Last Updated on December 1, 2025 by Bilal Hasdemir

icu meaning
Hospitals have special units for critical care. Did you know that nearly 1 in 5 hospital admissions in the United States requires some form of critical care? What is the ICU meaning? We explain if a Critical Care Unit (CCU) is more serious than an ICU. Get the definitive answer.
Different hospitals call these units by various names. They might say cardiac or critical care units, which are similar to an intensive care unit (ICU). We will look into the differences and similarities between these units. This will help us understand the ICU meaning and its importance in healthcare.
Key Takeaways
- The terms “Critical Care Unit” and “ICU” are often used interchangeably, but may have different implications depending on the hospital.
- ICU stands for Intensive Care Unit, a department specializing in critical care for patients with life-threatening conditions.
- The level of care in an ICU is typically more intense than in a standard hospital ward.
- Different hospitals may have varying criteria for admitting patients to an ICU.
- Understanding the ICU definition is crucial for patients and families navigating healthcare options.
Understanding Critical Care in Modern Healthcare

A high-tech critical care unit with state-of-the-art medical equipment. In the foreground, a team of dedicated healthcare professionals in sterile uniforms tending to a critically ill patient, monitors and life support systems surrounding the bed. Bright overhead lighting illuminates the scene, creating a sense of urgency and precision. In the middle ground, a panoramic view of the unit with additional beds, medical devices, and a bustling atmosphere of focused activity. The background fades into a clean, modern hospital setting, conveying the advanced capabilities of this critical care environment.
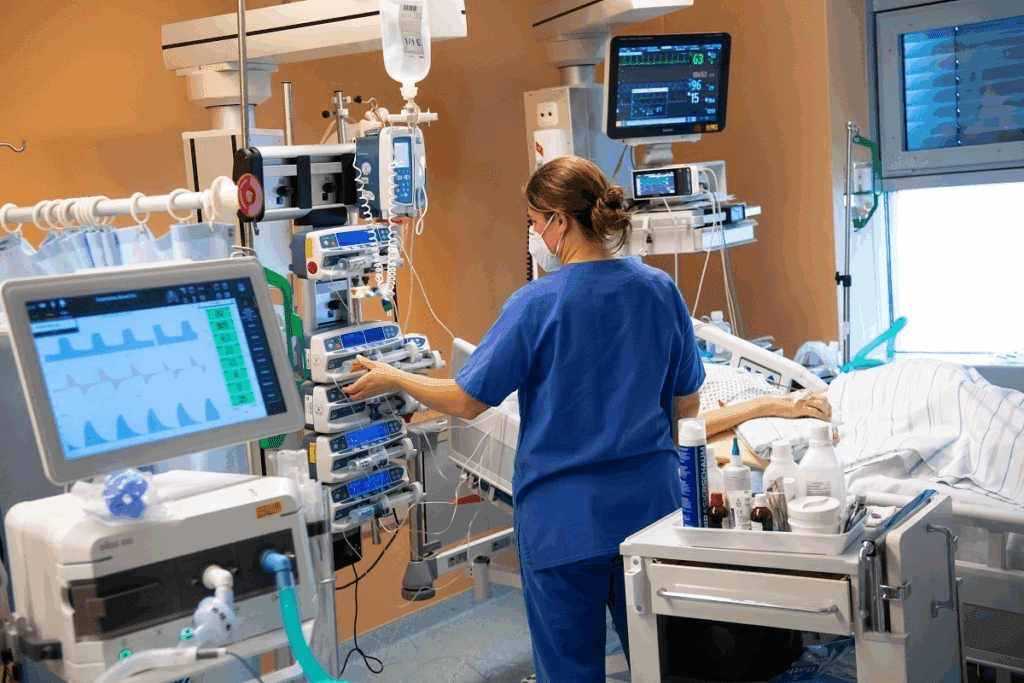
Healthcare keeps getting better, and critical care is key in saving lives. It’s a special part of medicine that deals with patients who are very sick. These patients need constant care and watching.
Over the years, critical care has changed a lot. It’s now better at handling severe and life-threatening cases. This is thanks to new medical tech, drugs, and understanding of serious illnesses.
The Evolution of Critical Care Medicine
The history of critical care is filled with important moments. The first ICUs started in the 1950s and 1960s. They were for patients with breathing problems, often from polio. Now, ICUs are high-tech places that handle many serious conditions.
- Advancements in Technology: New tech like ventilators and kidney machines has helped a lot.
