check and care for the patient.
Initial Assessment and Triage Procedures
The first step is a quick check of your health. This includes looking at your medical history and current symptoms. Triage helps figure out how serious the stroke is and what to do first.
Critical Time Benchmarks in Acute Stroke Care
Time is very important when treating strokes. There are key times to watch, like how long it takes to start treatment. These times help make sure care is given quickly and correctly.
By making the stroke code process better, hospitals can help patients more. We aim to give top-notch care that meets each patient’s needs.
Diagnostic Procedures for Acute Stroke
Effective stroke care starts with quick and accurate tests. When someone shows stroke symptoms, doctors must act fast. They need to know the stroke type and how severe it is to treat it right.
Non-Contrast CT Scans: The First-Line Imaging
Non-contrast CT scans are often the first test for acute strokes. They are fast and easy to get. This test helps tell if the stroke is caused by a blood clot or bleeding.
Non-contrast CT scans are especially good at finding bleeding. They show bleeding as bright spots on the scan.
Advanced Imaging: CT Angiography and Perfusion Studies
For ischemic stroke suspects, CT angiography (CTA) and CT perfusion (CTP) studies are key. CTA spots big blockages in blood vessels. CTP checks blood flow and brain tissue health.
These tests help doctors decide on treatments. They might suggest using a mechanical device to remove the clot.
MRI and Other Diagnostic Tools
Magnetic Resonance Imaging (MRI) shows brain and blood vessel details. It’s not always the first choice because it takes longer. But, MRI is great for certain cases, like checking for stroke look-alikes or strokes in the back of the brain.
Other tools like transcranial Doppler ultrasound and EEG might also help. They are used in specific situations to help diagnose and manage strokes.
Using all these tests together helps doctors make the best treatment plans. This approach can lead to better outcomes for stroke patients.
Ischemic Stroke Treatment: Clot-Busting Medications
Clot-busting medications are a key treatment for ischemic stroke. They help restore blood flow to the brain. These drugs dissolve the clot blocking a blood vessel, reducing stroke severity.
Tissue Plasminogen Activator (tPA): Mechanism and Administration
Tissue Plasminogen Activator (tPA) is a drug that breaks down blood clots. It’s given through an IV. The sooner tPA is given, the better the results.
Alteplase vs. Tenecteplase: Comparing Options
Alteplase and tenecteplase are drugs used to treat ischemic stroke. Alteplase is more common, but tenecteplase might be more effective. Research is ongoing to see which is safer and more effective.
| Characteristics | Alteplase | Tenecteplase |
| Dosing Regimen | Complex, weight-based | Single bolus, weight-based |
| Fibrin Specificity | Moderate | High |
| Half-life | Short | Longer |
Eligibility Criteria and Contraindications
To get thrombolytic therapy, you must meet certain criteria. This includes how long since the stroke started and your medical history. But, there are things that make you not eligible, like recent surgery or bleeding. Doctors carefully check these to keep you safe.
Time Windows for Thrombolytic Therapy
How long you have to get thrombolytic therapy is very important. It’s usually within 4.5 hours of the stroke. Getting treatment quickly can lead to better results. But, some people might get treatment later if they meet certain criteria.
It’s crucial to get medical help right away if you think you’re having a stroke. This can greatly improve your chances with clot-busting medications.
Mechanical Thrombectomy: Advanced Intervention for Large Vessel Occlusions
Mechanical thrombectomy has changed how we treat acute ischemic strokes. It’s a new way to treat severe strokes by removing clots from large vessels. This has greatly improved patient outcomes.
Patient Selection for Endovascular Treatment
Choosing the right patients for mechanical thrombectomy is key. We look at several factors. These include how long since the stroke started, the patient’s health, and what the scans show.
Advanced scans like CT angiography and perfusion studies help us find patients who can still recover. This is crucial for deciding who can benefit from this treatment.
Key criteria for patient selection include:
- Presence of a large vessel occlusion
- Minimal or no significant comorbidities
- Potential for neurological recovery
- Time window for intervention, typically within 6-24 hours
The Thrombectomy Procedure Explained
Mechanical thrombectomy uses a catheter to remove clots from blocked vessels. We use tools like stent retrievers or aspiration catheters to clear the blockage.
The procedure is done under sedation or anesthesia. Quick and effective thrombectomy can bring blood back to the brain. This can help reverse stroke damage.
