Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, thousands of people worldwide suffer from a stroke, also known as a cerebrovascular accident (CVA). This happens when blood flow to the brain stops. It leads to cell death and can cause severe problems cerebrovascular disease.
We often mix up “stroke” and “cerebrovascular accident,” but knowing the difference is key. A stroke or CVA can greatly affect a person’s life. Understanding the causes and effects of strokes is crucial.
Key Takeaways
- A stroke and a cerebrovascular accident are terms often used interchangeably.
- The interruption of blood flow to the brain leads to cell death.
- Understanding the nuances between these terms is crucial for diagnosis and treatment.
- Stroke or CVA can have severe consequences on an individual’s quality of life.
- Comprehending the underlying causes is essential for effective management.
Defining Cerebrovascular Events: CVA vs. Stroke
It’s important to know the difference between CVA and stroke for the right treatment. Both deal with brain blood supply issues, but they have key differences. This knowledge helps doctors and patients.
Medical Terminology and Distinctions
CVA, or Cerebrovascular Accident, is often called “stroke.” But CVA includes more types of brain blood issues. An ischemic cerebrovascular accident blocks a brain blood vessel. A hemorrhagic CVA is when a brain blood vessel bursts.
TIA, or Transient Ischemic Attack, is called a “mini-stroke.” It’s when symptoms last less than 24 hours. Knowing these differences helps doctors treat right.
Historical Evolution of the Terms
At first, “stroke” meant sudden brain problems. As we learned more, so did our words. Now, CVA is used to show it’s a blood issue.
Our understanding of brain blood diseases has grown. This history helps us see how to diagnose and treat better.
Current Usage in Clinical Practice
Today, both “stroke” and “CVA” are used, depending on the situation. “Stroke” is often used in emergencies to quickly explain the problem. “CVA” is used in detailed medical records for a precise diagnosis.
Knowing what causes stroke is key to managing it. Whether it’s a blockage or a burst, quick and right care is crucial.
The Pathophysiology of Cerebrovascular Disease
The brain’s blood vessels are key to its health. Problems with these vessels can cause serious issues. Cerebrovascular disease affects the brain’s blood supply, leading to strokes and other brain injuries.
Brain Vasculature and Blood Supply
The brain gets its blood from arteries branching from the aorta and vertebral arteries. The cerebral circulation is a complex system. It ensures the brain gets enough oxygen and nutrients.
“The cerebral vasculature is a complex system that is essential for maintaining the brain’s homeostasis,” as noted by medical professionals. The brain’s blood vessels can adjust blood flow based on neural activity, a process known as neurovascular coupling.
Cerebral Circulation Dynamics
Cerebral circulation is about controlling blood flow in the brain. This is vital for brain function. Blood pressure, CO2 levels, and neural activity all play a role in this.
- Cerebral autoregulation helps maintain a constant blood flow despite changes in systemic blood pressure.
- Chemical regulation, particularly through CO2 levels, affects cerebral vessel diameter.
- Neural regulation involves the release of vasoactive substances that can dilate or constrict cerebral vessels.
Mechanisms of Brain Injury
Brain injury in cerebrovascular disease can happen in different ways. Ischemia causes damage by cutting off blood flow. Hemorrhage causes damage through bleeding into or around the brain.
Understanding these causes is key to treating cerebrovascular disease. “Early intervention is key to minimizing brain damage in cerebrovascular events,” as emphasized by healthcare professionals.
Types of Cerebrovascular Accidents
Strokes, or cerebrovascular accidents, are mainly split into ischemic and hemorrhagic types. Knowing which one a patient has is key to choosing the right treatment.
It’s important to understand the differences between these two types. We’ll look at each one, starting with ischemic events.
Ischemic Events
Ischemic strokes happen when a blood vessel in the brain gets blocked. This reduces blood flow. About 87% of strokes are ischemic. Ischemic strokes can be either thrombotic or embolic.
- Thrombotic strokes are caused by a blood clot in a brain blood vessel.
- Embolic strokes happen when a clot from elsewhere blocks a brain blood vessel.
Treatment for ischemic strokes often includes thrombolytic therapy. This helps dissolve the clot and get blood flowing again. Quick action is vital to prevent brain damage.
