Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know that patients with severe brain injuries or illnesses need special care? Neurocritical care is a unique field for those with life-threatening brain and brain surgery conditions.
Understanding intensive care can be tough. It’s key to know the difference between neurocritical care and regular ICU. Neuro ICUs have the latest technology and teams ready for brain and brain surgery patients.
Neurocritical care focuses on specialized treatment for severe brain injuries or illnesses. Knowing the difference helps patients and families get the right care.
Key Takeaways
- Neurocritical care is a specialized form of intensive care for patients with severe neurological and neurosurgical conditions.
- Neuro ICUs are equipped with advanced technology and staffed by trained multidisciplinary teams.
- The care provided in neuro ICUs differs significantly from traditional ICU treatment.
- Understanding the differences between neurocritical care and traditional ICU is crucial for navigating the healthcare system.
- Neurocritical care addresses the unique needs of patients with severe brain injuries or illnesses.
Understanding Traditional ICU Care
A brightly lit, high-contrast hospital room with modern medical equipment and technology. In the foreground, a hospital bed with a patient receiving attentive care from a team of nurses and doctors, their faces focused and determined. The middle ground features a variety of medical devices and monitors, their screens displaying vital signs and other crucial data. In the background, a panoramic window overlooking a bustling city skyline, conveying a sense of the patient’s connection to the outside world despite their critical condition. The overall mood is one of professionalism, urgency, and the unwavering dedication of the medical staff to providing the highest level of care.
Intensive Care Units (ICUs) are special parts of hospitals for very sick patients. They need close watch and treatments to keep them alive. ICUs have the latest technology and teams ready for many serious health issues.
Definition and Purpose of General ICU
A general ICU gives full care to very sick patients, no matter their illness. Its main job is to keep patients alive with treatments and watch them closely. This is for patients at high risk of dying or whose health can get worse fast.
Types of Patients Treated in Traditional ICUs
ICUs help many kinds of patients, like those with breathing problems, serious infections, or injuries. They also help after surgery or with other serious health issues. These patients might need help breathing, blood pressure support, and other treatments to live.
Standard Equipment and Monitoring in ICUs
ICUs have lots of advanced tools and devices for care. You’ll find heart monitors, machines to help breathing, and pumps for medicine. These tools help doctors and nurses catch problems early and act fast.
Equipment | Purpose | Patient Benefit |
Cardiac Monitors | Continuous monitoring of heart rate and rhythm | Early detection of cardiac complications |
Mechanical Ventilators | Support for patients with respiratory failure | Assistance with breathing, reducing respiratory distress |
Hemodynamic Monitoring Systems | Monitoring of blood pressure and cardiac output | Guiding fluid and vasopressor therapy to maintain optimal blood pressure |
What is Neuro ICU and How Does It Differ?
A modern, well-equipped neuro ICU ward with high-tech medical equipment, monitoring devices, and specialized staff tending to critically ill neurological patients. The scene is bathed in a soft, warm lighting, creating a serene, calming atmosphere. In the foreground, we see an array of state-of-the-art medical devices, such as ventilators, IV pumps, and EEG machines. In the middle ground, a team of dedicated nurses and physicians are carefully monitoring patient vitals and administering specialized treatments. In the background, we glimpse the calm, soothing ambiance of the ward, with muted colors and subtle architectural details. The overall impression is one of a highly specialized, technologically advanced, and compassionate environment dedicated to the care of critically ill neurological patients.
Neuro ICUs are special intensive care units for patients with serious brain issues. They use advanced tools and treatments to care for these patients.
Definition and Specialized Focus of Neurointensive Care
Neurointensive care deals with severe brain illnesses or injuries. Neuro ICUs have a team of experts ready to handle these cases. They handle things like brain injuries, strokes, and more.
This care goes beyond just treating the brain issue. It also looks after other health problems that might arise. This all-around approach helps patients get better.
History and Development of Neurocritical Care
Neurocritical care has grown a lot in recent years. This is thanks to new medical tech, understanding brain diseases better, and new treatments. Dedicated neuro ICUs have been key in this growth.
