For those with drug-resistant epilepsy (DRE), resective epilepsy surgery could change their life. About one-third of people with epilepsy don’t get better with medicine. So, other treatments are key.
To be a good epilepsy surgery candidate, you’ve tried at least two medicines without success. A detailed check is done to see if surgery is right for you. This includes looking at your seizure type, how often they happen, and how well past treatments worked. The ultimate guide for Epilepsy surgery candidates. Discover the critical criteria and hopeful outlook for those seeking a permanent cure.
Key Takeaways
- Drug-resistant epilepsy (DRE) is a condition where seizures are not controlled with medication.
- Resective epilepsy surgery is a viable treatment option for suitable candidates.
- Patients must have tried at least two antiseizure medicines without success to be considered.
- A detailed evaluation is needed to decide if surgery is right.
- The goal of epilepsy surgery is to reduce or stop seizures, making life better.
Understanding Drug-Resistant Epilepsy
It’s key to understand drug-resistant epilepsy to find out who might benefit from epilepsy surgery. This condition, also known as refractory epilepsy, happens when people keep having seizures even after trying many medicines.
Definition and Prevalence
Drug-resistant epilepsy means that two medicines that are safe and work well don’t stop seizures. About 30% of people with epilepsy face this issue. It shows the need for new ways to treat the condition.
Impact on Quality of Life
Drug-resistant epilepsy greatly affects a person’s life. It can cause cognitive decline, psychosocial dysfunction, and a higher risk of death. It makes everyday tasks hard, like driving and working, leading to feelings of isolation and frustration.
When Medications Fail
If medicines don’t stop seizures, looking for other treatments is important. Epilepsy surgery is an option for some, mainly those with temporal lobe epilepsy (TLE). Choosing surgery needs a detailed check to see if it could lead to a seizure-free life.
In summary, drug-resistant epilepsy is a complex issue that needs a detailed approach to manage. Knowing its definition, how common it is, and its effects is vital for doctors to provide the best care. This includes checking if surgery could help.
The Journey to Becoming an Epilepsy Surgery Candidate

The path to epilepsy surgery starts with a detailed check-up. This step is key to see if someone can have surgery for epilepsy.
Initial Diagnosis and Treatment Attempts
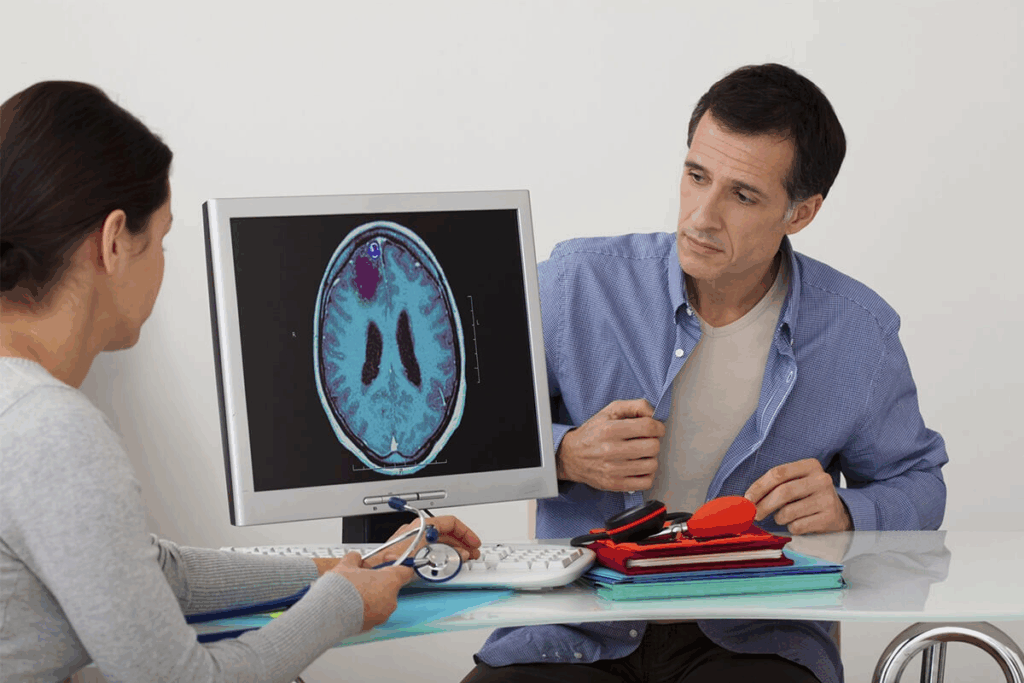
First, patients get a full check to find out what’s causing their epilepsy. Tests like magnetic resonance imaging (MRI) look for problems like hippocampal sclerosis or focal cortical dysplasia. If medicines don’t stop the seizures, more tests are needed.
