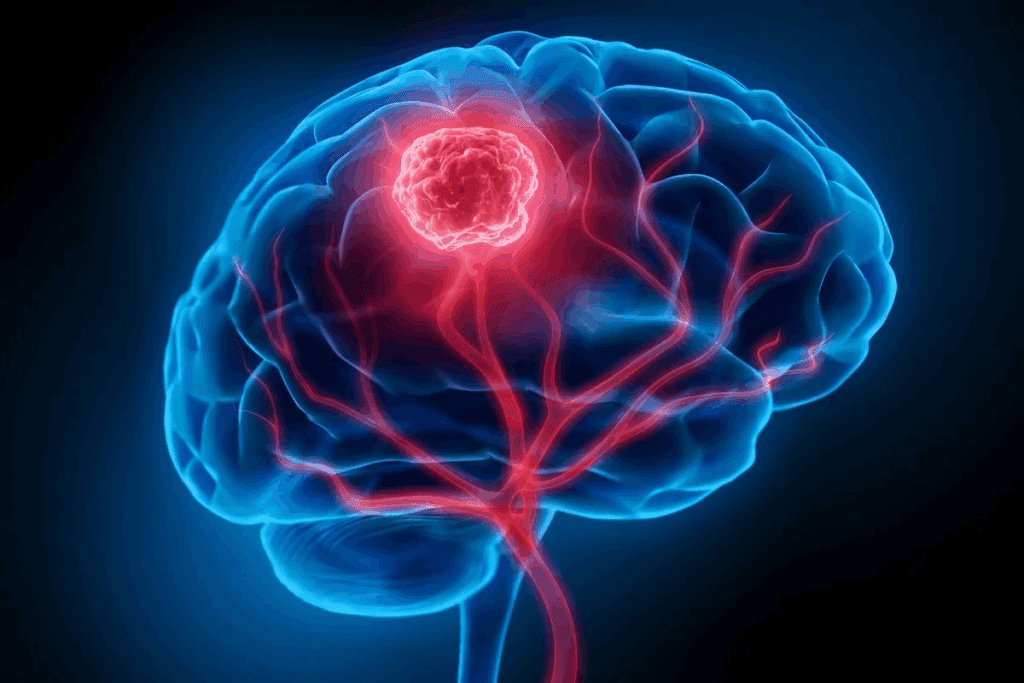
Nearly 28,000 Americans are diagnosed with brain tumors each year. Many need surgery to treat them. Craniotomy is a serious surgery that removes part of the skull to reach the brain. It’s a big worry for many.Learn what is a craniotomy. Understand the seriousness of brain surgery to remove a tumor and the associated risks clearly.
A craniotomy for tumor removal is very precise. Our team works hard to care for you from start to finish. Knowing about brain tumor surgery shows the skill and kindness needed to do it right.
Key Takeaways
- Craniotomy is a surgical procedure that involves temporarily removing a portion of the skull.
- Brain tumor surgery is a complex operation requiring great precision.
- Understanding the process can help alleviate concerns for patients and families.
- Comprehensive care is key for good results in brain surgery.
- Expertise in neurosurgery is vital for effective tumor removal.
Brain Tumors: Types, Causes, and Diagnosis

Brain tumors are abnormal cell growths in the brain. They can be benign or cancerous. Understanding the different types, causes, and diagnosis is key for patients and their families.
Common Types of Brain Tumors
Brain tumors can be primary or metastatic. Primary tumors start in the brain. Metastatic tumors spread to the brain from other parts. Here are some common primary brain tumors:
- Meningioma: Typically benign tumors arising from the meninges, the protective membranes around the brain.
- Glioma: Tumors that arise from the brain’s glial cells, ranging from low-grade to high-grade (glioblastoma).
- Pituitary Adenoma: Tumors of the pituitary gland, often benign and affecting hormone production.
How Do You Get a Brain Tumor?
The exact cause of most brain tumors is unknown. But, some risk factors are known. For example:
- Genetic predisposition: Conditions like neurofibromatosis or Li-Fraumeni syndrome increase the risk.
- Radiation exposure: Previous radiation therapy, specially in childhood, is a risk factor.