- Specialization: ICUs now focus on specific areas like heart or brain problems. This makes treatment better.
- Multidisciplinary Care Teams: ICUs now have teams with doctors, nurses, and more. This team approach helps a lot.
The Role of Critical Care in Hospital Settings
Critical care units are crucial in hospitals. They are where the sickest patients get care. These units are always open, giving patients the care they need.
ICUs do many important things:
- Continuous Monitoring: They watch patients closely to catch any problems early.
- Life-Supporting Therapies: ICUs have the tools to help keep organs working, like breathing machines.
- Multidisciplinary Care: A team of experts works together to care for patients.
By knowing how critical care has evolved, we see how vital it is. It’s all about saving lives and making patients better.
What Does ICU Mean? Exploring ICU Meaning and Purpose
A sterile, modern hospital room with a focus on the central intensive care unit (ICU) bed. The room is well-lit with a warm, calming atmosphere, emphasizing the importance of patient care and medical vigilance. The bed is elevated, surrounded by various life-support equipment, intravenous lines, and monitoring devices, conveying the critical nature of the ICU setting. The walls are a neutral tone, with medical charts and equipment visible in the background, suggesting the highly technical nature of the environment. The scene captures the essence of an ICU, its purpose, and the seriousness of the care provided within.
ICU stands for Intensive Care Unit. It’s a special part of hospitals for very serious cases. Patients needing constant care and life-saving treatments go here.
Definition and Core Functions of an Intensive Care Unit
An Intensive Care Unit (ICU) is a special part of hospitals. It’s for patients who are very sick and need close watch. The main jobs of an ICU include:
- Providing life-supporting interventions such as mechanical ventilation.
- Continuous monitoring of vital signs and other critical parameters.
- Administering complex treatments and medications.
- Employing a multidisciplinary team approach to patient care.
The ICU has the latest technology and a team of experts in critical care.
Historical Development of ICUs in American Hospitals
The idea of ICUs started in the 1950s and 1960s. It was because of new medical tech and the need for special care for very sick patients. Over time, ICUs in American hospitals have changed a lot:
- Early Development: The first ICUs were for patients after surgery and those needing close watch.
- Advancements in Technology: New life-support tech and monitoring tools have made ICUs better.
- Specialization: Now, ICUs are more specialized, like cardiac or pediatric ICUs, for different needs.
Today, ICUs are key in healthcare. They give critical care to those who need it most.
Critical Care Unit vs. ICU: Are They Different?
A modern hospital ward with two distinct sections: an Intensive Care Unit (ICU) and a Critical Care Unit (CCU). The ICU is a brightly lit, sterile environment, with advanced medical equipment and attentive nurses monitoring critically ill patients. The CCU, in contrast, has a more subdued, high-intensity atmosphere, with specialized staff and equipment for managing the most severe cases. The two units are separated by a transparent divider, allowing a clear visual comparison of the different levels of care and patient acuity. The scene is captured from an overhead angle, highlighting the contrast between the two spaces and the specialized nature of each unit.
Many people get confused about the difference between a Critical Care Unit (CCU) and an Intensive Care Unit (ICU). Both offer critical care, but they have different roles and names. It’s important to know the details.
Terminology Clarification: CCU and ICU
The term Critical Care Unit (CCU) can be confusing. It can mean a Cardiac Care Unit for heart patients or a general Critical Care Unit. But, ICU is widely known as a place for very sick patients needing constant care.
Functional Differences and Similarities
CCU and ICU both offer critical care, but they focus on different things. A Cardiac Care Unit deals mainly with heart issues. An ICU, on the other hand, treats many serious conditions. Both have top-notch equipment and teams ready to help.
Even though they differ, CCUs and ICUs share many things. They both:
- Watch patients closely and help keep them alive.
- Have teams with special training in critical care.
- Use the latest technology to help patients.
- Have more nurses to give each patient the best care.
In summary, CCUs and ICUs may have their own special areas, but they both play key roles in caring for very sick patients.
Types of Intensive Care Units in Modern Hospitals
A vast, modern hospital interior with specialized Intensive Care Units (ICUs) in the foreground. Pristine white walls, gleaming medical equipment, and sleek, futuristic-looking beds and machinery. Bright overhead lighting casts a sterile, clinical glow, creating an atmosphere of precision and advanced medical care. In the middle ground, doctors and nurses in scrubs and lab coats move purposefully between rooms, tending to critically ill patients. In the background, a network of corridors and nursing stations, hinting at the complex, interconnected nature of the hospital’s infrastructure. The overall scene conveys a sense of cutting-edge medical technology and the unwavering dedication of the staff to providing the highest level of intensive care.