As we learn more about brain care, the care in neuro ICUs gets better too. This means patients get even better treatment and care.
The Growing Importance of Specialized Neurological Care
Specialized brain care is more important than ever. More people are getting brain injuries or strokes. Neuro ICUs are crucial in helping these patients.
We can expect even more progress in neuro ICU care. This will lead to even better results for those with complex brain conditions.
Key Differences Between Neurocritical Care and General ICU
A well-lit neurocritical care unit, equipped with state-of-the-art medical devices. In the foreground, a mechanical ventilator, its intricate controls and displays illuminated, stands ready to support a patient’s breathing. Surrounding it, a tangle of tubes, wires, and monitors capturing vital signs – heart rate, blood pressure, oxygen levels. In the middle ground, a high-tech bedside console, its touchscreen interface enabling precise monitoring and adjustment of medication and therapies. In the background, the clean, clinical environment is punctuated by the occasional flashing indicator light, creating a sense of focused intensity. The overall atmosphere conveys the specialized, technology-driven nature of neurocritical care, distinct from a general intensive care unit.
Neuro ICUs focus on the unique needs of brain health, unlike regular ICUs. They offer specialized care for patients with brain conditions. This care is more detailed and tailored to their specific needs.
Specialized Equipment and Monitoring Systems
Neuro ICUs use specialized equipment for brain patients. They have advanced tools like:
- Intracranial pressure monitors
- Brain tissue oxygen monitors
- Continuous EEG monitoring systems
These tools help doctors keep a close eye on brain health. They can act quickly if needed.
Staff Training and Expertise Requirements
Staff in neuro ICUs get rigorous training for brain care. They learn:
Staff Member | Specialized Training |
Neurointensivists | Advanced training in neurocritical care |
Nursing Staff | Certification in neurocritical care nursing |
Rehabilitation Therapists | Experience in neurological rehabilitation |
A leading expert says, “Brain care needs a skilled team.”
“Caring for brain patients needs advanced tech and deep knowledge of brain health.”
Treatment Protocols and Approaches
Neuro ICUs use specialized treatment protocols for brain patients. These plans help manage brain pressure and prevent further damage.
Physical Environment and Unit Design
Neuro ICUs are designed differently than regular ICUs. They focus on supporting brain care needs. This includes:
- Private rooms to reduce infection and help patients rest
- Advanced life-support systems in the room
- Areas for family visits
Neuro ICUs offer better care with their equipment, trained staff, and tailored plans. They also have a supportive environment for patients.
Types of Patients Treated in Neurocritical Care Units
A high-contrast, cinematic scene of a Neuro ICU ward, bathed in the warm glow of medical lighting. In the foreground, patients lie still in their beds, hooked up to a tangle of tubes and wires, monitors displaying vital signs. The middle ground features the attentive medical team, clad in scrubs and lab coats, closely observing the patients. In the background, a haze of diagnostic equipment and the hushed, focused atmosphere of the intensive care unit. The scene conveys the gravity and importance of neurocritical care, the delicate balance between life and death, and the unwavering dedication of the medical professionals.
Neurocritical Care Units treat many complex neurological conditions. These units offer intensive care for life-threatening injuries or illnesses. They are designed to closely monitor and treat patients.
Traumatic Brain Injury Patients
Traumatic brain injuries (TBI) are common in Neuro ICUs. These injuries can happen from accidents, falls, or violence. Prompt and specialized care is key to prevent more damage and help recovery.
Stroke and Cerebrovascular Conditions
Stroke patients, including those with ischemic or hemorrhagic strokes, are also treated here. Timely intervention is vital to reduce brain damage and improve outcomes. Neuro ICUs have the tools and staff to manage stroke patients’ complex needs.
Neurosurgical Recovery Cases
Patients after neurosurgery need close monitoring. Neuro ICUs provide the care needed for these patients. They manage complications and support recovery, thanks to their specialized staff.
