Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 700,000 people worldwide are diagnosed with a brain tumor each year. Radiation therapy is a common treatment for this.
Going through radiation therapy can be tough. It’s normal to wonder how well it works.
Knowing how a tumor will react to radiation is key. It helps set realistic hopes and makes treatment choices clearer.
Key Takeaways
- Radiation therapy is a common treatment for brain tumors.
- The response to radiation therapy varies among patients.
- Understanding the tumor shrinkage timeline helps manage patient expectations.
- Cancer treatment progress is closely monitored by healthcare professionals.
- Effective radiation therapy can significantly improve patient outcomes.
Understanding Brain Tumors and Radiation Therapy

It’s important to know about brain tumors and how they react to radiation therapy. Brain tumors can be either primary or metastatic. Each type grows differently and has its own characteristics.
Types of Brain Tumors and Their Growth Patterns
Brain tumors can be either benign or malignant. Benign tumors grow slowly and are usually not dangerous. But, they can cause problems because of where they are.
Malignant tumors grow faster and can spread to other parts of the brain. Primary brain tumors start in the brain. Metastatic tumors come from other parts of the body.
The most common primary brain tumors are gliomas, meningiomas, and acoustic neuromas.
| Tumor Type | Growth Pattern | Malignancy |
| Gliomas | Variable, can be slow or rapid | Can be benign or malignant |
| Meningiomas | Typically slow-growing | Usually benign |
| Acoustic Neuroma | Slow-growing | Benign |
How Radiation Therapy Works Against Brain Tumors
Radiation therapy is a key treatment for brain tumors. It damages the DNA of tumor cells, stopping them from growing. High-energy rays are used to target the tumor.
There are several types of radiation therapy. External beam radiation therapy (EBRT) comes from outside the body. Stereotactic radiosurgery (SRS) focuses radiation directly on the tumor.
Radiation therapy can be used alone or with other treatments like surgery and chemotherapy. The treatment plan depends on the tumor’s type, size, and location. It also depends on the patient’s health.
Tumor Shrinkage Timeline: What to Expect
Knowing when a tumor shrinks after radiation is key for patients and doctors. How a tumor reacts to radiation depends on its type, grade, and the radiation method used.
Immediate Effects After Radiation
Right after radiation, the tumor might not change much. Sometimes, it could even look bigger due to swelling. This swelling is not a sign that treatment failed. We use MRI tumor monitoring to tell if it’s real growth or just swelling.
Short-term Response (1-3 months)
Within 1-3 months, some patients see their tumors get smaller. But not everyone, and how fast it happens varies. Post-radiation effects like tiredness and hair loss can happen, but they’re usually short-lived. Regular MRI scans help us see how well the treatment is working and make changes if needed.
Long-term Response (3-12 months)
Between 3 to 12 months, we can really see how well the treatment worked. Many patients see big changes in their tumors. The tumor shrinkage timeline depends on the tumor, its size, and the radiation dose. Keeping an eye on the tumor with MRI tumor monitoring is key to adjusting treatment plans.
It’s important to remember that everyone’s experience is different. The tumor’s biology and the patient’s health affect how much and how fast it shrinks. By watching the radiation therapy response closely, doctors can tailor care and support to each patient’s needs.
Factors Affecting Tumor Shrinkage Rate
It’s important to know what affects how fast a brain tumor shrinks after radiation. The speed of shrinkage isn’t the same for everyone. Several key factors can influence this.
Tumor Type and Grade
The type and grade of the tumor are very important. Different tumors react differently to radiation. For example, low-grade gliomas might take longer to shrink than high-grade glioblastomas.
The grade of the tumor also matters. It shows how much the tumor cells look like normal cells. High-grade tumors are usually more aggressive and might not respond the same way as low-grade tumors.
- Tumor Type: Different tumor types have varying sensitivities to radiation.
- Tumor Grade: Higher-grade tumors may respond differently compared to lower-grade ones.
Tumor Size and Location
The size and location of the tumor also play a big role. Bigger tumors take longer to shrink. Smaller tumors can shrink faster. Tumors near important brain areas need special care to avoid harm.
- Tumor size affects the shrinkage rate, with larger tumors potentially taking longer to respond.
- Tumors in sensitive locations may require specialized radiation approaches.