Hemorrhagic Events
Hemorrhagic strokes are caused by a blood vessel in the brain bursting. This leads to bleeding. This category includes intracerebral and subarachnoid hemorrhage.
- Intracerebral hemorrhage happens when a blood vessel in the brain’s tissue bursts.
- Subarachnoid hemorrhage is when bleeding occurs in the space around the brain.
Managing hemorrhagic strokes involves stopping the bleeding and lowering brain pressure. It also aims to prevent more problems.
Both types of cerebrovascular accidents need quick and proper treatment to help patients. Knowing the differences between ischemic and hemorrhagic strokes is crucial for doctors to provide the best care.
Transient Ischemic Attack: The “Mini-Stroke”
It’s key to know about TIAs to spot stroke warning signs. A Transient Ischemic Attack (TIA), or “mini-stroke,” is when brain blood flow stops briefly. It shows stroke-like signs but goes away in 24 hours, usually without lasting harm.
TIA Medical Definition and Characteristics
A TIA is a short brain or eye blood flow stoppage without lasting damage. Its symptoms are like a stroke’s, including sudden weakness, speech trouble, vision changes, dizziness, or balance loss.
TIAs are short-lived and can be reversed. Yet, they’re serious because they mean a big stroke risk is coming.
Distinguishing TIAs from Complete Strokes
The main difference between a TIA and a stroke is how long symptoms last and brain damage extent. TIAs don’t cause permanent brain harm because blood flow stops only briefly.
Telling TIAs from strokes is vital for quick medical help. Tests like MRI or CT scans show if brain tissue is permanently damaged.
Importance as Warning Signs
TIAs are important warning signs for a stroke. Acting fast on TIA symptoms can greatly lower stroke risk. It’s very important for those with TIA symptoms to get medical help right away.
After finding out about a TIA, doctors can start steps to stop another stroke. This might include changing lifestyle, taking blood clot meds, or managing health issues like high blood pressure or diabetes.
Understanding TIAs helps us prevent worse brain problems. As healthcare workers, we must teach patients about TIA symptoms and how to act on them.
Etiology and Risk Factors
Understanding the causes of cerebrovascular accidents is key. It involves knowing both changeable and unchangeable risk factors. This knowledge is vital for preventing and managing strokes.
Modifiable Risk Factors
There are several risk factors for stroke that can be changed. High blood pressure can damage brain blood vessels, making them more likely to block or rupture. Diabetes can also narrow blood vessels, raising stroke risk.
Other changeable risk factors include:
- Smoking
- High cholesterol
- Heart disease
- Obesity and physical inactivity
- Poor diet
By making lifestyle changes and getting medical help, you can lower your stroke risk.
Non-modifiable Risk Factors
Some risk factors can’t be changed, but knowing them is still important. Age is a big one, as stroke risk goes up with age. Family history of stroke also matters, suggesting a possible genetic link.
Other unchangeable risk factors include:
Risk Factor | Description |
Gender | Men are generally at higher risk of stroke than women, though women’s risk increases after menopause. |
Race/Ethnicity | African Americans are at higher risk of stroke than other ethnic groups. |
Previous Stroke or TIA | A history of stroke or transient ischemic attack (TIA) significantly increases the risk of future strokes. |
Knowing these unchangeable risk factors helps both individuals and healthcare providers. It encourages taking steps to manage changeable risks and closely watching those at higher risk.
Clinical Presentation and Symptoms
Knowing the signs of a stroke is key to quick medical help. We need to spot the classic warning signs and use good assessment methods to find stroke victims fast.
Classic Stroke Symptoms and Warning Signs
Stroke symptoms include sudden numbness or weakness in the face, arm, or leg, especially on one side. Other signs are speech difficulties, like slurred speech or trouble understanding, and vision problems, like sudden vision loss or double vision.
Other warning signs are sudden severe headache, dizziness, or loss of balance. Remember, stroke symptoms can differ based on the person and the brain area affected.
The FAST Assessment Method
The FAST method is a well-known tool for spotting stroke victims. FAST stands for:
- Face: Ask the person to smile. Does one side of their face droop?
- Arm: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple sentence. Is their speech slurred or hard to understand?
- Time: Time is crucial. If the person shows any of these symptoms, call for emergency services right away.
