Last Updated on December 1, 2025 by Bilal Hasdemir
types of icu
Did you know that Intensive Care Units (ICUs) are a big part of hospital care? Studies show that almost 1 in 5 patients need specialized care in ICUs because of serious illnesses or injuries. Discover the 4 main types of ICU. This ultimate guide explains the difference between NICU, PICU, SICU, and MICU.
ICUs are special hospital areas that give intensive care. They watch patients very closely who are in a bad shape. Finding out about the intensive care unit types can be hard, especially when you’re looking for medical help for yourself or a family member.
Big hospitals have different ICUs for different needs. For example, there are ICUs for kids, newborns, surgery, and heart care. In this article, we’ll look at the different icu levels and what they offer.
Key Takeaways
- ICUs provide specialized care for critically ill patients.
- Different ICUs cater to specific patient needs, such as pediatric or cardiac care.
- Large hospitals often have multiple ICUs with varying levels of care.
- Understanding the different types of ICUs can help patients and families make informed decisions.
- ICUs require close and constant monitoring of patients.
Understanding the Intensive Care Unit (ICU)
A dimly lit intensive care unit, its sterile environment illuminated by the soft glow of medical equipment. In the foreground, a patient lies unconscious, surrounded by a tangle of tubes and wires monitoring their vital signs. Nurses and doctors in scrubs move with precision, their faces shielded by surgical masks. The middle ground features an array of high-tech machines and monitors, their screens displaying real-time data. In the background, the shadowy silhouettes of other beds suggest the scale and complexity of the ICU. The atmosphere is one of tense concentration, the air heavy with the weight of critical care.
Intensive Care Units (ICUs) are key in modern healthcare. They give critical care to patients who need close watching and life-saving treatments. ICUs are vital in hospitals, handling the most serious cases.
Definition and Purpose of ICUs
ICUs are known for their high-level care for critically ill patients. Their main goal is to offer a controlled setting for constant care from experts. This includes advanced patient monitoring and life-supporting equipment.
“The ICU is a crucial part of any hospital,” says a healthcare expert. “It combines technology, expertise, and care to save lives.”
In ICUs, care is tailored to each patient’s needs. A team of healthcare professionals works together. They use state-of-the-art equipment and treatments to help patients.
Historical Development of ICUs
ICUs have changed a lot over time. At first, they were just recovery rooms for patients after surgery. But as medical tech improved, ICUs became more advanced.
Now, ICUs have the latest technology. This includes advanced ventilators, cardiac monitors, and dialysis machines. The growth of ICUs shows how critical care has evolved. It shows how important these units are in today’s healthcare.
Types of ICU: An Overview

A well-lit, high-resolution photograph capturing four distinct types of intensive care units (ICUs). In the foreground, a state-of-the-art neonatal ICU with specialized incubators and monitoring equipment. In the middle ground, a cardiac ICU with advanced cardiac life support systems and telemetry. In the background, a trauma ICU with emergency resuscitation bays and imaging technology. Across the scene, a general ICU with a variety of critical care beds, ventilators, and comprehensive patient monitoring. The overall atmosphere conveys the advanced, high-stakes nature of modern intensive care medicine.
The Intensive Care Unit (ICU) has grown a lot over time. It now has many specialized types to meet different patient needs. This change helps doctors give better care to very sick patients.
General vs. Specialized ICUs
ICUs are mainly divided into general and specialized units. General ICUs handle many critical conditions. On the other hand, specialized ICUs focus on specific areas like surgery or cardiology. The choice depends on the patient’s needs and the required care level.
- General ICUs: Provide broad critical care services
- Specialized ICUs: Focus on specific conditions or patient populations
ICU Distribution in American Hospitals
In American hospitals, ICU types vary. Bigger hospitals usually have more specialized ICUs. The availability of ICUs depends on hospital size, location, and care level.
The variety in ICU types helps hospitals meet different patient needs. As healthcare changes, ICUs will likely adjust to new challenges.