Neurological Disorders Requiring Intensive Care
Neurocritical Care Units also treat severe neurological disorders. Conditions like status epilepticus, meningitis, or encephalitis need intensive monitoring and treatment. This care helps prevent long-term damage and improves patient outcomes.
The Neurocritical Care Team Structure
A team of highly skilled medical professionals standing in a well-lit, modern hospital ward, wearing crisp white coats and engaged in intense discussion. In the foreground, a neurosurgeon and critical care nurse review patient charts, their expressions focused and determined. In the middle ground, a neurologist and respiratory therapist collaborate at a computer terminal, analyzing vital signs and test results. The background is filled with state-of-the-art medical equipment, creating a sense of cutting-edge technology and expertise. The overall atmosphere is one of professionalism, collaboration, and a steadfast commitment to providing exceptional neurocritical care.
Effective neurocritical care comes from a team of experts. They work together to handle complex neurological issues. This team includes many professionals from different fields.
Neurointensivists and Their Role
Neurointensivists are doctors who focus on critical care of the brain. They make important decisions for patients with severe brain injuries or strokes. Their skills are crucial for managing these conditions.
Key responsibilities of neurointensivists include:
- Assessing and managing intracranial pressure
- Overseeing the use of advanced monitoring techniques
- Coordinating with other specialists to develop comprehensive care plans
Specialized Nursing Staff in Neuro ICU
Specialized nurses are vital in the neuro ICU. They have advanced training in caring for brain injuries. They work with neurointensivists to watch over patients, give medicine, and provide top-notch care.
The role of specialized nurses includes:
- Continuous monitoring of patients’ neurological status
- Administering and managing complex medication regimens
- Providing emotional support to patients and their families
Multidisciplinary Support Team Members
A team of specialists is key in the neuro ICU. This team includes neurosurgeons, neurologists, and more. They work together to create care plans for each patient.
The support team members play crucial roles in:
- Providing surgical interventions when necessary
- Offering rehabilitation services to aid in recovery
- Ensuring optimal medication management
Together, the neurocritical care team gives patients the best care. This improves their outcomes and quality of life.
Advanced Monitoring Techniques in Neurointensive Care
A sleek, state-of-the-art neuromonitoring station in a dimly lit neurocritical care unit. In the foreground, a bank of high-resolution displays showcases real-time data from advanced brain imaging and electrical activity sensors. The middle ground features various probes, catheters, and monitoring devices neatly arranged, conveying a sense of precision and clinical expertise. The background depicts the softly lit, high-tech environment of the intensive care setting, with subtle hints of medical equipment and the occasional movement of medical personnel. The overall mood is one of cutting-edge technology, meticulous care, and the unwavering dedication to providing the best possible outcomes for critically ill neurological patients.
In neurointensive care, advanced monitoring is key. It helps doctors watch patients closely and make quick decisions. This care is vital for those with severe brain injuries.
Intracranial Pressure Monitoring
Intracranial pressure (ICP) monitoring is crucial. It’s used for patients with brain injuries or swelling. It lets doctors see pressure changes fast and act to prevent more damage.
Benefits of ICP Monitoring:
- Early detection of increased ICP
- Guided management of cerebral perfusion pressure
- Optimization of treatment strategies
Brain Tissue Oxygen Monitoring
Brain tissue oxygen monitoring is another important tool. It checks oxygen levels in the brain. This gives insights into brain health.
This monitoring is key because it spots brain oxygen problems early. This allows for quick actions to help patients.
Monitoring Technique | Purpose | Benefits |
Intracranial Pressure Monitoring | Measure ICP to guide management | Early detection of increased ICP, optimized treatment |
Brain Tissue Oxygen Monitoring | Assess cerebral oxygenation | Detection of cerebral hypoxia, improved outcomes |
Continuous EEG Monitoring | Monitor brain activity continuously | Detection of seizures, assessment of neurological status |
Continuous EEG Monitoring
Continuous EEG monitoring watches brain activity all the time. It’s great for catching seizures and checking on patients.