Extended Time Windows Based on Imaging
Oldly, the time to treat a stroke was short. But new imaging lets us treat more patients. We can see who might still benefit from treatment even after the usual time has passed.
| Imaging Modality | Information Provided | Clinical Utility |
| CT Angiography | Vessel occlusion location and extent | Helps determine eligibility for thrombectomy |
| CT Perfusion | Assessment of cerebral blood flow and volume | Identifies areas of salvageable brain tissue |
| MRI DWI/FLAIR | Extent of infarcted tissue and potential penumbra | Guides decision-making for late-window thrombectomy |
By carefully choosing patients and using new imaging, we can make mechanical thrombectomy more effective. This helps improve outcomes for those with severe strokes.
Hemorrhagic Stroke Interventions and Management
Managing hemorrhagic stroke requires a mix of medical and surgical steps. Quick and right actions are key. They must match the patient’s specific needs.
Medical Management of Intracranial Bleeding
At first, medical care is vital for hemorrhagic stroke. It helps control pressure inside the skull, keeps blood pressure stable, and stops seizures. Anticonvulsants may be given to stop seizures, which can make things worse.
Surgical Options for Hemorrhagic Stroke
Surgery is often needed to ease brain pressure, fix damaged blood vessels, and clear out blood. Surgery depends on the hemorrhage’s location and how bad it is. The main goal is to lessen brain damage and help the patient recover better.
Coiling and Clipping for Ruptured Aneurysms
When a hemorrhagic stroke is due to a burst aneurysm, coiling and clipping are key. Coiling fills the aneurysm with coils to stop more bleeding. Clipping puts a clip on the aneurysm’s neck to hold it in place. Both methods aim to stop bleeding again and help the patient get better.
| Procedure | Description | Benefits |
| Coiling | Filling the aneurysm with coils | Minimally invasive, reduces risk of re-bleeding |
| Clipping | Placing a clip around the aneurysm neck | Effective for certain aneurysm locations, durable solution |
Specialized Stroke Units: Optimizing Post-Acute Care
Specialized stroke units have changed how we care for stroke patients after they leave the hospital. These units offer advanced care. They use a team of experts to help patients get better.
Benefits of Dedicated Stroke Units
Dedicated stroke units help patients get better faster and stay in the hospital less time. They focus on stroke care, making treatment better and more efficient.
The Multidisciplinary Care Team Approach
A multidisciplinary care team is at the heart of these units. It includes doctors, nurses, and therapists. They work together to create a care plan for each patient.
Monitoring and Managing Complications
Managing complications is key in stroke care. Specialized units watch for problems like infections. They act fast if they see any issues.
By being proactive, these units help patients recover better. They improve the lives of stroke survivors.
Post-Stroke Stabilization and Monitoring
The time after a stroke is very important. It’s when we need to be careful to avoid more brain damage. We focus on managing blood pressure, stopping other problems, and checking the brain often.
Blood Pressure Management Protocols
Keeping blood pressure in check is key after a stroke. Hypertension is a big problem that must be controlled. We have special plans to keep blood pressure right for each patient.
| Blood Pressure Category | Systolic BP (mmHg) | Diastolic BP (mmHg) |
| Normal | < 120 | < 80 |
| Elevated | 120-129 | < 80 |
| Hypertension Stage 1 | 130-139 | 80-89 |
Preventing Secondary Complications
Stopping other problems is also very important. We work to prevent deep vein thrombosis (DVT), help with swallowing difficulties, and keep patients safe from falls. We use medicine, physical therapy, and nursing care to do this.
Ongoing Neurological Assessments
Checking the brain often is crucial. We look at level of consciousness, cranial nerve function, and motor strength. This helps us change treatment plans to help patients get better.
Early Rehabilitation Efforts for Stroke Recovery
Early rehabilitation is key for stroke survivors. Starting treatment quickly is vital for the best results. It helps patients regain lost abilities and live better lives.
Starting Rehabilitation in the Acute Setting
Rehab starts when the patient is stable. Early mobilization prevents problems like blood clots and bed sores. It keeps muscles strong and joints moving.
Our team creates a special plan for each patient. They look at the patient’s needs and make a plan to help them.
Physical, Occupational, and Speech Therapy Approaches
A good rehab program includes physical, occupational, and speech therapy. Physical therapy boosts strength and mobility. Occupational therapy helps with daily tasks. Speech therapy fixes communication and swallowing issues.
These therapies are made just for each patient. They help meet their unique needs.
J-Shaped Walking Aids and Adaptive Equipment
Tools like J-shaped walking aids help a lot. They give support and let patients walk safely. Other tools include wheelchairs, grab bars, and special utensils for everyday tasks.