Location-Specific Manifestations
Stroke symptoms can vary based on the brain area affected. For example, a stroke in the left hemisphere can cause language problems. A stroke in the right hemisphere can affect spatial awareness and judgment.
Knowing these specific symptoms helps healthcare providers tailor their care to each patient’s needs.
Diagnostic Approaches and Imaging
Getting a stroke diagnosis right is key. It starts with a check-up and then uses advanced tests.
Initial Clinical Assessment
The first step is a detailed check-up. We look at the patient’s health history and symptoms. We also do a physical exam. This helps us figure out if a stroke might be happening and what tests to do next.
Neuroimaging Techniques
Neuroimaging is very important for finding out about strokes. We use CT scans and MRI to see the brain. This helps us know what kind of stroke it is and how big it is.
CT scans are quick and easy to get, which is why they’re often used first. They show if there’s bleeding. MRI gives us more detailed pictures of the brain. It’s great for spotting ischemic strokes.
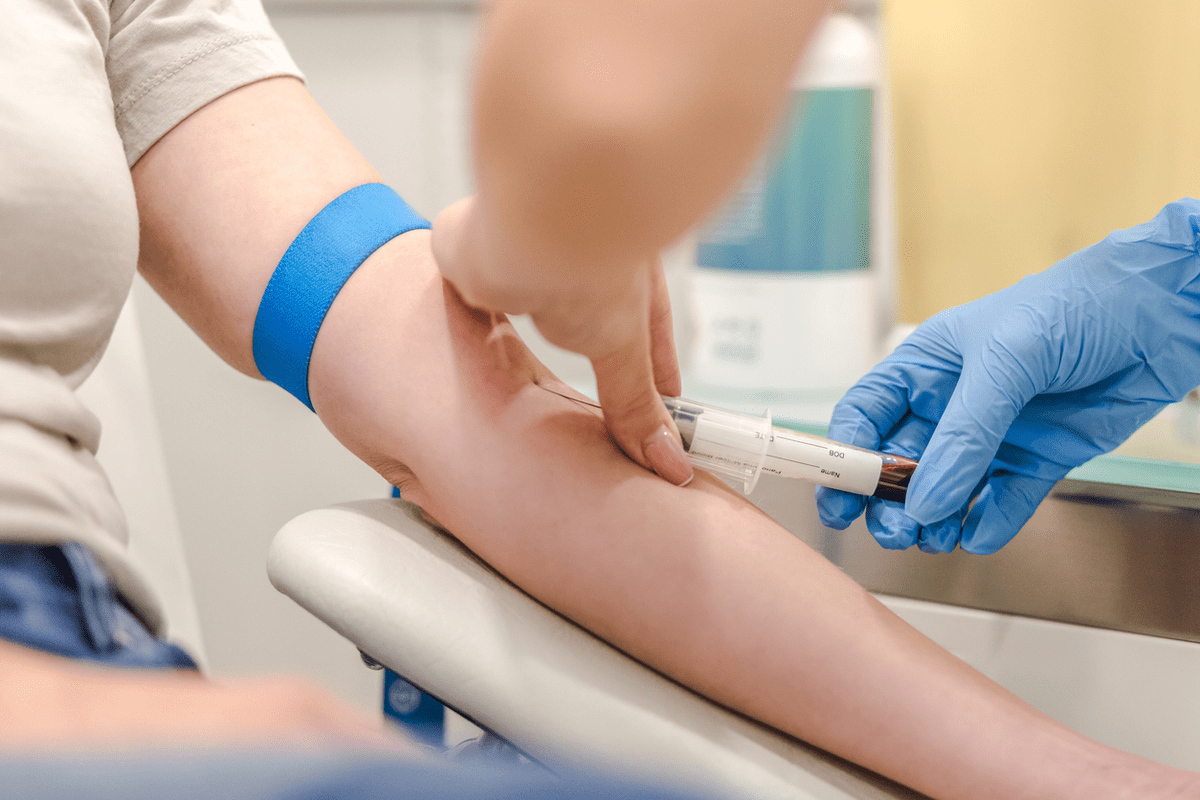
Laboratory Investigations
Labs are key for checking if other things could be causing symptoms. We test things like blood sugar, blood counts, and how blood clots. These tests help us see how the patient is overall.
By looking at the results from the check-up, scans, and lab tests, we can really know if someone has had a stroke. Then, we can plan the best treatment.