Advantages of Continuous EEG Monitoring:
- Early detection of non-convulsive seizures
- Continuous assessment of neurological function
- Guidance for therapeutic interventions
Advanced Neuroimaging in Critical Care
Neuroimaging like MRI and CT scans are vital in the ICU. They show detailed brain pictures. This helps doctors plan the best treatment.
Using these advanced tools, ICUs can greatly improve care. Monitoring ICP, brain oxygen, EEG, and imaging together helps doctors give the best care.
Specialized Brain Trauma Care in the Neuro ICU
A well-lit modern neuro ICU room, with a patient undergoing advanced brain trauma rehabilitation. In the foreground, a physiotherapist guides the patient through precise exercises, their limbs gently moving as cutting-edge monitoring equipment tracks progress. In the middle ground, a team of neurologists and nurses monitor vital signs, adjusting equipment as needed. In the background, large windows offer a calming view of a serene hospital garden, natural light filtering in. The atmosphere is one of focused care and quiet determination, as the medical team works to restore the patient’s cognitive and motor functions.
Traumatic brain injury management in Neuro ICUs is complex. It involves many medical specialties. We focus on acute management and preventing secondary brain injury in our care.
Acute Management of Traumatic Brain Injuries
The acute management of traumatic brain injuries is urgent. It aims to stabilize the patient and prevent further injury. This includes:
- Rapid assessment and diagnosis
- Stabilization of vital signs
- Surgical interventions when necessary
A study in the Journal of Neurotrauma highlights the importance of early intervention. It says it improves outcomes for traumatic brain injury patients.
“The initial management of traumatic brain injury is crucial in determining patient outcomes.”
Journal of Neurotrauma
Preventing Secondary Brain Injury
Preventing secondary brain injury is key in Neuro ICUs. Strategies include:
Strategy | Description |
Monitoring Intracranial Pressure | Continuous monitoring to detect and manage elevated ICP |
Cerebral Perfusion Management | Ensuring adequate blood flow to the brain |
Neuroprotective Measures | Implementing measures to protect the brain from further injury |
Rehabilitation Initiation in Critical Care
Rehabilitation starts early in the Neuro ICU. It aims to optimize recovery. A team of physical, occupational, and speech therapists work together.
Long-term Outcome Considerations
Long-term outcomes for traumatic brain injury patients depend on several factors. These include the injury’s severity and the quality of care. We consider these when planning treatment, aiming for the best recovery and quality of life.
The Brain Trauma Foundation emphasizes the importance of guidelines. They say they are crucial for improving patient outcomes.
“The management of severe traumatic brain injury requires a comprehensive and multidisciplinary approach.”
Brain Trauma Foundation