Referral to Comprehensive Epilepsy Centers
Those who keep having seizures after trying medicines go to special centers. These places have the latest tools and teams ready to check if surgery is right.
The Multidisciplinary Team Approach
At these centers, experts like neurologists and neurosurgeons team up. They do tests like video-EEG monitoring to find where seizures start. They also look at the risks and benefits of surgery.
This careful check is vital to find out who can have epilepsy surgery. With the latest tests and teamwork, doctors can help patients have a chance at living without seizures.
Ideal Epilepsy Surgery Candidates: Key Criteria
Finding the right candidates for epilepsy surgery is a detailed process. It looks at several important factors. Surgery is an option for those with drug-resistant epilepsy (DRE) who can’t control their seizures with medicine.
Confirmed Diagnosis of Drug-Resistant Epilepsy
A confirmed DRE diagnosis is essential. This means trying two or more medicines that are safe and work well, but not stopping seizures. Drug-resistant epilepsy greatly affects a person’s life, making surgery a possible game-changer.
“The failure to achieve seizure freedom with antiepileptic drugs is a critical indicator for considering surgical options.”
Identifiable Seizure Focus
Another important factor is finding an identifiable seizure focus. This is the brain area where seizures start. Doctors use electroencephalography (EEG) and other tests to find this area.
| Diagnostic Tool | Purpose |
| EEG | To monitor and record electrical activity in the brain, helping to identify seizure patterns and localize the seizure focus. |
| Neuroimaging (e.g., MRI) | To visualize the brain’s structure and identify any abnormalities that may be causing seizures. |
Risk-Benefit Assessment
A detailed risk-benefit assessment is done to see if surgery is right. It looks at the chance of stopping seizures and the possible risks of surgery.
Healthcare experts use these criteria to find the best candidates for surgery. This helps patients make smart choices about their treatment.
Comprehensive Presurgical Evaluation Process
Identifying the right candidates for epilepsy surgery is key. A detailed evaluation process is used. It includes several tests to see if surgery is a good option.
Video-EEG Monitoring
Video-EEG monitoring (VEM) is a big part of the evaluation. It records EEG and video at the same time. This helps find where seizures start and what they look like.
Neuroimaging Studies
Neuroimaging is important for finding brain problems that cause seizures. The main tests used are:
MRI Findings
Magnetic Resonance Imaging (MRI) is great at finding brain lesions. It shows things like hippocampal sclerosis and cortical dysplasia. High-quality MRI is needed to spot where seizures might start.
FDG-PET and SPECT
Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) and Single-Photon Emission Computed Tomography (SPECT) are used to see how the brain works. FDG-PET looks at glucose use in the brain. SPECT, like ictal SPECT, shows blood flow changes during a seizure. This helps pinpoint where seizures start.
| Imaging Modality | Primary Use | Key Findings |
| MRI | Structural Imaging | Hippocampal sclerosis, cortical dysplasia |
| FDG-PET | Functional Imaging | Hypometabolism in seizure focus |
| SPECT | Functional Imaging | Increased blood flow during seizure |
Neuropsychological Assessment
A neuropsychological assessment is done to check brain function. It looks at things like memory and thinking. This helps see how surgery might affect the brain.