Diagnostic Process and Imaging
Diagnosing a brain tumor involves imaging studies and sometimes a biopsy. Key tools include:
| Diagnostic Tool | Description | Use in Brain Tumor Diagnosis |
| MRI (Magnetic Resonance Imaging) | Provides detailed images of the brain using magnetic fields. | Primary tool for visualizing tumor size, location, and characteristics. |
| CT Scan (Computed Tomography) | Uses X-rays to create images of the brain. | Quick and useful for detecting hemorrhage or calcification within tumors. |
| Biopsy | Involves taking a sample of tumor tissue for pathological examination. | Definitive diagnosis of tumor type and grade. |
What Is a Craniotomy? Procedure Overview and Definition

A craniotomy is a complex surgery that opens the skull to reach the brain. Neurosurgeons do this to treat brain issues like tumors, aneurysms, and injuries.
Craniotomy Meaning and Medical Definition
A craniotomy is a surgery where part of the skull is removed temporarily. This lets neurosurgeons access the brain. It’s a key operation for many brain conditions.
People often look up the craniotomy meaning to understand this surgery better. It helps them grasp what’s happening during the operation.
When Is a Craniotomy Necessary?
A craniotomy is needed for serious brain issues. These include brain tumors, bleeding in the brain, or severe head injuries. Doctors decide on a craniotomy after careful evaluation and tests.
They use MRI or CT scans to make this decision. The choice depends on the brain lesion’s location and size, the patient’s health, and the surgery’s benefits and risks.
Different Types of Craniotomy Procedures
There are many craniotomy procedures, each for different needs:
- Standard Craniotomy: Removes a part of the skull to access the brain.
- Keyhole Craniotomy: Uses a small incision and opening for a less invasive approach.
- Awake Craniotomy: Done while the patient is awake to monitor brain functions.
Each procedure has its own use and benefits. The right choice depends on the condition and the patient’s needs.
The Surgical Team: What Is a Brain Surgeon Called?
A brain surgeon, or neurosurgeon, is key in removing brain tumors. They have to be very skilled and precise. This is because brain surgery is very complex.
Neurosurgeons: Training and Specialization
Neurosurgeons focus on the brain and nervous system. They go through a lot of training. This includes:
- Completing medical school
- Residency programs in neurosurgery
- Often, additional fellowship training in specialized areas like brain tumor surgery
The American Association of Neurological Surgeons says neurosurgeons must keep learning. This helps them use the newest techniques and technologies.
“The complexity of brain surgery demands not only technical skill but also a deep understanding of the brain’s intricacies.”
The Multidisciplinary Brain Surgery Team
Brain surgery is not just about the neurosurgeon. A team of experts is needed for the best care:
| Team Member | Role |
| Neurosurgeon | Performs the surgery |
| Neuroanesthesiologist | Administers anesthesia and monitors patient vitals during surgery |
| Neurologist | Assists in diagnosis and post-operative care |
| Radiologist | Provides imaging studies for surgical planning |
| Nurses and Rehabilitation Specialists | Offer pre- and post-operative care, including rehabilitation |
How to Choose the Right Neurosurgeon
Finding the right neurosurgeon is very important. Here are some tips:
- Experience: Choose neurosurgeons with lots of experience in brain tumor surgery.
- Credentials: Make sure they are board certified and part of professional groups.
- Patient Reviews: Check what other patients say about them.
- Hospital Affiliation: Make sure they work at good hospitals with the latest equipment.
It’s a good idea to talk to several neurosurgeons. This way, you can find the one that makes you feel most comfortable and confident.
Meningioma Surgery: Special Considerations
Surgery for meningiomas needs special care because of where they grow and what they are. These tumors grow slowly and are usually not cancerous. But, they can be tricky to remove because they are near important parts of the brain.
Meningioma Operation Techniques
Doctors have developed new ways to remove meningiomas without harming the brain. They use microsurgery and endoscopic surgery. The choice depends on the tumor’s size, where it is, and the patient’s health.
Microsurgery uses a microscope for detailed work. Endoscopic surgery uses a camera and tools through a small cut. This way, the tumor can be removed with less damage.
Frontal Lobe Meningioma Surgery Approach
Removing meningiomas in the frontal lobe is very careful. The tumor is close to important brain areas. Doctors use special imaging to plan the surgery carefully.