Medical Intensive Care Unit (MICU)
A modern medical intensive care unit (MICU) filled with state-of-the-art equipment, bathed in soft, even lighting from overhead lamps. In the foreground, a high-tech ventilator with digital displays and intuitive controls stands ready to support critical patients’ breathing. Beside it, an infusion pump precisely administers vital medications. In the middle ground, a patient monitor with a large touchscreen displays real-time vital signs, allowing healthcare professionals to closely track the condition of those under their care. In the background, a mobile x-ray machine and other specialized medical devices stand poised to provide comprehensive diagnostic and treatment capabilities within the MICU setting. The overall atmosphere conveys a sense of advanced medical technology dedicated to saving lives.
The Medical Intensive Care Unit (MICU) is a special part of the hospital. It gives top-level care to adults with serious illnesses. We know being in the ICU can be tough for patients and their families. Our team works hard to give caring and top-notch care.
Purpose and Function
The main job of an MICU is to care for adults who are very sick or in danger. Our team is full of skilled healthcare workers. They are ready to handle many serious health issues.
Common Conditions Treated
MICUs deal with many serious health problems. These include things like diabetes emergencies, bleeding in the stomach, drug overdoses, strokes, cancer issues, and breathing problems. These issues need quick and intense treatment to keep the patient safe.
Some specific problems we handle in MICUs are:
- Severe infections and sepsis
- Respiratory failure needing a machine to breathe
- Heart problems
- Many organs not working right
- Brain problems from being very sick
Specialized Equipment
MICUs have the latest medical tools and gear. This includes machines to help patients breathe, dialysis equipment, and systems to watch patients closely. Our team can quickly see any changes in a patient’s health.
Our MICU is made to be safe and caring for patients needing a lot of care. We use the newest medical tech and care methods. This helps us give the best care and improve patient results.
Surgical Intensive Care Unit (SICU)
A modern, well-equipped Surgical Intensive Care Unit (SICU) with state-of-the-art medical equipment. The foreground features a patient bed surrounded by various monitoring devices, IV stands, and medical staff in scrubs tending to the patient. The middle ground showcases advanced life support systems, including ventilators and cardiac monitors. The background depicts a clean, sterile environment with bright, overhead lighting and a view of the bustling hospital through large windows. The atmosphere conveys a sense of focused, professional care and technological sophistication.
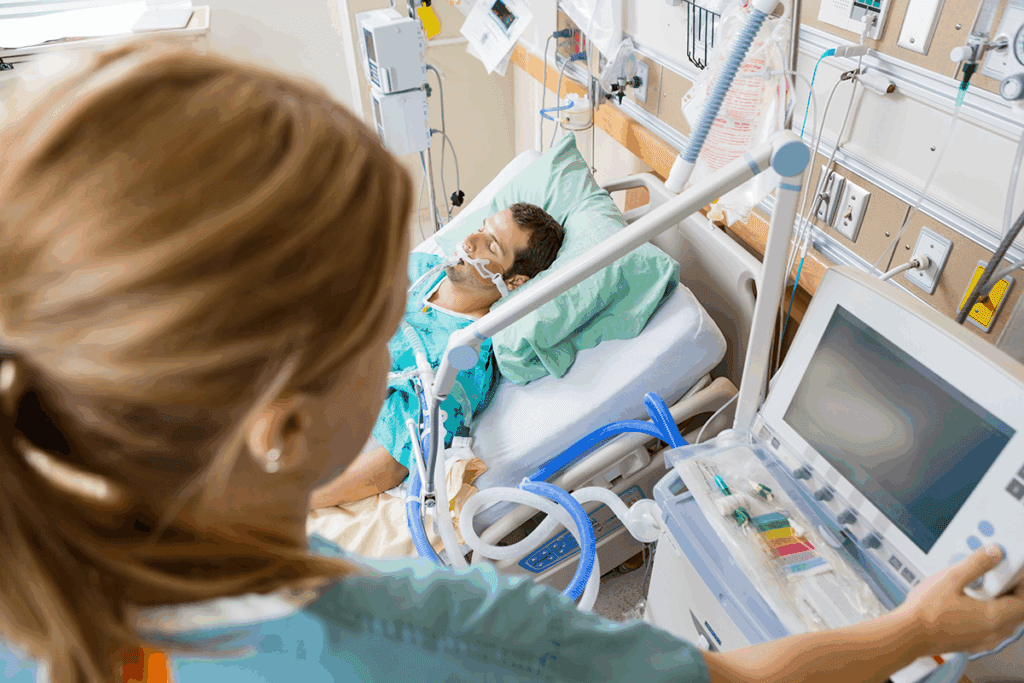
Surgical Intensive Care Units (SICUs) are key in critical care. They manage patients after big surgeries. These units offer top care for those needing close watch and support.