When is a Neurosurgical Intensive Care Unit Necessary?
A neurosurgical intensive care unit (NICU) is key for patients with complex neurosurgery needs. It offers specialized care tailored to their unique needs, aiming for the best results.
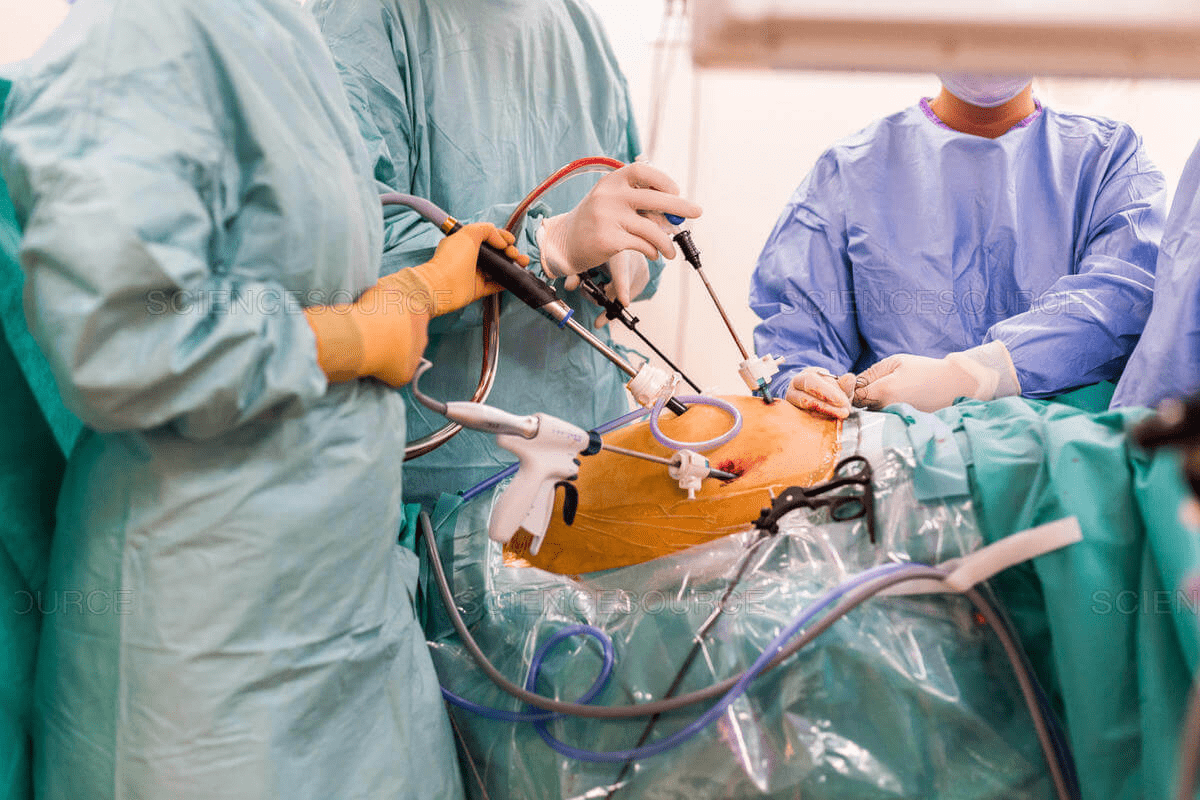
Pre and Post-Operative Neurosurgical Care
Patients needing pre and post-operative care for neurosurgery often go to an NICU. This includes surgeries like tumor removals, aneurysm clipping, or spinal operations. They need close monitoring and intensive care before and after surgery.
In the NICU, pre-operative care prepares the patient for surgery. This includes managing pressure in the brain and improving blood flow to the brain. It also addresses critical neurological issues.
Post-operative care in the NICU focuses on watching for complications and managing pain. The team is ready to handle any issues that come up, ensuring the best recovery.
Complex Neurological Emergencies
Severe brain injuries, strokes, or seizures also need an NICU. These emergencies require quick and specialized care to prevent more damage and improve outcomes.
The NICU has advanced tools and staff with neurocritical care expertise. They closely monitor vital signs and brain function, providing the needed care.
Transfer Criteria from General ICU to Neuro ICU
Deciding when to move a patient from a general ICU to an NICU is important. It depends on the patient’s neurological needs and the care they require.
Criteria | Description |
Complex Neurosurgical Conditions | Patients needing care for complex neurosurgical conditions, such as post-operative care for brain tumors or aneurysms. |
Severe Neurological Injury | Patients with severe traumatic brain injuries or spinal cord injuries requiring intensive neurological care. |
Need for Advanced Neurological Monitoring | Patients requiring advanced monitoring techniques such as intracranial pressure monitoring or continuous EEG. |
Transferring patients to an NICU when needed ensures they get the specialized care they need. This can lead to better outcomes.
Patient and Family Experience in Neuro ICU
In the Neuro ICU, we treat critical neurological conditions and support patients and families. The environment is specialized, focusing on top-notch care for both medical and emotional needs.
Unique Challenges for Families of Neurological Patients
Families of patients in Neuro ICU face unique challenges. They must cope with uncertainty and navigate a complex medical environment. Emotional support is key, and our team is committed to providing it.
The emotional journey can be tough, with feelings of anxiety, fear, and hope. We believe in family-centered care. We keep families informed and involved in the care process.
Communication Strategies with Unconscious Patients
Communicating with unconscious patients is complex. We believe they can still hear and benefit from therapeutic communication. Our staff uses various strategies, including speaking, playing music, and gentle touch.