Types of Epilepsy Most Suitable for Surgical Intervention
Some types of epilepsy can greatly benefit from surgery. This offers hope to those with seizures that don’t respond to medication. Surgery is now seen as a good option for many epilepsy types, mainly those with clear seizure origins.
Temporal Lobe Epilepsy with Hippocampal Sclerosis
Temporal lobe epilepsy (TLE) with hippocampal sclerosis is a common and well-studied condition. Hippocampal sclerosis means the hippocampus, a key part of the temporal lobe, is scarred. This scarring is linked to seizures. Research shows that surgery to remove the affected area can greatly reduce or stop seizures in many patients.
Focal Cortical Dysplasia
Focal cortical dysplasia (FCD) is another condition that surgery can help. FCD is a birth defect where brain tissue develops abnormally. People with FCD often have seizures that don’t respond to medication. Surgery is a good option for them. Finding the exact area of abnormal tissue is key for a successful surgery.
Other Structural Lesions
Other structural issues can also be treated with surgery. These include brain tumors, vascular malformations, and other developmental malformations. The main thing is that there must be a clear, identifiable lesion that matches the seizure focus. New imaging techniques help find these lesions and plan the surgery.
Choosing surgery for epilepsy involves a detailed evaluation. This includes various tests to figure out the type of epilepsy and if surgery is right. Knowing the specifics of a patient’s epilepsy helps doctors offer the best treatment. This can lead to better seizure control and a better life for the patient.
Prognostic Factors for Successful Epilepsy Surgery Outcomes
Prognostic factors are key in predicting the success of epilepsy surgery. They help find the best candidates and forecast results.
Concordant EEG and Imaging Findings
When EEG and imaging tests agree on a seizure focus, success rates soar. Concordant findings guide surgeons to remove the right area. This leads to better control over seizures.
A study showed patients with matching EEG and MRI results had more success. They were more likely to be seizure-free after surgery.
Duration of Epilepsy
The length of time someone has epilepsy matters a lot. Those with epilepsy for a shorter time usually do better after surgery. This is because their brain networks are less spread out and complications are fewer.
Age and Neurological Status
Age and neurological health at surgery time also matter. Younger patients with fewer health issues tend to do better. Their brains are more flexible, making recovery easier.
| Prognostic Factor | Impact on Outcome |
| Concordant EEG and Imaging Findings | Increased likelihood of seizure freedom |
| Shorter Duration of Epilepsy | Better surgical outcomes due to less widespread epileptogenic networks |
| Younger Age and Fewer Neurological Deficits | More favorable outcomes due to greater brain plasticity |
In summary, factors like EEG and imaging agreement, shorter epilepsy time, and good health and age are vital. They help doctors pick the right patients and guess how well surgery will work.
Challenges in Identifying Epilepsy Surgery Candidates
Finding the right people for epilepsy surgery is tough. It takes a detailed look at many factors to see who might benefit.
MRI-Negative Epilepsy
MRI-negative epilepsy is a big problem. It means people have epilepsy but their MRI scans look normal. This makes it hard to find where the seizures start.
To find the right candidates, we need new ways to look at the brain. This is key for those with MRI-negative epilepsy.
Multiple or Diffuse Seizure Foci
Another challenge is multiple or diffuse seizure foci. When seizures come from different places in the brain, surgery gets harder.
We need to carefully check if removing the main seizure spot can help. This is important for these cases.
Discordant Test Results
Discordant test results add to the problem. When tests don’t agree, finding the seizure spot is tricky.
A team of experts is needed to sort out these differences. They help decide if surgery is right for the patient.
Surgical Options for Different Types of Candidates
There are many surgical options for people with epilepsy, each one suited to different needs. The right surgery depends on several things. These include the type of epilepsy, where seizures start, and the person’s health.
Resective Surgery
Resective surgery removes the brain area where seizures start. It’s often for those with temporal lobe epilepsy or a clear seizure spot. The aim is to cut down or stop seizures.