Role and Purpose of SICUs
SICUs focus on patients after complex surgeries. This includes surgeries like abdominal, craniotomy, and thoracotomy. They have advanced patient monitoring and a team ready for postoperative challenges.
Our SICUs meet the complex needs of patients. They provide a safe place for recovery.
Post-Operative Care Protocols
Post-operative care in SICUs is very specialized. It focuses on pain management and watching for complications. We use proven protocols to give our patients the best care.
Our care plans are flexible and focus on each patient’s needs. We make sure care is tailored for the best recovery.
Trauma Recovery in SICUs
SICUs also care for trauma patients. They provide immediate and intensive care for severe injuries. Our trauma recovery plans aim to stabilize patients and support healing.
In SICUs, we use our critical care skills for trauma patients. Our teams are ready to handle trauma care challenges. This ensures the best outcomes for our patients.
Cardiac Intensive Care Unit (CICU)
A dimly lit hospital room, the soft glow of cardiac monitoring equipment casting a gentle light across the scene. In the foreground, a patient’s bed with an array of sensors and wires connected to a central monitoring console, displaying real-time data on heart rate, blood pressure, and other vital signs. In the middle ground, a team of medical professionals, their expressions focused, intently observing the readouts and adjusting the settings as needed. In the background, a panoramic window reveals the bustling city outside, a reminder of the critical nature of the Cardiac Intensive Care Unit and the advanced technologies that enable its lifesaving work.
The Cardiac Intensive Care Unit (CICU) is a special part of hospitals for patients with serious heart issues. It’s a place where patients with severe heart problems get the care they need. The CICU is designed to be a critical environment for these patients.
Functions and Specialization
CICUs focus on patients with life-threatening heart problems, like cardiac arrest or heart attacks. Our team of healthcare professionals is ready to handle these complex heart conditions. They make sure patients get the best care possible.
The CICU works together to give cardiac care. Cardiologists, intensivists, nurses, and other experts team up. This way, they can tackle the complex needs of heart patients well.
Heart Emergency Management
Managing heart emergencies is key in the CICU. We’re ready to deal with cardiac arrests and other heart issues. We use advanced life-support technologies and proven treatment plans to help patients.
When a heart emergency happens, our team acts fast. They provide the right care to keep the patient stable. This might include giving clot-busting drugs, doing emergency angioplasty, or other urgent procedures.
Cardiac Monitoring Technologies
Advanced cardiac monitoring tools are essential in the CICU. We use the latest technology to watch over patients’ heart health. This helps us spot any issues or complications quickly.
Our CICU has top-notch monitoring systems. They track important signs like heart rate and function. This lets us customize treatment for each patient, aiming for the best results.
Neonatal Intensive Care Unit (NICU)
A state-of-the-art neonatal intensive care unit, bathed in soft, warm lighting. In the foreground, specialized medical equipment such as incubators, respirators, and monitoring devices stand ready to provide critical care. The middle ground features medical personnel in sterile attire, attentively tending to the needs of fragile newborns. The background showcases a calming, soothing environment with muted colors and minimalist decor, creating a serene atmosphere conducive to the delicate recovery of premature or critically ill infants. The scene conveys a sense of professionalism, technological advancement, and compassionate care, reflecting the essential role of a neonatal ICU.
The Neonatal Intensive Care Unit (NICU) is a special area in hospitals. It cares for newborns who are premature, very sick, or need close watching. We make sure this place is warm and caring for these tiny patients.
Purpose and Design
NICUs are made to be safe and caring for newborns. They have special equipment and technology. This helps doctors and nurses take good care of these babies.
The layout of NICUs makes it easy to get to each baby. There are incubators and monitors everywhere. This lets our team watch over the babies closely.
Specialized Care for Premature Infants
Premature babies need special care. In the NICU, we feed them just right and manage their health problems. Our team is ready to handle their delicate needs.