- Speaking in a calm and reassuring tone
- Encouraging family members to communicate with their loved ones
- Using non-verbal communication techniques
Support Systems and Resources
Support for families is crucial in the Neuro ICU. We offer counseling services, support groups, and educational materials. These help families during this challenging time.
Support Service | Description |
Counseling Services | Individual and family counseling to cope with the stress and emotional impact of critical illness |
Support Groups | Regular meetings for families to share experiences and find support among peers |
Educational Resources | Information and guidance on caring for loved ones, understanding their condition, and navigating the healthcare system |
Transitioning from Neuro ICU to Step-Down Units
Transitioning a patient from the Neuro ICU to a step-down unit is a big step in their recovery. We explain the changes in care level and what to expect. This helps families prepare.
Our team provides comprehensive care in the step-down unit. We focus on continued recovery and rehabilitation. We support families and patients through this transition.
Outcomes and Benefits of Specialized Neurocritical Care
Specialized neurocritical care has changed how we treat very sick brain patients. It leads to better lives for them. We must keep learning about the good things these units do.
Impact on Patient Survival Rates
Neurocritical care greatly helps patients live longer. Studies show that patients in neuro ICUs live longer than those in regular ICUs. This is thanks to the special care and watchful eyes of neurointensivists.
A study in the Journal of Neurosurgery found that a neurocritical care program cut down deaths in severe brain injury patients. 1 This shows how crucial specialized care is.
Neurological Recovery Outcomes
Neurocritical care also boosts how well patients recover. It helps avoid more brain damage and helps patients get better faster.
Research shows that patients in neuro ICUs do better. They have better thinking skills and less disability. 2 This is key for those with stroke, brain injury, and urgent neurosurgery.
Condition | General ICU Care | Neuro ICU Care |
Traumatic Brain Injury | Higher mortality rates | Improved survival and recovery |
Stroke | Limited specialized care | Targeted interventions for better outcomes |
Neurosurgical Emergencies | Variable care quality | Specialized post-operative care |
Cost-Effectiveness of Specialized Units
Starting a neuro ICU might seem expensive at first. But, these units save money in the long run. They help patients stay in the hospital less, avoid more problems, and get better faster.
A study on the cost of neuro ICUs found they save a lot of money. This is because they reduce the need for long-term care and help patients recover faster. 3
Establishing Dedicated Neuro ICU Facilities
Creating a Neuro ICU needs a detailed plan, including hospital needs and certification steps. We understand the challenge of setting up these units. They are key for top-notch care of neurological patients.
Hospital Requirements and Considerations
Hospitals have to think about several important things when starting a Neuro ICU. First, they need to check their current setup to see if it can handle the special equipment and monitoring needed. This means looking at space, staff, and the chance to add new tech.
It’s also crucial to have a team of experts, like neurointensivists and specialized nurses. Their training is key for the high care level needed in a Neuro ICU.
Resource Allocation and Planning
Planning how to use resources is a big part of starting a Neuro ICU. This includes money, physical things like beds, and people like staff and trainers. Good planning makes sure the Neuro ICU can meet the complex needs of neurological patients, like brain injuries and stroke recovery.
Good planning also means setting up systems for watching over patients closely. This includes checking things like brain pressure and brain oxygen levels. These tools are vital for the care needed in a Neuro ICU.
Certification and Accreditation Processes
To make sure a Neuro ICU is top-notch, it must go through certification and accreditation. These steps check the unit’s setup, staff, and care methods to make sure they meet standards.
Getting certified by known groups boosts the Neuro ICU’s reputation. It also means the unit is ready to give patients the best care possible. We stress how important these steps are for keeping care quality high in Neuro ICUs.
Neurocritical Care Jobs and Career Opportunities
Working in neurocritical care is both rewarding and challenging. It’s a field where healthcare professionals can make a big difference. The demand for skilled workers is growing fast.