Critical care has evolved, leading to specialized ICUs in hospitals. Medical technology advances and patient needs grow more complex. Now, hospitals have different ICU types to meet various patient needs.
Medical Intensive Care Units (MICU)
Medical Intensive Care Units (MICU) are for patients with severe medical issues. They need close monitoring and life-saving treatments. The MICU medical abbreviation is used in healthcare to refer to these units. MICUs have experts in critical care medicine, ready for emergencies like severe infections and heart crises.
Surgical Intensive Care Units (SICU)
Surgical Intensive Care Units (SICU) are for patients after major surgery. They need post-operative care that’s intensive. These units have advanced life-support systems and staff trained in surgical critical care. They help patients recover smoothly, bridging the gap between the operating room and the general ward.
Specialized ICUs and Their Functions
Hospitals also have specialized ICUs for specific patient groups. For example:
- Neonatal ICU (NICU): For critically ill newborns, including premature infants and those with congenital conditions.
- Pediatric ICU (PICU): For children needing intensive care, staffed by pediatric critical care experts.
- Cardiovascular ICU (CVICU): Focuses on patients with heart conditions, requiring close monitoring and intervention.
These specialized ICUs offer focused care. Patients get treatment from staff with the right expertise.
In conclusion, the variety in ICU types shows the complexity of modern healthcare. With MICU, SICU, and other specialized ICUs, hospitals can offer top-notch care to those who need it most.
The Cardiac Critical Care Unit (CCU): Purpose and Specialization
A modern, well-equipped cardiac care unit (CCU) filled with state-of-the-art medical equipment. The foreground features a team of dedicated healthcare professionals attentively monitoring patient vitals on sleek digital displays. The middle ground showcases the latest cardiac monitoring devices, including ECG machines and IV drips. In the background, the room is bathed in a calming, warm lighting that creates a serene atmosphere, complemented by the soft hues of the medical-grade walls and floors. The composition emphasizes the specialized nature of the CCU, designed to provide comprehensive, round-the-clock care for patients with critical cardiac conditions.
The Cardiac Critical Care Unit (CCU) is a special unit for patients with heart problems. It’s a key part of modern healthcare, giving intensive care to those with severe heart issues.
The CCU offers 24/7 care for serious heart issues. This includes heart attacks, irregular heartbeats, and problems after heart surgery. It has staff and tools made for heart patients’ needs.
Key Differences Between CCU and ICU
CCU and ICU both offer critical care, but they focus on different areas. An ICU is a general term for many critical care units. But a CCU is all about heart care.
Key differences include:
- Specialized staff trained in cardiology
- Equipment specific to cardiac monitoring and intervention
- Focused care protocols for cardiovascular conditions
Patient Criteria for CCU Admission
Patients go to the CCU for serious heart issues. They need close monitoring and intensive care. The criteria include:
- Acute myocardial infarction requiring close monitoring
- Post-cardiac surgery patients needing intensive care
- Severe arrhythmias or other life-threatening cardiac conditions
Understanding CCUs helps us see their vital role in caring for heart patients. They provide top-notch care for those with serious heart conditions.
Understanding CVICU Meaning and Its Role in Cardiovascular Care
A sterile, well-lit cardiovascular intensive care unit with modern medical equipment and monitors. In the foreground, a team of doctors and nurses in scrubs and face masks, intently focused on a critically ill patient lying on a hospital bed, various tubes and wires connected to their body. The middle ground showcases state-of-the-art technology, including an advanced cardiac monitor, IV pumps, and a ventilator. In the background, a window provides a view of a bustling hospital corridor, emphasizing the unit’s role as a central hub of cardiovascular care. The atmosphere is one of calm professionalism, with a palpable sense of urgency and dedication to providing the best possible treatment.
It’s key to know what CVICU stands for to understand its role in saving lives. CVICU stands for Cardiovascular Intensive Care Unit. It’s a special part of hospitals that takes care of patients with serious heart issues.
Cardiovascular Intensive Care Unit Explained
A Cardiovascular Intensive Care Unit (CVICU) is for patients with heart diseases. These units have the latest technology and a team of experts. The team includes cardiologists, surgeons, nurses, and more.
“The CVICU is a crucial part of healthcare today,” says a top cardiologist. “It offers focused care for heart patients. This care, with a team of experts and advanced tech, greatly improves patient results.”