The key to successful meningioma surgery lies in meticulous planning and precise execution. By understanding the tumor’s characteristics and its relationship to surrounding brain structures, neurosurgeons can optimize outcomes for patients.
Meningioma Removal Success Rates
Most people who have meningioma surgery get better or feel much better. How well the surgery goes depends on the tumor’s size, where it is, and how aggressive it is.
| Tumor Location | Success Rate | Recurrence Rate |
| Convexity | 90% | 10% |
| Skull Base | 80% | 15% |
| Parasagittal | 85% | 12% |
In conclusion, meningioma surgery needs a lot of planning and skill. Knowing about the different ways to operate and how successful the surgery can be helps patients understand their treatment better.
Pre-Surgical Evaluation and Planning
The pre-surgical evaluation phase is key for checking the patient’s condition and planning the surgery. It involves a detailed assessment to make sure the surgical team is ready for the procedure.
Essential Imaging Studies
Imaging studies are very important in planning the surgery. We use MRI and CT scans to get detailed info about the tumor. This info helps us plan the best surgical approach.
Functional Brain Mapping
Functional brain mapping is a big part of the pre-surgical evaluation. It’s very important for tumors in important brain areas. This method helps us find out which brain areas are critical, like speech and vision. It helps us plan the surgery to avoid damage.
Patient Selection and Risk Assessment
Picking the right patient and assessing risks are key parts of the pre-surgical process. We look at the patient’s health, medical history, and the tumor details. This helps us create a personalized surgical plan and talk about possible risks and benefits.
By carefully checking the patient’s condition and planning the surgery, we can greatly improve brain tumor surgery outcomes. Our team works together to give each patient the best care possible.
The Craniotomy Procedure Steps in Detail
A craniotomy is a complex surgery to remove brain tumors. It involves several key steps that neurosurgeons must follow carefully. Knowing these steps can help patients understand what to expect.
Anesthesia Administration
The first step is giving anesthesia. General anesthesia keeps the patient comfortable and pain-free. Our anesthesiologists watch the patient’s vital signs and adjust the anesthesia as needed.
Surgical Access: Opening the Skull
With the patient under anesthesia, the team opens the skull. They make an incision in the scalp and move the skin to show the skull. A craniotome is used to remove a part of the skull, creating a flap for brain access.
Tumor Resection Techniques
With the skull open, the neurosurgeon finds and removes the tumor. Microsurgical techniques and intraoperative imaging help remove as much tumor as possible while saving brain tissue.
Skull Replacement and Closure
After removing the tumor, the team puts the skull flap back. They use titanium plates or sutures to secure it. Then, they close the skin with sutures or staples. This step is key for healing and restoring the skull’s integrity.
Our team of neurosurgeons, anesthesiologists, and nurses work together for the best patient outcome. By knowing the steps of this surgery, patients can feel more informed and ready for their treatment.
Are You Awake During Brain Surgery?
Awake brain surgery, or awake craniotomy, is a complex technique. It lets neurosurgeons work while the patient is awake. This method is key for surgeries near brain areas that control speech, movement, and feeling.
When Awake Craniotomy Is Recommended
Doctors often suggest awake craniotomy for patients with brain tumors or epilepsy near important brain areas. These areas handle vital functions. By keeping the patient awake, the team can watch brain functions closely, lowering damage risks.
Choosing awake craniotomy depends on many factors. These include the patient’s health, tumor location and size, and their ability to follow instructions during surgery.
| Condition | Awake Craniotomy Benefit |
| Tumor near eloquent brain areas | Real-time monitoring of neurological functions |
| Epilepsy surgery | Precise localization of seizure foci |
| Patient’s ability to cooperate | Better outcomes due to patient feedback during surgery |
The Patient Experience During Awake Brain Surgery
Being awake during surgery might seem scary, but patients are given sedation to relax. They are awake but comfortable, with the area numbed to avoid pain.
“The experience was surprisingly manageable. I was nervous at first, but the medical team was very reassuring. I could respond to their requests during the surgery, which made me feel more in control.” – A patient who underwent awake craniotomy
Patients can talk to the team during the surgery. This is key for success, when working near critical brain spots.