Education and Training Requirements
To work in neurocritical care, you need special education and training. Doctors must complete a residency in neurology, neurosurgery, or anesthesiology. Then, they get fellowship training in neurocritical care.
Nurses and other healthcare workers also need special training. They start with basic critical care education. Then, they get certifications or courses in neurocritical care.
It’s key to keep learning in this field. Professionals must stay up-to-date with new techniques and research. This helps them give the best care to their patients.
Physician Roles and Specialization Paths
Physicians are vital in neurocritical care teams. Neurointensivists manage care for critically ill neurological patients. They work with neurosurgeons and other specialists to plan treatments.
Becoming a neurointensivist requires hard work and dedication. Doctors must finish medical school, then a residency. They often do fellowship training in neurocritical care or a related field.
Nursing and Allied Health Positions
Nurses and allied health workers are crucial in neurocritical care units. They care for patients 24/7, monitor their health, and help with treatment plans. Nurses get special training and often get certifications like CCRN or PCCN.
Allied health professionals, like respiratory therapists and physical therapists, are also key. They help with the comprehensive care of neurocritical patients.
Job Outlook and Compensation
The job outlook for neurocritical care is good. The demand for specialized neurological care is increasing. This is because more people are getting neurological conditions as they age.Salaries for neurocritical care professionals vary. They depend on location, experience, and role. But, these jobs are well-paid. This shows the high demand for their skills.
Conclusion
Neurocritical care is a special field of intensive care that’s different from regular ICU care. The summary of neuro ICU shows its key role in handling complex brain conditions. It needs advanced tools, skilled staff, and specific treatment plans.
We’ve seen how neuro ICUs help patients, especially those with brain injuries, strokes, or after neurosurgery. The neurocritical care conclusion is clear: these units are crucial in today’s healthcare. They offer detailed and effective care.
Knowing the difference between neurocritical care and general ICU helps everyone. It shows the importance of specialized brain care. As neuro ICUs grow, they will lead in improving patient care and results.
FAQ
What is the primary difference between a Neuro ICU and a traditional ICU?
Neuro ICUs focus on patients with severe brain injuries. They use special equipment not found in regular ICUs. This is because they deal with acute neurological conditions.
What kind of patients are treated in a Neuro ICU?
Neuro ICUs care for patients with brain injuries, strokes, and other brain disorders. They also help those recovering from brain surgery.
What advanced monitoring techniques are used in Neuro ICUs?
Neuro ICUs use high-tech tools like monitoring brain pressure and oxygen levels. They also do continuous EEG and advanced brain scans.
How does the staff in a Neuro ICU differ from that in a traditional ICU?
Neuro ICU teams have neurointensivists and nurses trained in brain care. They work with a team focused on brain health. This is different from the general care teams in regular ICUs.
When is a Neurosurgical Intensive Care Unit necessary?
Neurosurgical ICUs are needed for patients before and after brain surgery. They also care for complex brain emergencies. This is often after a patient is moved from a regular ICU.
What are the benefits of specialized Neurocritical Care?
Specialized care in Neuro ICUs leads to better survival rates and recovery. It also improves quality of life and is cost-effective for managing brain conditions.
What is the role of a neurointensivist in a Neuro ICU?
Neurointensivists are doctors with brain care training. They manage patients with brain injuries, diagnose, treat, and plan for recovery.
How do Neuro ICUs support families of patients?
Neuro ICUs offer support and resources for families. They help with communication, counseling, and guidance through treatment and recovery.
What are the requirements for establishing a dedicated Neuro ICU?
To start a Neuro ICU, hospitals need special equipment and trained staff. They also need the right unit design. Plus, they must get certified and accredited.
What career opportunities are available in Neurocritical Care?
There are many jobs in Neurocritical Care, like neurocritical care doctors and nurses. These roles have a good outlook and pay well.
What is the significance of intracranial pressure monitoring in Neuro ICUs?
Monitoring brain pressure is key in Neuro ICUs. It helps catch and manage high pressure early. This prevents further brain damage.
References
National Center for Biotechnology Information. Neurocritical care versus general intensive care understanding the difference. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21519958/