Types of Patients Treated in CVICU
CVICUs help many patients with heart problems. These include:
- Those who have had heart surgery
- People with heart attacks
- Patients with severe heart failure needing close monitoring
- Those with complex heart rhythm problems
The care in CVICUs is very detailed. It includes watching patients closely, giving them life-saving treatments, and doing complex procedures. CVICUs are essential for saving lives and improving the lives of heart patients.
The Progressive Care Unit (PCU): Bridging the Gap
A modern, well-equipped Progressive Care Unit (PCU) with rows of state-of-the-art hospital beds and medical equipment. The room is bathed in warm, natural lighting filtering through large windows, creating a calm and soothing atmosphere. In the foreground, a team of attentive nurses and doctors tending to patients, their expressions focused and professional. The middle ground features various medical devices and monitors displaying vital signs. The background showcases a clean, organized layout with medical supplies and technology seamlessly integrated into the space. The overall scene conveys a sense of transitional care, bridging the gap between the intensity of the ICU and the more general ward.
The Progressive Care Unit (PCU) is a special area in hospitals. It helps patients who are moving from the ICU but aren’t ready for the general ward yet.
PCU Medical Abbreviation Explained
The PCU medical abbreviation means Progressive Care Unit. It’s a part of a hospital for patients needing more care than a general ward but not as much as an ICU.
The Step-Down Function of PCUs
PCUs act as a middle ground between ICUs and general wards. They are for patients who are:
- Getting better from big surgeries or serious illnesses
- Stable but still need to be watched closely
- Need more nursing care than general wards can offer
PCUs have advanced monitoring tools and staff ready for complex patient needs.
| Care Aspect | ICU | PCU | General Ward |
| Level of Care | Highly Intensive | Intermediate | Standard |
| Monitoring | Continuous | Close | Regular |
| Nurse-to-Patient Ratio | 1:1 or 1:2 | 1:3 or 1:4 | 1:5 or higher |
PCUs offer care that’s between ICU and general ward levels. They are key in improving patient results and using hospital resources well.
Severity Assessment: Which Unit Handles More Critical Patients?
Understanding a patient’s condition is key in critical care. Going to the ICU means a serious situation needs close watch and intense care.
Different hospital units have different levels of care. We’ll look at how these levels compare and the scoring systems used to measure patient severity.
Comparing Acuity Levels Across Different Units
Hospital units vary in care levels, from ICUs to general wards. ICUs are for patients needing constant, intense care. PCUs offer a step-down care for those moving from ICU but still need more than a general ward.
ICUs handle more critical cases. They deal with patients on life support, needing strong medications, and facing organ failures. PCUs, on the other hand, care for patients who are less sick but still need more watch than a general ward.
| Unit Type | Acuity Level | Typical Patient Conditions |
| ICU | High | Life-threatening conditions, multi-organ failure |
| PCU | Moderate to High | Step-down care, post-ICU recovery, less critical conditions |
| General Ward | Low to Moderate | Stable patients, post-operative recovery, less intensive care needs |
The APACHE and SOFA Scoring Systems
Healthcare uses scoring systems to measure patient severity and predict outcomes. The APACHE and SOFA systems are two common ones.
The APACHE scoring system looks at several factors like temperature, blood pressure, and lab results. It also considers chronic health conditions. This score helps predict hospital death rates and sorts patients by how sick they are.
The SOFA scoring system checks organ function or failure in six areas: respiratory, cardiovascular, hepatic, coagulation, renal, and neurological. It’s great for tracking organ failure and predicting death in critical patients.
Both scoring systems are crucial in ICUs. They help doctors make better care plans and use resources wisely. By knowing how sick a patient is, doctors can improve treatment and outcomes.
Staffing and Resources: What Makes ICUs Unique
ICUs stand out because they offer specialized care with expert staff and top-notch equipment. This mix of human skill and tech is key to handling critical cases.
Nurse-to-Patient Ratios in Critical Care
ICUs are known for their strict nurse-to-patient ratios. Nurses usually watch over just one or two patients. This 1:1 or 1:2 nurse-to-patient ratio ensures each patient gets the care they need.
Keeping these ratios is vital for several reasons:
- It lets nurses closely watch patients and act fast if needed.
- It helps in making care plans that fit each patient’s needs.
- It makes patients safer by cutting down on treatment mistakes.
Specialized Equipment and Technology
ICUs also use advanced medical equipment and technology. These tools help doctors and nurses keep an eye on patients’ health, support failing organs, and manage complex systems.