Does Awake Brain Surgery Hurt?
Many worry about pain during awake brain surgery. But, the area is numbed with local anesthesia, so patients don’t feel pain.
Some might feel discomfort or pressure, but it’s usually manageable. The team keeps a close eye on the patient’s comfort and adjusts sedation as needed.
In summary, awake craniotomy is a safe and precise procedure. It offers significant benefits for the right patients. It requires careful selection and a skilled team.
Brain Tumor Surgery Tools and Technology
Brain tumor surgery has become more advanced with new tools and technology. These improvements have made treatments more precise and effective. This has led to better results for patients.
Standard Neurosurgical Instruments
Neurosurgeons use many tools for brain tumor surgeries. These include:
- Magnifying glasses or microscopes for detailed visualization.
- Specialized surgical tools such as scalpels, forceps, and retractors designed for delicate brain tissue.
- Electrosurgical units for cutting and coagulation.
These tools are key to successful brain tumor surgery. They help remove tumors precisely, protecting the brain around it.
Advanced Imaging During Surgery
Modern brain tumor surgery relies on advanced imaging. Techniques like:
- Intraoperative MRI let surgeons check how much tumor is removed during surgery.
- Fluorescence-guided surgery using agents like 5-ALA helps see tumor edges.
These technologies make tumor removal more precise. They also improve treatment results.
Endoscopic Brain Surgery Equipment
Endoscopic methods are becoming more common in brain tumor surgery. They offer a less invasive way to operate. The equipment includes:
- High-definition endoscopes for clear views.
- Specialized endoscopic instruments for removing tumors.
Endoscopic brain surgery can lead to faster recovery and less scarring. It’s a good option for some brain tumors.
We keep seeing new tools and technology for brain tumor surgery. These advancements help us treat these complex conditions more effectively.
Craniotomy Risks and Possible Complications
Craniotomy is a lifesaving surgery, but it comes with risks and complications. Like any major surgery, it has risks that can affect how well a patient does.
Short-Term Surgical Complications
Short-term issues after a craniotomy might include:
- Infection at the surgical site
- Bleeding or hemorrhage
- Swelling or edema in the brain
- Seizures or convulsions
- Reaction to anesthesia
These problems can be managed with the right medical care. It’s important for patients to be watched closely after surgery.
Long-Term Neurological Risks
Long-term brain risks from craniotomy can be:
- Cognitive changes or memory issues
- Seizure disorders
- Motor or sensory deficits
- Personality changes
These risks depend on the surgery’s location and extent, and the patient’s health.
Craniotomy Survival Rate
The survival rate for craniotomy patients depends on several things. These include the condition being treated, the patient’s health, and the surgeon’s skill. While statistics give a general idea, each person’s outcome can be different.
Important factors for craniotomy survival rate are:
- The nature and severity of the underlying condition
- Patient’s age and overall health
- Surgical team’s experience and skill level
- Quality of post-operative care
Knowing these factors helps patients and their families make better decisions about their care.
Craniotomy Recovery: What to Expect
Craniotomy recovery is a complex process. It includes immediate care, scar healing, and rehabilitation. Knowing what to expect can help patients and their families prepare.
Immediate Post-Operative Care
After a craniotomy, patients are watched closely in the ICU. Close monitoring helps manage pain and watch for neurological issues.
Immediate care focuses on:
- Managing pain effectively
- Monitoring for signs of infection or neurological changes
- Maintaining proper wound care
- Gradually mobilizing the patient to prevent complications like deep vein thrombosis
Craniotomy Scar Healing Process
Scar healing after a craniotomy varies. The scar may start red and swollen but will gradually fade and become less noticeable over time.
To help with scar healing:
- Follow the surgeon’s instructions for wound care
- Keep the scar area clean and dry
- Avoid direct sun exposure on the scar
- Use recommended topical treatments to aid healing
Physical and Cognitive Rehabilitation
Rehabilitation after a craniotomy is key. It helps regain strength and improve cognitive function. A comprehensive rehabilitation plan may include physical, occupational, and speech therapy.