Acute Management and Treatment Strategies
In the early stages of a stroke, quick and right actions are key to saving lives and lessening harm. A team of healthcare experts works together to manage the situation effectively.
Time-Critical Interventions
The first hours after a stroke are vital. Time-critical interventions aim to get blood flowing to the brain again. This helps reduce damage. It’s most effective when done quickly.
It’s crucial to spot stroke signs early and get medical help fast. Thrombolytic therapy is a main part of stroke care, if the patient gets help in time.
Thrombolytic Therapy
Thrombolytic therapy uses medicines to break up blood clots. Alteplase is a common drug that helps improve outcomes for stroke patients.
Doctors decide if this therapy is right based on several factors. These include how long since the stroke started, the patient’s health history, and what the scans show.
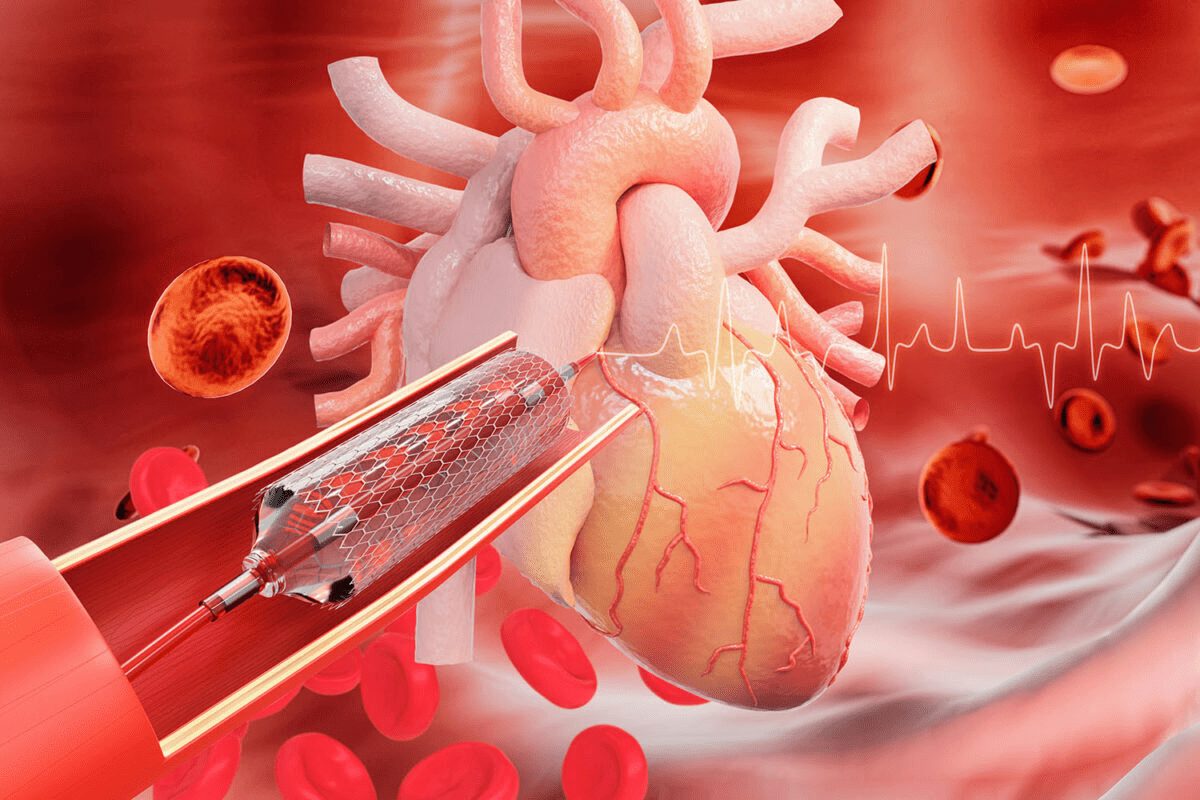
Endovascular Procedures
For those who can’t get thrombolytic therapy or if it doesn’t work, endovascular procedures are an option. These involve using a mechanical device to remove the clot.
Who gets this treatment depends on several things. These include the type of stroke, how big the blockage is, and how much brain tissue can be saved.