We treat many issues in the NICU, like breathing problems and infections. We also help with problems from being born too early. Our doctors and nurses keep parents updated and support them every step of the way.
Equipment and Technology
The NICU has advanced medical technology for newborns. This includes incubators, ventilators, and monitors. We always update our tools and methods to help our babies the best we can.
Important tools in NICUs include cardiac monitors and infusion pumps. These help our team give precise care. This improves the health of our youngest patients.
Other Specialized ICU Types
A high-tech intensive care unit, bathed in warm, clinical lighting. Sleek, cutting-edge medical equipment lines the walls, surrounded by specialized staff in sterile gowns and masks, tending to critically ill patients with the utmost care and precision. The room has a serene, yet purposeful atmosphere, conveying the advanced nature of the specialized services provided within. A complex array of monitoring screens and advanced life support systems fill the space, creating an impression of a technologically advanced, life-saving environment.
The intensive care landscape includes several specialized ICU types. Each is designed to address unique medical conditions. These units are crucial in providing high-quality, targeted care to patients with specific needs.
Pediatric ICU (PICU)
Pediatric ICUs (PICUs) are dedicated to caring for critically ill children. They are equipped with specialized equipment and staffed by healthcare professionals trained in pediatric care. PICUs provide a supportive environment that caters to the unique needs of children, from premature infants to adolescents.
The care provided in PICUs is comprehensive. It addresses a wide range of conditions, from complex surgical recoveries to severe infections. Family-centered care is a hallmark of PICUs, with families actively involved in the care and decision-making process.
Neurological ICU (Neuro ICU)
Neurological ICUs specialize in the care of patients with severe neurological conditions. These include stroke, traumatic brain injury, or spinal cord injury. Neuro ICUs are equipped with advanced monitoring technologies that enable healthcare professionals to closely monitor patients’ neurological status.
The care team in Neuro ICUs includes neurologists, neurosurgeons, and other specialists. They work together to provide comprehensive care. Rehabilitation is a key component of care in Neuro ICUs, aiming to help patients regain lost functions and achieve the best possible outcomes.
Burn ICU
Burn ICUs are dedicated to the care of patients with severe burns. These units are equipped with specialized equipment, such as burn beds and wound care facilities. Burn ICUs provide a sterile environment that minimizes the risk of infection, a major concern for burn patients.
The care team in Burn ICUs includes burn surgeons, nurses, and other specialists. They work together to provide comprehensive care. Pain management and wound care are critical components of treatment in Burn ICUs.
Respiratory ICU
Respiratory ICUs specialize in the care of patients with severe respiratory conditions. These include acute respiratory distress syndrome (ARDS). Respiratory ICUs are equipped with advanced respiratory support technologies, including mechanical ventilators and extracorporeal membrane oxygenation (ECMO) machines.
The care team in Respiratory ICUs includes pulmonologists, respiratory therapists, and other specialists. They work together to provide comprehensive care. Weaning from mechanical ventilation is a key goal in Respiratory ICUs, with the aim of helping patients regain their respiratory function.
ICU Levels and Classifications
It’s important to know about the different ICU levels. This helps us see the range of critical care services out there. ICUs are divided into levels based on their care abilities and the complexity of the care they offer.
Tertiary Care Capabilities in Level I ICUs
Level I ICUs offer the highest care level, with tertiary care capabilities. They have top-notch equipment and staff to handle complex cases. Some key features of Level I ICUs include:
- Advanced life support systems
- Specialized monitoring technologies
- Multidisciplinary teams with expertise in critical care
Comprehensive Care in Level II ICUs
Level II ICUs provide comprehensive care for a wide range of critical conditions. They might not have all the features of Level I ICUs but can still handle most critical care needs. The main characteristics of Level II ICUs are:
- Ability to provide continuous monitoring and life support
- Availability of specialized care services
- Trained staff capable of managing complex cases
Basic Critical Care in Level III ICUs
Level III ICUs offer basic critical care, helping to stabilize patients who need more care. These ICUs are key for first assessment and stabilization before moving to a higher ICU if needed. Key aspects of Level III ICUs include:
- Basic life support capabilities
- Initial assessment and stabilization of critical patients
- Arrangements for transfer to higher-level ICUs when necessary
In conclusion, knowing about the different ICU levels helps us understand their capabilities. Recognizing the care levels each ICU offers helps us navigate the healthcare system better. This ensures patients get the right care.