Timeline for Returning to Normal Activities
The time it takes to return to normal activities varies. It depends on the patient’s health, surgery complexity, and any complications.
| Recovery Stage | Typical Timeline | Activities |
| Immediate Recovery | 1-2 weeks | Rest, limited mobility |
| Early Rehabilitation | 2-6 weeks | Gradual mobilization, light activities |
| Advanced Rehabilitation | 6-12 weeks | Increased physical activity, returning to work |
We know each patient’s recovery is unique. Our team is dedicated to providing personalized care and support.
Brain Tumor Size and Survival Rates
The size of a brain tumor greatly affects a patient’s survival rate and prognosis. It’s key for both patients and doctors to understand this. This knowledge helps in making the best treatment choices.
Survival Rates for Small Brain Tumors
A 2 cm brain tumor is considered small. Survival rates for these tumors vary a lot. This depends on the tumor type, where it is, and the patient’s health.
Smaller tumors usually mean better chances of survival. This is because they are caught early and treated less invasively.
For example, a study on meningiomas found that tumors under 2 cm have a much higher survival rate. We’ll dive into these numbers to see what they mean for patients.
Survival Rates for Larger Brain Tumors
A 4 cm brain tumor is larger and more challenging to treat. Survival rates for these tumors are generally lower. This is because they can damage more brain tissue.
But, new surgical and treatment methods have helped. We’ll look at the latest survival rate data for 4 cm tumors. We’ll also talk about what affects these outcomes.
Factors Affecting Long-Term Prognosis
While tumor size is important, it’s not the only factor. Other things that greatly affect long-term survival include:
- Tumor Type: Benign tumors usually have better outcomes than malignant ones.
- Tumor Location: Tumors in easier-to-reach spots may have better surgery results.
- Patient’s Overall Health: Patients with fewer health issues tend to live longer.
- Treatment Approach: Using surgery, radiation, and chemotherapy together can lead to better results.
It’s vital to understand these factors and how they work together. This knowledge helps in creating effective treatment plans. As we keep improving in neuro-oncology, brain tumor patients’ chances of survival keep getting better.
How Much Does Brain Surgery Cost?
It’s important for patients to know the cost of brain surgery before they decide. The cost can be high, and it’s good to understand what makes it so.
Average Brain Tumor Surgery Cost in the United States
The cost of brain tumor surgery in the U.S. changes a lot. It depends on where you are, the hospital, and how complex the surgery is. Costs can be anywhere from $80,000 to over $200,000.
| Procedure Component | Average Cost |
| Surgical Fees | $30,000 – $60,000 |
| Hospital Stay | $20,000 – $50,000 |
| Anesthesia | $1,000 – $3,000 |
| Imaging and Tests | $5,000 – $10,000 |
| Rehabilitation | $5,000 – $20,000 |
Insurance Coverage for Craniotomy
Most insurance plans cover brain surgery. But, how much they cover can differ a lot. It’s key to check your policy to know what you’ll pay for.
Key factors affecting insurance coverage include:
- The type of insurance plan
- The specific policy details
- The medical necessity of the procedure
Financial Assistance Programs
If you’re worried about the cost, there are help programs out there. These include government aid, non-profit groups, and financial help from hospitals.
It’s a good idea to look into these options. They can help make brain surgery more affordable.
Alternative Approaches to Brain Tumor Treatment
There are many ways to treat brain tumors, not just surgery. Other treatments can be used alone or with surgery to help patients. This can lead to better outcomes.
Radiation Therapy Options
Radiation therapy is a common treatment for brain tumors. It uses high-energy particles or waves to kill cancer cells. There are several types, including:
- External Beam Radiation Therapy (EBRT): This is the most common type. It sends radiation from outside the body to the tumor.
- Stereotactic Radiosurgery (SRS): This is not surgery but a precise radiation therapy. It gives a high dose of radiation to a specific area.
- Brachytherapy: This involves placing radioactive material directly into or near the tumor.
Radiation therapy can treat many brain tumors. It’s used for tumors that can’t be removed or have come back after surgery.
Chemotherapy Protocols
Chemotherapy is another option for brain tumors. It uses drugs to kill or slow cancer cells. The drugs can be taken by mouth or given through an IV, depending on the tumor type.
Some common chemotherapy drugs for brain tumors include:
- Temozolomide: This is often used for glioblastoma.