Surgical Management Options
In hemorrhagic strokes or big ischemic strokes with swelling, surgical management might be needed. Surgery can include removing part of the skull to relieve pressure.
Whether to have surgery depends on the patient’s condition, what the scans show, and their likely outcome.
Rehabilitation and Recovery Processes
Stroke survivors need a multidisciplinary rehabilitation strategy to regain lost functions. This approach is key for a good recovery and quality of life.
Multidisciplinary Rehabilitation Approach
A team of healthcare professionals works together. They include physical therapists, occupational therapists, speech-language pathologists, and psychologists. This team creates a plan that fits the individual’s needs and goals.
Physical and Mobility Rehabilitation
Physical therapy is crucial for regaining mobility and strength. Physical therapists use proven methods to improve balance and coordination. This helps patients do daily activities better.
Speech and Cognitive Therapy
Speech therapy helps with communication issues like aphasia and dysarthria. Speech-language pathologists work to improve speech and comprehension. Cognitive therapy boosts memory, attention, and problem-solving skills.
Psychological Support and Adaptation
The psychological effects of a stroke are significant. Psychological support is vital for managing emotional changes like depression and anxiety. Psychologists and counselors offer support and teach coping strategies.
Using a multidisciplinary approach to rehabilitation helps stroke survivors a lot. This care model meets the complex needs of stroke patients. It supports them on their recovery journey.
Long-term Complications of Cerebrovascular Accidents
After a stroke, patients face many long-term challenges. These can greatly affect their recovery and happiness. Getting the right care is key.
Physical Sequelae
Physical problems are common after a stroke. These can include weakness on one side of the body and trouble with balance. Rehabilitation programs help patients regain their independence.
- Hemiparesis or hemiplegia
- Coordination and balance issues
- Chronic pain
- Fatigue
Cognitive and Neuropsychological Effects
Strokes can also harm a person’s mind. This can range from small memory problems to severe dementia. Neuropsychological assessments help figure out how much damage there is and what to do next.
- Memory loss
- Attention deficits
- Executive function impairments
- Language difficulties
Development of Vascular Dementia
People who have had a stroke are more likely to get vascular dementia. This is when the brain doesn’t get enough blood and it starts to decline. It’s important to manage risk factors to stop this from getting worse.
Impact on Quality of Life
Strokes can really change a person’s life. They can lead to physical problems, memory loss, and emotional issues. It’s important to have care that covers all these areas to help improve life.
Knowing about the long-term effects of strokes helps doctors give better care. This care can help patients recover and live better lives.
Prevention of Cerebrovascular Disease
Preventing cerebrovascular disease requires both primary and secondary measures. Primary prevention aims to stop a first stroke. Secondary prevention helps those who have had a TIA or stroke avoid more.
Primary Prevention Strategies
Primary prevention is key for those at high risk. It includes a healthy diet, regular exercise, managing blood pressure, and not smoking. It also means controlling diabetes and high cholesterol through diet and medicine.
Eating well, like fruits and veggies, can lower stroke risk. Exercise, like walking, boosts heart health. Keeping blood pressure in check is also vital.
Lifestyle Modification | Benefit |
Healthy Diet | Reduces risk of stroke and cardiovascular disease |
Regular Physical Activity | Improves cardiovascular health and reduces stroke risk |
Hypertension Management | Critical in preventing stroke |
Smoking Cessation | Significantly reduces stroke and cardiovascular risk |
Secondary Prevention After TIA or Stroke
After a TIA or stroke, secondary prevention is crucial. It includes managing risk factors, lifestyle changes, and sometimes medicine.
Doctors may use blood thinners, manage blood pressure, and control cholesterol. Lifestyle changes are also important.
Medication Regimens
Medicine is vital for preventing strokes. For the first time, managing blood pressure and diabetes is key. After a stroke, blood thinners and statins help prevent more.
By using these strategies, we can greatly reduce stroke risk. It’s a mix of medicine and lifestyle changes, based on each person’s needs.
Special Considerations in Stroke Management
Managing strokes requires special care, especially for kids and pregnant women. These cases need unique approaches to diagnosis, treatment, and recovery.
Pediatric Cerebrovascular Events
Pediatric stroke is rare but serious. It’s hard to diagnose because kids often show non-specific symptoms.