Patient-Specific Factors
Each patient’s health, age, and genetics can also affect how well they respond to radiation. Younger patients might do better than older ones. Some genetic markers can change how a tumor reacts to radiation.
Knowing these factors helps doctors plan better treatments. This way, they can make radiation therapy more effective for each patient. It’s all about making treatment work best for each person.
Different Radiation Approaches and Their Impact on Shrinkage Time
Radiation therapy for brain tumors uses many techniques. Each method affects how fast a tumor shrinks. It’s important for patients and doctors to know the differences.
Conventional External Beam Radiation
Conventional external beam radiation therapy (EBRT) is common for brain tumors. It sends radiation from outside the body to the tumor. EBRT works well for big tumors or those that can’t be removed. The treatment is given in parts over weeks, helping the tumor shrink slowly.
How well EBRT works can change. Patients often get scans to see how the tumor is doing. How long treatment lasts and how often scans are needed can affect how we see tumor shrinkage.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery (SRS) is very precise. It gives a big dose of radiation in one or a few sessions. SRS is good for small tumors or those that are easy to spot. It also helps protect healthy brain tissue.
SRS can cause tumors to shrink quickly. Some people see big changes in a few months. But, how a tumor responds can depend on its type and other things.
Proton Therapy and Other Advanced Techniques
Proton therapy uses protons instead of X-rays to kill cancer cells. This method is precise, which helps protect healthy tissue. It’s great for tumors near important areas or for kids.
Other advanced methods like IMRT and VMAT also offer better precision and fewer side effects. These can be customized for each patient, possibly improving how well tumors shrink.
| Radiation Technique | Tumor Size Suitability | Precision | Typical Treatment Duration |
| Conventional EBRT | Large tumors | Moderate | Several weeks |
| Stereotactic Radiosurgery (SRS) | Small to medium tumors | High | 1-5 sessions |
| Proton Therapy | Variable | High | Several weeks |
It’s key to understand the different radiation methods and how they affect tumor shrinkage. Choosing the right method for each patient can lead to better treatment results and a better life.
Primary vs. Metastatic Brain Tumors: Differences in Response Time
It’s important to know how primary and metastatic brain tumors react to radiation therapy. Primary tumors start in the brain, while metastatic tumors spread from other parts of the body. This difference affects how well they respond to treatment.
Response Patterns in Primary Brain Tumors
Primary brain tumors, like gliomas, react differently to radiation therapy. Some tumors respond fast, while others take longer or don’t respond at all.
Gliomas, a common primary brain tumor, show varied responses. Low-grade gliomas may take months to years to respond. On the other hand, high-grade gliomas might respond quickly but have a shorter survival time.
Response Patterns in Metastatic Brain Tumors
Metastatic brain tumors react differently than primary tumors. They often respond well to radiation therapy in the short term.
Research shows metastatic tumors can respond to radiation therapy in weeks to months. Stereotactic radiosurgery (SRS) is very effective for these tumors, giving them a high chance of local control.
Monitoring Tumor Shrinkage After Radiation
It’s important to check how tumors change after radiation treatment. We use special imaging to see if the treatment is working. This helps us know if we need to make any changes.