Critical Care Equipment and Technology
ICUs have the latest equipment to watch over and help very sick patients. The care given in these units depends a lot on advanced medical tech. This tech is key to how well patients do.
Patient Monitoring Systems
Patient monitoring systems are vital in ICUs. They let doctors and nurses keep an eye on important signs and data. These systems include heart monitors, oxygen level checkers, and brain pressure trackers, among others.
Key Features of Patient Monitoring Systems:
- Real-time data display
- Advanced alarm systems for critical changes
- Integration with electronic health records
Life Support Equipment
Life support gear is crucial for ICU patients. It helps with their most important body functions. This includes machines for breathing, kidney work, and giving medicine.
| Equipment | Function | Clinical Use |
| Mechanical Ventilators | Supports or replaces spontaneous breathing | Respiratory failure, post-operative care |
| Dialysis Machines | Performs kidney functions | Renal failure, fluid overload |
| Infusion Pumps | Delivers precise medication doses | Critical care medication administration |
Emerging Technologies in ICU Care
The world of ICU care is always changing thanks to new medical tech. New tech includes better monitoring systems, AI for predicting needs, and new life-support devices.
These new techs are changing ICU care. They help patients get better, make care more efficient, and help doctors make better choices.
As we keep adding new tech to ICU care, we’ll see even better patient care and results. The future of critical care looks bright, with tech leading the way.
Staffing and Roles in Different ICU Types
ICUs need a team of healthcare experts to care for patients well. The right staff is key to giving top-notch care.
Medical Staff Composition
ICUs have many professionals, like intensivists, critical care nurses, and respiratory therapists. Intensivists are doctors who focus on very sick patients. They make big decisions and coordinate care.
Critical care nurses are very skilled. They watch over ICU patients all the time. They make sure patients get the care they need.
| Staff Role | Responsibilities | Specialized Training |
| Intensivists | Lead care team, make critical decisions | Fellowship in Critical Care Medicine |
| Critical Care Nurses | Provide bedside care, monitor patient condition | CCRN Certification, Critical Care Coursework |
| Respiratory Therapists | Manage ventilators, administer respiratory treatments | RRT Certification, Specialized Respiratory Therapy Training |
Specialized Training Requirements
ICU staff need special training to care for very sick patients. This training includes education, certifications, and ongoing learning.
For example, intensivists get fellowship training in Critical Care Medicine. Critical care nurses get CCRN certification. Respiratory therapists need RRT certification and special training.
Interdisciplinary Collaboration
Teamwork is crucial in ICUs. It ensures patients get all-around care. Team members talk often, like during daily rounds and case discussions.
Working together is key in ICUs. It helps patients get better and improves care quality.
Patient Care Protocols Across ICU Types
ICU patient care protocols cover many steps, from when a patient comes in to when they leave. These steps are made to make sure all patients get the best care, no matter where they are in the ICU.
Admission Criteria and Triage
Getting a patient into the ICU right away is key. We use special rules to decide who needs ICU care the most. These rules help us figure out how sick a patient is and what kind of care they need.
We use scores like the Acute Physiology and Chronic Health Evaluation (APACHE) II to check how sick a patient is. This helps us decide the best care and how to use our resources.
| Scoring System | Purpose | Components |
| APACHE II | Evaluate severity of illness | Physiological variables, age, chronic health |
| SAPS II | Predict mortality | Physiological variables, type of admission |
| SOFA | Track organ dysfunction | Respiratory, cardiovascular, hepatic, renal, coagulation, neurological |
Daily Care Routines and Assessments
In ICUs, we check on patients every day. We watch their vital signs, lab results, and how their meds are working. We also have team meetings to talk about each patient’s care plan.
These daily checks help us catch any changes in a patient’s health early. We use them to see if treatments are working and make changes if needed.
Transfer and Discharge Procedures
When a patient gets better, we decide if they can move to a less intense care area or go home. We use certain rules to make these decisions, like if the patient is stable and can get the right care elsewhere.