Some important technologies and equipment in ICUs include:
- Ventilators and other respiratory support devices.
- Cardiac monitors and life-support systems.
- Dialysis equipment for patients with acute kidney injury.
- Advanced imaging technologies, such as portable X-ray and ultrasound machines.
By combining skilled staff with these advanced tools, ICUs can give the best care to critically ill patients.
ICU Admission Criteria: When Is Intensive Care Necessary?
Deciding to put a patient in the ICU is crucial. We look at how sick the patient is, if they need constant watching, and if they might need special treatments to live.
Medical Conditions Requiring ICU Care
Patients go to the ICU if they need a lot of care and watching. This includes:
- Severe breathing problems that need a machine to breathe
- Heart issues that need special medicines
- Needs care after big surgeries
- Has serious injuries from trauma
- Has sepsis or septic shock
The ICU has special tools and a team ready for critical care. They can handle more than a regular ward can.
The Decision-Making Process for ICU Transfer
Choosing to move a patient to the ICU is a big decision. We check if they really need the ICU’s care. The steps are:
- First, the primary team checks the patient.
- Then, ICU experts give their opinion.
- We look at how sick the patient is and if they might get worse.
- We also think about what the patient and their family want.
This careful process makes sure patients get the right care when they need it. Knowing when to send someone to the ICU helps us in critical care.
The Patient Experience in an ICU Setting
The ICU experience is complex and challenging for patients and families. It involves advanced medical care and emotional support. Understanding the psychological and emotional aspects is key.
Psychological Impact of ICU Stays
Patients in ICUs face big psychological challenges like anxiety and confusion. The ICU’s busy environment can be overwhelming. The mental impact of an ICU stay is as important as the physical reason for admission.
Research shows emotional support improves ICU outcomes. Support comes from family, healthcare, and ICU design.
Family Involvement and Visitation Policies
Family involvement is vital in the ICU. Visitation rules differ by hospital but most allow family visits. Visitors are usually immediate family, and only a few are allowed at once.
| Visitation Aspect | Typical ICU Policy |
| Visitor Limitation | 1-2 visitors at a time |
| Visitation Hours | Flexible, but often restricted |
| Family Support | Available through hospital staff |
Many hospitals now have more flexible visitation policies. They see family presence as key to recovery and emotional health.
ICU Terminology: Understanding the Medical Language
Learning ICU terminology is key for anyone in critical care. This includes patients, family members, and healthcare workers. The ICU is a place where doctors and nurses use special words to talk about patient care.
Knowing these terms helps you understand the ICU better. We’ll look at common ICU acronyms and how to read medical charts. This way, patients and families can make better care choices.
Common ICU Acronyms and Their Meanings
ICU staff use many acronyms to talk about patient health and treatments. Knowing these can make you feel less worried and help you talk better with doctors. Here are some examples:
- APACHE II: Acute Physiology and Chronic Health Evaluation II, a way to measure how sick a patient is.
- SOFA: Sequential Organ Failure Assessment, tracks a patient’s organ function or failure in the ICU.
- CVVH: Continuous Veno-Venous Hemofiltration, a treatment for acute kidney injury.
- ECMO: Extracorporeal Membrane Oxygenation, a therapy for heart and lung failure.
Knowing these acronyms can give you insight into a patient’s health and treatment. Always ask doctors to explain any terms you don’t get.
Interpreting ICU Medical Charts and Reports
ICU charts and reports have important info on a patient’s health and treatment. They use a lot of medical terms and abbreviations. This can be hard to understand without help.
| Term | Meaning |
| BP | Blood Pressure |
| HR | Heart Rate |
| RR | Respiratory Rate |
| SpO2 | Peripheral Oxygen Saturation |
Critical Care During the COVID-19 Pandemic: Lessons Learned
The COVID-19 pandemic was a huge challenge for intensive care units (ICUs) around the world. ICUs had to handle a lot of sick patients, making things very tough. We look at how ICUs changed their ways to deal with this crisis.
Adapting to Crisis Situations
ICUs had to quickly get ready for more COVID-19 patients. They had to make more ICU beds by using different areas. This included turning operating rooms and recovery rooms into ICU spaces.
They also changed how they staffed ICUs. This meant moving staff around to help with the extra work. Being flexible was key to handling the sudden need for more care.
The pandemic showed how important teamwork is in ICUs. Teams worked together to create new rules and share knowledge. This teamwork was crucial in facing the challenges of COVID-19.