Setting Realistic Recovery Goals
Setting goals is important for staying motivated. Our team works with patients and families to set goals. This way, everyone knows what to work towards.
| Therapy Type | Focus Area | Benefits |
| Physical Therapy | Mobility and Strength | Improves walking, balance, and overall physical function |
| Occupational Therapy | Daily Living Skills | Enhances ability to perform daily tasks and maintain independence |
| Speech Therapy | Communication and Swallowing | Improves speech clarity and addresses swallowing disorders |
Preventing Recurrent Strokes: Secondary Prevention
Secondary prevention is key to lowering the chance of having another stroke after the first one. It’s important to use strategies that help prevent another stroke. We will look at the main parts of secondary prevention, like medicines, managing risks, lifestyle changes, and follow-up care.
Antiplatelet and Anticoagulation Medications
Medicines are a big part in stopping strokes from happening again. Antiplatelet medications, like aspirin, stop platelets from clumping together. This helps prevent blood clots. Anticoagulation medications, such as warfarin, are important for people with heart problems that can cause strokes. The right medicine depends on why the stroke happened and the patient’s health.
Managing Modifiable Risk Factors
It’s important to manage risk factors that can be changed. These include high blood pressure, diabetes, high cholesterol, and smoking. Hypertension is a big risk, and keeping blood pressure in check can lower stroke risk. Managing diabetes and hyperlipidemia with diet and exercise is also key. Quitting smoking is crucial because it doubles the risk of stroke.
Lifestyle Modifications for Stroke Prevention
Making lifestyle changes is important to prevent strokes. Eating a healthy diet full of fruits, veggies, and lean proteins is good. Avoiding too much fat, salt, and sugar is also important. Regular physical activity keeps the heart healthy. Keeping a healthy weight and drinking less alcohol are also key. These changes help lower stroke risk and improve health overall.
Follow-up Care and Monitoring
Regular check-ups are important to make sure prevention plans are working. This includes visits to the doctor, tracking risk factors, and taking medicines as prescribed. Patients and their caregivers need to know the signs of another stroke and the need to get help right away.
Conclusion: Empowering Stroke Awareness and Response
Understanding the urgency of stroke treatment can save lives.
Stroke awareness and quick action are vital in lessening the effects of stroke. Being informed and ready helps us react quickly when someone has a stroke. This can lead to better results for patients. Our aim is to give readers the tools to act fast, ensuring those affected get the best care.
By spreading the word about stroke awareness and response, we can all help reduce stroke’s impact. We urge everyone to share this information, building a community that’s ready and able to handle stroke emergencies.
FAQ
What is a stroke and how does it occur?
A stroke happens when the brain doesn’t get enough oxygen and nutrients. This can be due to a blockage or a rupture in blood vessels.
What are the different types of strokes?
There are three main types of strokes. Ischemic strokes are caused by blockages. Hemorrhagic strokes are due to ruptures. TIAs are temporary disruptions in blood flow.
What is the BE-FAST acronym, and how does it help in recognizing stroke symptoms?
BE-FAST is an acronym for Balance, Eyes, Face, Arm, Speech, and Time. It helps spot stroke symptoms by looking for imbalance, vision changes, facial drooping, arm weakness, speech issues, and the need for quick action.
Why is timely medical intervention crucial in stroke treatment?
Quick medical help is key because the brain loses cells fast during a stroke. Fast treatment can reduce damage and improve results.
What is tPA, and how is it used in stroke treatment?
tPA is a clot-busting drug for ischemic strokes. It dissolves clots to restore blood flow. It’s most effective when given quickly.
What are the eligibility criteria for thrombolytic therapy with tPA?
To get tPA, you must be within a certain time frame. You need a confirmed ischemic stroke diagnosis. And you can’t have recent bleeding or certain health issues.
What is mechanical thrombectomy, and when is it used?
Mechanical thrombectomy removes blood clots from large brain vessels. It’s for patients with large vessel occlusions who meet specific criteria and have certain imaging results.
How are hemorrhagic strokes managed?
Hemorrhagic strokes are treated with medical help to control bleeding. Surgery may be needed to fix damaged blood vessels. Procedures like coiling and clipping are used for ruptured aneurysms.
What is the importance of post-stroke rehabilitation?
Post-stroke rehab is vital for patients to regain lost functions. It helps them adapt to any lasting effects and improve their life quality. It includes physical, occupational, and speech therapy.
How can recurrent strokes be prevented?
Preventing future strokes involves secondary prevention. This includes using antiplatelet and anticoagulation drugs. It also means managing risk factors and making lifestyle changes.
What is the role of a stroke unit in patient care?
A stroke unit offers specialized care for stroke patients. It has a team approach, close monitoring, and manages complications. All these help improve patient outcomes.
How can individuals empower themselves to respond to strokes effectively?
People can empower themselves by learning to spot stroke symptoms with BE-FAST. They should understand the importance of quick medical help. And know what to do when someone has a stroke.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31662037/