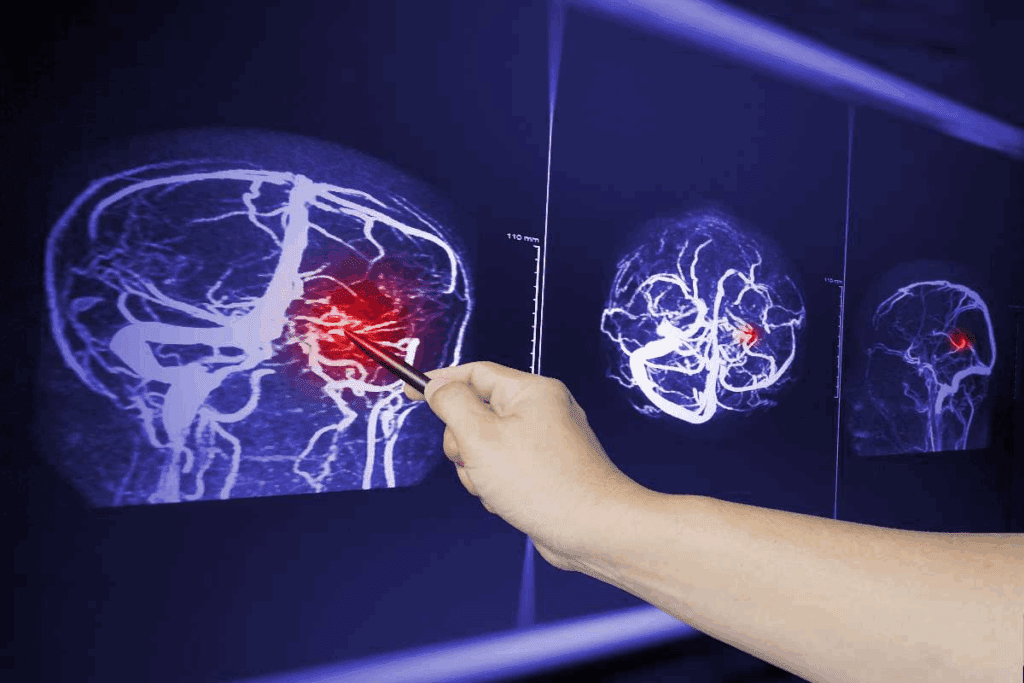
MRI and Other Imaging Techniques
Magnetic Resonance Imaging (MRI) is a key tool for checking tumor response after radiation. It gives clear pictures of the brain. Doctors can then measure how big the tumor is and see if it’s changing.
Other methods like Computed Tomography (CT) scans and Positron Emission Tomography (PET) scans might also be used. This depends on the specific situation.
Each imaging method has its own benefits. MRI is great for soft tissue tumors. CT scans are better for finding calcifications. PET scans show how active the tumor is, helping tell real tumor from scar tissue.
Frequency of Follow-up Imaging
How often we need to do follow-up imaging depends on several things. These include the type of tumor, its size, and the patient’s health. Usually, we do imaging every 3-6 months to see how the tumor is responding.
Some patients might need more frequent checks. This is true if there are concerns about how the tumor is acting or if there could be complications. Our team makes sure the imaging schedule fits each patient’s needs.
What Radiologists Look For
Radiologists look for important signs when they review imaging. They check for changes in tumor size and how the tumor looks on MRI. They also look for any new growths.
A smaller tumor is a good sign, showing the treatment is working. But, they also watch for signs of problems. These could be radiation damage or changes that look like the tumor is growing again.
By closely watching how tumors respond, we can adjust treatments. This helps us give our patients the best care possible.
Interpreting Imaging Results: Shrinkage vs. Pseudo-progression
After radiation therapy, doctors look at imaging results to see if tumors are shrinking or not. It’s important to know if the tumor is really getting smaller or if it looks that way because of the treatment. This helps doctors decide if the treatment is working and what to do next.
Understanding Pseudo-progression
Pseudo-progression happens when scans show the tumor looks like it’s getting bigger. But, it’s really just because of the treatment, not because the tumor is actually growing. This can happen in about 30% of patients with brain tumors who get radiation therapy.
This can worry patients because it looks like the tumor is getting worse. But, it’s common and doesn’t mean the treatment has failed.
Distinguishing True Response from Treatment Effects
It’s hard to tell if a tumor is really shrinking or if it’s just looking that way because of the treatment. Doctors need to look at the scans carefully and also consider how the patient is feeling and other tests.
Key factors in this evaluation include:
- Changes in tumor size and appearance on serial imaging studies
- Clinical symptoms and their progression or resolution
- Advanced imaging techniques, such as perfusion-weighted MRI or spectroscopy
By looking at these things, doctors can better understand how well the treatment is working. They can then change the treatment plan if needed.
Accurate interpretation of imaging results is vital for patient care. It affects treatment choices and how well patients do. Our team works hard to give the best care and support to our patients during their treatment.
Common Response Patterns for Specific Brain Tumor Types
It’s important to know how different brain tumors react to radiation therapy. This knowledge helps manage what patients can expect. The way tumors respond depends on the type, grade, and other factors.
Other Common Brain Tumor Types
Other brain tumors, like acoustic neuromas and pituitary adenomas, also react differently to radiation therapy. Acoustic neuromas may take 1 to 3 years to respond, while pituitary adenomas can respond in 6 to 12 months.
It’s key to remember that each person’s response can be different. Things like tumor size, location, and individual health factors affect how a tumor responds.