Changes in Critical Care Protocols and Procedures
The pandemic led to big changes in how ICUs work. One big change was using prone positioning for patients with severe breathing problems. This helped them breathe better.
ICUs also started using remote monitoring more. This let them keep an eye on patients without going into their rooms. It helped keep everyone safer from infection.
ICUs also got stricter about stopping the spread of COVID-19. They used more protective gear and limited visitors. These steps were key in keeping the virus out of ICUs.
There was also a bigger focus on palliative care. This made sure patients got care that helped with their physical, emotional, and social needs.
Looking back, ICUs were very important in fighting the pandemic. The changes they made will help them better in the future.
The Future of Intensive Care: Trends and Innovations
Intensive care units (ICUs) are on the verge of a big change. This change comes from new technology and better care models. These advancements will make ICUs better for patients and more efficient for care.
Technological Advancements in Critical Care
New technology is key to the future of ICUs. Some important changes include:
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML help predict when patients might get worse. They also help make treatment plans better.
- Telemedicine: This lets doctors check on patients from far away. It’s great for areas that don’t have enough doctors.
- Advanced Monitoring Systems: New systems give doctors real-time data. This helps them make quick, smart choices.
- Personalized Medicine: Doctors use genetic and biomarker data to make treatments just right for each patient. This could lead to better results.
Evolving Models of ICU Care Delivery
ICU care is also changing in big ways. Some of these changes are:
- Family-Centered Care: ICUs are now more open to families. They know how important family is in helping patients get better.
- Multidisciplinary Teams: ICU teams are getting bigger. They now include more specialists, making care more complete.
- Flexible Care Models: ICUs are moving towards more flexible care. This means they can change to meet different patient and system needs.
- Post-ICU Care: There’s a growing focus on care after the ICU. Programs are being set up to help patients after they leave.
These changes and trends will make ICUs more focused on patients, efficient, and effective. As we keep moving forward, we’ll see big improvements in how well ICUs care for patients.
Conclusion: Navigating the Complex World of Critical Care
It’s key to know the differences between various critical care units. This ensures patients get the right care. The terms Critical Care Unit and ICU are often mixed up. But they cover a wide range of care in hospitals.
The icu care concept focuses on intensive monitoring and life-saving treatments for very sick patients. Understanding critical care helps us see the importance and complexity of these units. This includes knowing the roles of different ICUs and their staff, resources, and who gets admitted.
As healthcare keeps changing, it’s important to stay up-to-date on critical care. This knowledge improves patient care. It also helps families and healthcare workers make better decisions.
FAQ
What does ICU stand for?
ICU stands for Intensive Care Unit. It’s a special part of hospitals for very sick patients.
What is the difference between a Critical Care Unit and an ICU?
Critical Care Units and ICUs both care for very sick patients. But, they might focus on different things depending on the hospital.
What is the role of a Cardiac Critical Care Unit (CCU)?
A Cardiac Critical Care Unit (CCU) cares for patients with heart problems. They watch them closely and treat them.
What does CVICU mean?
CVICU stands for Cardiovascular Intensive Care Unit. It’s for patients with heart and blood vessel issues, including after surgery.
What is a Progressive Care Unit (PCU)?
A Progressive Care Unit (PCU) is for patients who need more care than a regular ward but not as much as an ICU.
How do ICUs assess patient severity?
ICUs use scores like APACHE and SOFA to see how sick a patient is. This helps decide how much care they need.
What makes ICUs unique in terms of staffing and resources?
ICUs have very skilled doctors and nurses. They also have special equipment and technology for intensive care.
What are the criteria for ICU admission?
Patients go to the ICU if they’re very sick. They need close watching and treatments to keep them alive.
How do ICUs support family involvement?
ICUs let families visit and support their loved ones. They give updates on the patient’s condition.
What are some common ICU acronyms?
Common ICU acronyms include MICU (Medical Intensive Care Unit), SICU (Surgical Intensive Care Unit), and CVICU (Cardiovascular Intensive Care Unit).
How have ICUs adapted to crisis situations like the COVID-19 pandemic?
ICUs have changed their ways during crises. They plan for more patients, adjust staff, and focus on keeping everyone safe.
What are the future trends and innovations in ICU care?
The future of ICU care will bring new tech like telemedicine and artificial intelligence. It will also focus more on what patients want.
References
National Center for Biotechnology Information. Critical care unit nomenclature and ICU equivalence. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20648089/