We make sure transfers and discharges go smoothly. We give the next team all the important details about the patient’s care and any special needs.
By sticking to these protocols, we make sure our patients get top-notch care from start to finish in the ICU.
Challenges and Advancements in ICU Care
ICU environments lead in critical care, facing daily challenges. They aim for better patient outcomes. It’s key to tackle these obstacles head-on.
Current Challenges in Critical Care
ICUs face many hurdles despite medical progress. Staffing shortages are a big problem, affecting care quality. Hospital-acquired infections are also a major concern, needing strict control measures.
The mental toll of ICU care on patients and families is significant. The stress of critical illness can last long. Thus, care must include psychological support.
Innovations and Future Directions
New technologies like artificial intelligence and telemedicine are changing ICU care. They improve patient care and outcomes. Personalized medicine is also becoming more common, fitting treatments to each patient’s needs.
Future ICU care will see better patient monitoring and life support. These advancements will make care more precise and effective. This will lead to better patient results.
| Challenge | Innovation | Benefit |
| Staffing Shortages | Telemedicine | Increased access to specialist care |
| Infection Control | Advanced sterilization technologies | Reduced hospital-acquired infections |
| Psychological Impact | Holistic care approaches | Improved patient and family well-being |
The future of ICU care looks promising. It will be shaped by tackling current challenges and embracing new ideas. This way, ICUs can keep providing top-notch care to those in need.
Conclusion
Intensive Care Units (ICUs) are key in healthcare, helping patients with severe conditions. We’ve looked at the different ICUs, each focusing on specific critical care areas. This includes medical, surgical, cardiac, and neonatal care.
The need for ICUs will keep growing thanks to new medical tech and the need for better care. ICUs have the latest life-support tools and teams of skilled professionals. They work together to give patients the best care possible.
Good care in ICUs needs a team effort, with constant monitoring and quick action. As healthcare changes, ICUs must stay ahead. They need to provide the specialized care that critically ill patients need.
In short, ICUs are vital in today’s healthcare. They help improve patient outcomes. By understanding the different ICUs and their roles, we see the importance of critical care. ICUs are essential for delivering top-notch healthcare.
FAQ
What are the primary types of Intensive Care Units (ICUs)?
There are several main types of ICUs. These include Medical ICU, Surgical ICU, Cardiac ICU, and Neonatal ICU. Each one focuses on different patient needs and offers specialized care.
What is the purpose of a Medical Intensive Care Unit (MICU)?
MICUs care for adult patients with severe medical issues. They need close monitoring and life-supporting treatments.
What kind of care is provided in a Surgical Intensive Care Unit (SICU)?
SICUs watch over patients who have had major surgery or suffered trauma. They manage complications and help with recovery.
What is the specialization of a Cardiac Intensive Care Unit (CICU)?
CICUs focus on patients with severe heart conditions. They handle heart emergencies and provide advanced cardiac care.
What is the purpose of a Neonatal Intensive Care Unit (NICU)?
NICUs care for newborns who are premature, critically ill, or need close monitoring. They create a safe, nurturing environment for these babies.
Are there other specialized types of ICUs beyond the primary ones?
Yes, there are more specialized ICUs. These include Pediatric ICU (PICU), Neurological ICU (Neuro ICU), Burn ICU, and Respiratory ICU. Each one serves specific patient groups and conditions.
How are ICUs categorized, and what do these classifications mean?
ICUs are grouped by care level. Level I ICUs offer the most advanced care. Level III ICUs provide basic critical care.
What kind of equipment and technology are used in ICUs?
ICUs use advanced tools and tech. This includes patient monitoring systems, life support devices, and new technologies to improve care.
What is the role of staffing in ICUs, and what kind of training is required?
Staffing in ICUs is key to quality care. Teams include intensivists, critical care nurses, and respiratory therapists. They need special training to care for critically ill patients.
What are some of the current challenges and future directions in ICU care?
ICUs face challenges like staffing shortages and hospital infections. Future goals include using technology to improve care and outcomes.
How do patient care protocols vary across different ICU types?
Care protocols in ICUs vary by type. They include admission rules, daily routines, and transfer procedures. Each is tailored to the specific needs of patients and the ICU type.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10325721/