As we improve radiation therapy, we can better treat various brain tumors. Knowing how tumors usually respond helps us make treatment plans that work best for each patient. This way, we can improve their outcomes and quality of life.
When Tumors Don’t Shrink: Understanding Radiation Resistance
It’s important to know why some brain tumors don’t shrink after radiation therapy. This knowledge helps us find new ways to treat cancer. Radiation resistance is a complex issue that affects how well cancer treatments work.
Radiation therapy damages the DNA of tumor cells, stopping them from growing. But, some cells can fix this damage or become less affected by radiation. This makes them resistant to treatment.
Biological Mechanisms of Radiation Resistance
The reasons behind radiation resistance are complex. They involve many cellular pathways and genetic factors. These allow tumor cells to keep growing even after radiation.
The tumor’s environment also plays a big role. For example, if the tumor is not getting enough oxygen, it becomes more resistant to radiation. This is because oxygen helps radiation damage cells more effectively.
Genetic changes are another key factor. Mutations in genes related to DNA repair, cell cycle, and apoptosis help tumors resist radiation.
“The development of radiation resistance is often associated with changes in the tumor microenvironment and genetic makeup of the tumor cells.”
Treatment Options for Radiation-Resistant Tumors
When tumors don’t respond to radiation, we need to try other treatments. These can include chemotherapy, targeted therapy, immunotherapy, or a mix of these.
Chemotherapy can help when used with radiation therapy. Targeted therapies focus on specific molecules that help tumors grow. They can be very effective.
- Chemotherapy
- Targeted therapy
- Immunotherapy
Immunotherapy uses the body’s immune system to fight cancer. It’s a good option for tumors that are hard to treat with usual methods.
By understanding radiation resistance and trying different treatments, we can help patients with brain tumors that don’t respond to radiation therapy.
Combining Radiation with Other Treatments: Effects on Shrinkage Timeline
When treating brain tumors, using radiation therapy with other treatments can change how fast tumors shrink. This method, called combination therapy, is key in treating many brain tumors. It lets doctors create treatment plans that fit each patient’s needs, which can lead to better results.
Radiation with Chemotherapy
Using radiation therapy with chemotherapy is a common treatment for some brain tumors. Chemotherapy makes tumor cells more likely to be damaged by radiation. This combo can help tumors shrink faster and improve survival rates in some patients.
For example, glioblastoma treatment often includes chemotherapy like temozolomide with radiation. The timing and order of chemotherapy and radiation can affect how well the treatment works. It depends on the tumor type, grade, and the patient’s health.
Radiation with Immunotherapy
Immunotherapy, which uses the body’s immune system to fight cancer, is being tested with radiation therapy for brain tumors. Radiation can help immunotherapy work better by releasing tumor antigens and making the tumor more vulnerable to immune attacks.
Early trials show promising results for some brain tumors treated with radiation and immunotherapy. For instance, checkpoint inhibitors, a type of immunotherapy, have been used with radiation for brain metastases. This combo has shown better local control and sometimes systemic responses.
Radiation with Targeted Therapies
Targeted therapies, which target specific molecular changes in tumor cells, are also being used with radiation therapy. This aims to kill more tumor cells while protecting normal tissues.
In patients with brain tumors and specific genetic mutations, targeted therapies can be used with radiation. For example, using BRAF inhibitors with radiation for BRAF-mutant gliomas is being studied.
By combining radiation therapy with chemotherapy, immunotherapy, and targeted therapies, we can make cancer treatment more effective. The choice of combination therapy depends on the tumor type, grade, and the patient’s health.
Managing Expectations: What Patients Should Know
The journey to recovery after radiation therapy for brain tumors is complex. It’s important to set realistic expectations. Patients and their families often have many questions about the treatment and how long it will take for the tumor to shrink.
Setting Realistic Timelines for Response
It’s key to understand what affects how fast a tumor shrinks. This includes the tumor’s type and grade, its size and location, and the patient’s health and past treatments.
| Factor | Description | Impact on Shrinkage Timeline |
| Tumor Type and Grade | Different tumors respond differently to radiation therapy. | High-grade tumors may respond quickly but have a higher chance of recurrence. |
| Tumor Size and Location | Larger tumors or those in critical areas may require more time to show significant shrinkage. | Tumors in sensitive areas may require more cautious treatment approaches. |
| Patient Health | Patients with overall good health tend to respond better to treatment. | Better health can lead to a more favorable response to radiation therapy. |
Communicating with Your Healthcare Team
Talking openly with your healthcare team is vital. It helps manage expectations and understand the treatment process. Patients should ask about their prognosis, the expected timeline for tumor shrinkage, and any concerns they have.