Key differences in pediatric stroke management include:
- Higher likelihood of underlying genetic or congenital conditions
- Different risk factors, such as sickle cell disease
- Need for age-appropriate treatment protocols
Pregnancy-Associated Strokes
Pregnancy increases the risk of stroke for mothers. Both ischemic and hemorrhagic strokes are more common.
Management challenges include:
- Balancing maternal and fetal health considerations
- Adapting treatment protocols to accommodate pregnancy-related physiological changes
- Managing potential complications such as preeclampsia
Ethnic and Racial Disparities in Care
Stroke care and outcomes vary by ethnicity and race. These differences stem from socioeconomic, environmental, and healthcare access factors.
Ethnic/Racial Group | Stroke Incidence | Stroke Mortality |
African American | Higher incidence | Higher mortality |
Hispanic/Latino | Variable incidence | Higher mortality |
Caucasian | Lower incidence | Lower mortality |
Emerging Research Directions
Stroke research is advancing quickly. New areas of study are showing promise.
Emerging trends include:
- Advanced imaging techniques for improved diagnosis
- Personalized medicine approaches based on genetic profiling
- Novel therapeutic agents for neuroprotection and recovery
Conclusion: Navigating Cerebrovascular Health
Understanding cerebrovascular health is key to preventing, diagnosing, and managing stroke and CVA. We stress the need to be aware, prevent, and manage cerebrovascular health effectively.
Knowing about stroke and CVA helps people understand their risks and outcomes better. Early detection and timely medical help are crucial. They greatly improve patient results.
Preventing and managing cerebrovascular disease need a wide approach. This includes changing lifestyles, medical treatments, and sometimes surgery. We must focus on cerebrovascular health to lower stroke rates and effects.
Good management strategies, like rehabilitation and preventing future strokes, are vital. They help improve life quality for those with stroke and CVA. By focusing on cerebrovascular health, we aim to lessen the global stroke burden.
FAQ
What is the difference between a cerebrovascular accident (CVA) and a stroke?
Both refer to brain cell death due to blood flow interruption. “CVA” is a broader term that includes strokes and TIAs. It covers various cerebrovascular events.
What are the main types of cerebrovascular accidents?
There are mainly two types: ischemic and hemorrhagic. Ischemic strokes happen when a blood vessel gets blocked. Hemorrhagic strokes occur when there’s bleeding in or around the brain.
What is a transient ischemic attack (TIA), and why is it significant?
A TIA, or “mini-stroke,” is a short blockage of brain blood flow that clears in 24 hours. It’s important because it warns of future strokes. It shows the need for quick medical checks and prevention.
What are the modifiable risk factors for stroke?
Risk factors for stroke that can be changed include high blood pressure, diabetes, high cholesterol, smoking, and irregular heartbeat. Changing these through lifestyle and medicine can lower stroke risk.
How is a stroke diagnosed?
Diagnosing a stroke involves a quick check by a doctor, scans like CT or MRI, and lab tests. Accurate diagnosis is key for the right treatment.
What is the FAST assessment method, and how is it used?
FAST helps spot stroke symptoms quickly: Face drooping, Arm weakness, Speech issues, and Time to call for help. It helps quickly identify and act on stroke signs.
What are the treatment options for acute ischemic stroke?
Treatments for acute ischemic stroke include dissolving the clot with medicine, removing the clot with a procedure, and supportive care. Quick action is vital for better outcomes.
What is the role of rehabilitation after a stroke?
Rehabilitation helps stroke survivors regain lost functions and adapt to any lasting effects. It includes physical, speech, and cognitive therapy, along with psychological support. This approach is key for the best recovery.
Can strokes be prevented?
Yes, strokes can be prevented or their risk greatly reduced. This can be done through managing risk factors and taking steps after a TIA or stroke. Lifestyle changes and medicine are part of this.
What are the long-term complications of cerebrovascular accidents?
Long-term effects can include physical, cognitive, and neuropsychological issues. Vascular dementia can also develop, affecting quality of life. Ongoing care and support are needed to manage these issues.
Are there special considerations in the management of stroke?
Yes, special considerations include managing strokes in children and pregnant women. It also includes addressing ethnic and racial disparities in care. Keeping up with new research is also important.
References
National Center for Biotechnology Information. Stroke Versus Cerebrovascular Accident Clarification. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538338/