Laser Interstitial Thermal Therapy
Laser interstitial thermal therapy (LITT) is a new, less invasive way to treat seizures. It uses a laser to destroy the seizure focus. It’s great for hard-to-reach areas in the brain.
Neurostimulation Alternatives
For those not suited for resective surgery, neurostimulation alternatives are good options. These include:
- Vagus Nerve Stimulation (VNS): A device is implanted to help control seizures by stimulating the vagus nerve.
- Responsive Neurostimulation (RNS): A device is implanted to detect and stop abnormal brain activity, which can reduce seizures.
Choosing the right surgery involves a detailed look at the patient’s history, seizure type, and test results. Knowing the options helps candidates make better choices for their treatment.
Post-Surgery Expectations and Recovery
Epilepsy surgery is a big step for many patients. Knowing what to expect after surgery is important for a smooth recovery. The journey after surgery includes key parts that affect the surgery’s success.
Seizure Freedom Rates
Patients worry about becoming seizure-free after surgery. Research shows that the chance of being seizure-free depends on the surgery type and patient factors. For example, those with temporal lobe epilepsy might have a better chance than those with more complex epilepsy.
Medication Management After Surgery
Medication management is vital after surgery. Patients might need to keep taking epilepsy drugs, but the dosage and number could change. The aim is to use the least amount of medication needed to control seizures.
Rehabilitation and Follow-up Care
Rehabilitation and follow-up care are key to recovery. Patients might need physical, occupational, or speech therapy to improve their skills. Regular check-ups with the healthcare team are important to track progress, handle any issues, and adjust treatment plans as needed.
Understanding these post-surgery care aspects helps patients navigate their recovery. It leads to the best possible outcomes.
Conclusion: Making an Informed Decision About Epilepsy Surgery
Epilepsy surgery is a good option for those with drug-resistant epilepsy. To decide, you need to know who can get surgery, the evaluation process, and the planning options.
People with neocortical epilepsy or other types might find surgery helpful. Getting evaluated at a top epilepsy center is key to finding the best treatment. This article helps you understand the important points to consider for surgery.
Choosing surgery should be a well-thought-out decision. Knowing the benefits and risks is essential. With a team of experts, you can make the right choice for your health.
FAQ
What is drug-resistant epilepsy?
Drug-resistant epilepsy is when people keep having seizures even after trying many medicines. It really affects their life quality.
What is the primary goal of epilepsy surgery?
The main goal of epilepsy surgery is to stop or lessen seizures. This helps improve the patient’s life a lot.
What is involved in the comprehensive presurgical evaluation process?
The evaluation process includes many tests. These are video-EEG monitoring, MRI, and other imaging studies. It also includes neuropsychological assessments.
What types of epilepsy are more likely to benefit from surgical intervention?
Some types of epilepsy, like temporal lobe epilepsy, can really benefit from surgery. So can other structural issues like tumors.
What are the prognostic factors that influence the outcome of epilepsy surgery?
Several factors affect surgery outcomes. These include how well tests match, how long someone has had epilepsy, and their age and health.
What are the challenges in identifying suitable epilepsy surgery candidates?
Finding the right candidates can be tough. This includes cases where tests don’t match, or when seizures come from many places. It needs a detailed approach.
What are the surgical options available for epilepsy treatment?
There are a few surgery options. These include removing part of the brain, laser therapy, and using devices like vagus nerve stimulation.
What can patients expect after epilepsy surgery?
Patients might see a big drop in seizures or even stop having them. After surgery, doctors adjust medications. Rehabilitation and follow-up care are key for the best results.
How is the suitability of a patient for epilepsy surgery determined?
Doctors check if surgery is right by looking at seizure types and how often they happen. They also look at past treatments and do tests like EEG and MRI.
What is the role of a multidisciplinary team in evaluating epilepsy surgery candidates?
A team of doctors is very important. They do a deep evaluation, including tests, to see if surgery is a good option.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9562030/




