Patients should keep communication lines open with their healthcare providers. This ensures they are well-informed about their treatment plan and any necessary adjustments.
Side Effects During the Tumor Shrinkage Process
Radiation therapy can shrink brain tumors but also causes side effects. It’s important to know about these side effects. This helps manage them and improves life quality during treatment.
Early Side Effects
Early side effects happen during or right after treatment. They include fatigue, headaches, and nausea. Fatigue is common as the body reacts to the radiation. Headaches might come from swelling or inflammation.
Delayed Side Effects
Delayed side effects show up months after treatment ends. They include cognitive changes, hair loss, and hormonal imbalances. Cognitive changes can affect memory and concentration. Hair loss happens if the scalp is in the radiation field.
Hormonal imbalances can occur if the radiation hits the pituitary gland or other endocrine parts.
Managing Side Effects
Managing side effects well is vital for a good quality of life during and after treatment. This involves medical treatments, lifestyle changes, and supportive care. For example, medicines can help with nausea and headaches.
Lifestyle adjustments like rest, a balanced diet, and staying hydrated are also important. We help patients create a plan to manage side effects. This ensures they get the best care during their treatment.
Long-term Outcomes and Survival Rates
Brain tumor patients’ long-term outcomes and survival rates depend on many factors. These include the tumor type and grade, treatment success, and patient health. Knowing these factors helps set realistic hopes and make informed care choices.
It’s key to understand how tumor shrinkage rates relate to prognosis. Also, long-term monitoring after treatment is vital.
Correlation Between Shrinkage Rate and Prognosis
The speed at which a brain tumor shrinks after radiation therapy gives clues about the patient’s future. Faster shrinkage often means a better outcome. But, the link between shrinkage rate and prognosis is complex. It’s influenced by:
- Tumor Type and Grade: Different tumors react differently to radiation.
- Tumor Size and Location: The tumor’s size and where it is can impact treatment success and prognosis.
- Patient-Specific Factors: Age, health, and genetics can affect how well a patient responds to treatment.
Research shows that some brain tumors, like meningiomas, have better outcomes than others, like glioblastomas.
Long-term Monitoring After Successful Treatment
Keeping an eye on patients long-term is critical. It helps catch any tumor comebacks and manage treatment side effects. Regular check-ups and scans, like MRI, are key.
How often scans are needed depends on the tumor type, patient health, and treatment plan. Usually, scans are done every 3-6 months for a few years after treatment.
Good long-term monitoring lets doctors:
- Detect Recurrence Early: Finding tumors early can lead to better treatment results.
- Manage Late Effects: Treatment side effects, like cognitive changes, can be managed.
- Adjust Treatment Plans: Treatment plans can be changed based on patient response and side effects.
Understanding brain tumor treatment outcomes helps patients and families. It aids in navigating care complexities and making informed decisions.
Recent Advances in Radiation Technology and Tumor Response Assessment
New breakthroughs in radiation oncology are making brain tumor treatments better. These advances improve how we target tumors and check how well they respond to treatment.
Emerging Technologies in Radiation Delivery
Recent years have brought big changes in radiation technology, including:
- Intensity-Modulated Radiation Therapy (IMRT): This method targets tumors more precisely, protecting healthy tissue.
- Stereotactic Body Radiation Therapy (SBRT): It gives high doses of radiation to small, well-defined tumors with high accuracy.
- Proton Therapy: This technology delivers radiation more precisely, reducing harm to nearby tissues.
These technologies are key to better treatment results for brain tumor patients.
New Methods for Evaluating Treatment Response
New ways to check how tumors respond to treatment are being developed:
- Advanced Imaging Techniques: Functional MRI and PET scans give detailed info on tumor metabolism and treatment response.
- Radiomics: This involves analyzing lots of data from medical images to forecast treatment outcomes.
- Liquid Biopsy: A non-invasive test that finds tumor DNA in the blood, showing treatment response.
These new technologies and methods are changing radiation oncology. They help create more effective treatments and better care for patients.
Case Studies: Real Patient Experiences with Tumor Shrinkage
Studies on patients with brain tumors treated with radiation show different results. These stories help doctors make treatment plans that fit each patient’s needs.
| Tumor Type | Average Shrinkage Rate | Time to Significant Shrinkage |
| Glioblastoma | 40-60% | 6-12 weeks |
| Meningioma | 50-70% | 3-6 months |
Delayed Response Cases
Not every patient sees their tumor shrink fast. Some may see it shrink slowly over months after treatment.
A case study showed a patient with a metastatic brain tumor. Their tumor shrank by 75% over nine months after treatment.
Slow responses can be due to many things. This includes the tumor’s nature and how the patient reacts to treatment. Knowing this helps doctors manage patient hopes and plan better treatments.
Looking at both fast and slow responses helps doctors understand tumor shrinkage better. This knowledge leads to better treatments and outcomes for patients.
Conclusion: The Journey of Brain Tumor Treatment and Recovery
Knowing how long it takes for brain tumors to shrink after radiation is key. We’ve looked at what affects this, like the tumor type and how the radiation is given. We also talked about how the patient’s health matters.
Good treatment for brain tumors means using radiation, watching the tumor, and supporting the patient. Knowing the patient’s journey helps doctors give care that fits each person. This can lead to better results and recovery.
As we get better at radiation and treatment plans, teaching patients is vital. This way, they can face their treatment with hope. It makes their recovery better.
FAQ
How long does it typically take for a brain tumor to shrink after radiation therapy?
The time it takes for a brain tumor to shrink after radiation therapy varies. It depends on the tumor’s type, size, and location. Also, the radiation therapy method used is important. Some tumors may start shrinking in a few weeks or months.
What are the different radiation therapy approaches used to treat brain tumors, and how do they impact the tumor shrinkage timeline?
There are several ways to treat brain tumors with radiation. These include conventional external beam radiation, stereotactic radiosurgery (SRS), and proton therapy. Each method has its own benefits and is chosen based on the tumor and patient’s health.
How is tumor shrinkage monitored after radiation therapy, and what imaging techniques are used?
Doctors use MRI and other scans like CT or PET to check if tumors are shrinking. How often these scans are done depends on the tumor type and treatment plan. Radiologists look at changes in size and shape to see how well the treatment is working.
What is pseudo-progression, and how is it differentiated from a true response to treatment?
Pseudo-progression is when a tumor looks like it’s growing after treatment, but it’s actually responding. It’s hard to tell the difference. Doctors use special imaging and clinical checks to figure it out.
Can combining radiation therapy with other treatments, such as chemotherapy or immunotherapy, affect the tumor shrinkage timeline?
Yes, using radiation with other treatments can change how fast a tumor shrinks. The exact effect depends on the tumor and the treatment plan. Combining therapies can sometimes lead to better results.
What are the possible side effects during the tumor shrinkage process, and how can they be managed?
Side effects like fatigue, hair loss, and radiation necrosis can happen. It’s important to manage these to keep patients’ quality of life good. Healthcare teams work with patients to find ways to reduce these effects.
How do primary and metastatic brain tumors differ in their response to radiation therapy?
Primary brain tumors, like gliomas, may take longer to respond to treatment. Metastatic tumors can respond faster. Knowing these differences helps doctors plan the best treatment.
What is radiation resistance, and what are the treatment options for radiation-resistant tumors?
Radiation resistance means a tumor doesn’t react to radiation therapy. There are complex reasons for this. Treatment options might include different radiation methods, chemotherapy, or other therapies.
How can patients manage their expectations regarding the tumor shrinkage timeline?
It’s key to have realistic expectations for treatment results. Patients should talk to their healthcare team to understand what to expect. This helps with treatment success and patient satisfaction.
What are the long-term outcomes and survival rates for patients with brain tumors, and how do they correlate with the rate of tumor shrinkage?
Survival rates for brain tumor patients vary based on several factors. These include the tumor type, size, and location, and the treatment plan. The rate of tumor shrinkage can also be a clue to how well the treatment is working. Long-term monitoring is important to catch any signs of recurrence.
References
National Center for Biotechnology Information. Survival Following Whole Brain Radiation for Brain Metastases. Retrieved from
https://pmc.ncbi.nlm.nih.gov/articles/PMC6088331/