- Bevacizumab: This drug is for glioblastoma that has come back. It stops tumors from growing by blocking new blood vessels.
Chemotherapy can be used alone or with other treatments like radiation therapy.
Emerging Treatments and Clinical Trials
New treatments for brain tumors are being researched. Some promising therapies include:
- Immunotherapy: This uses the immune system to fight cancer. Various immunotherapies are being studied for brain tumors, including checkpoint inhibitors and cancer vaccines.
- Targeted Therapy: These drugs target specific molecules in cancer cells. They are being tested for treating brain tumors with fewer side effects than traditional chemotherapy.
- Gene Therapy: This involves introducing genes into cancer cells to make them more treatable or to kill them directly.
Clinical trials are key for testing these new treatments. They help find out if these treatments are safe and effective. Patients with brain tumors might be able to join clinical trials, giving them access to new therapies.
By exploring these options, doctors can create treatment plans that fit each patient’s needs. This helps patients get the best care possible for their brain tumors.
Interesting Facts About Brain Surgery
Brain surgery has a rich and fascinating history. It has led to significant advancements in medical science. Exploring brain surgery reveals the remarkable journey of its evolution.
Historical Evolution of Craniotomy
The history of craniotomy goes back thousands of years. Ancient cultures practiced trephining, a form of skull surgery. This early technique involved removing a portion of the skull to relieve pressure or treat injuries.
Today, craniotomy has evolved significantly. Modern techniques allow for precise and safe surgical interventions.
Some key milestones in the evolution of craniotomy include:
- The development of antiseptic practices, significantly reducing infection rates
- The introduction of imaging technologies like MRI and CT scans, enabling better pre-surgical planning
- Advances in surgical instruments and techniques, such as microsurgery and endoscopy
Notable Brain Surgery Cases
Throughout history, there have been several notable brain surgery cases. One such case is Phineas Gage, who in 1848 survived a severe brain injury. This incident has been extensively studied, providing valuable insights into the relationship between the brain and behavior.
More recently, advancements in neurosurgery have led to successful surgeries in complex cases. These include:
- Awake craniotomies, where patients remain conscious during parts of the surgery
- Minimally invasive procedures, reducing recovery time and scarring
- Surgery on deep-seated brain tumors, previously considered inoperable
Future Directions in Neurosurgery
The future of neurosurgery is promising. Ongoing research and technological advancements are paving the way for new treatments and improved outcomes. Some exciting developments include:
- Personalized medicine, tailoring treatments to individual patient profiles
- Advanced imaging and navigation systems, improving surgical precision
- Robotics and artificial intelligence, potentially revolutionizing surgical techniques
As we continue to push the boundaries of what is possible in brain surgery, we remain committed to delivering the highest level of care to our patients. The future of neurosurgery is bright, and we look forward to the advancements that will continue to improve patient outcomes.
Conclusion: Understanding the Seriousness of Brain Tumor Surgery
Brain tumor surgery, like craniotomy, is a complex and serious medical procedure. We’ve looked at the different types of brain tumors and how they are diagnosed. We also explored the details of the craniotomy procedure and the role of neurosurgeons.
The seriousness of craniotomy is clear. It involves opening the skull to remove a tumor. If not done right, it can be life-threatening. It’s important for patients and their families to understand the risks and the need for a skilled neurosurgical team.
We’ve talked about the key role of advanced medical technology and thorough pre-surgery and post-operative care. This ensures the best outcomes for patients. By covering all these aspects, we aim to give patients the knowledge they need to face this challenging experience.
FAQ
What is a craniotomy?
A craniotomy is a surgery where part of the skull is taken off to reach the brain. This is often done to remove tumors or fix aneurysms.
Are you awake during brain surgery?
Yes, sometimes patients are awake during brain surgery. This is called an awake craniotomy. It helps surgeons see how the brain works and avoid harming important areas.
How serious is brain surgery to remove a tumor?
Removing a brain tumor is a serious surgery. It has risks, but it can save lives and greatly improve life quality for many.
What are the risks and complications of craniotomy?
Craniotomy risks include infection, bleeding, stroke, seizures, and brain damage. These are serious complications.
How long does it take to recover from a craniotomy?
Recovery time after a craniotomy varies. It can take weeks to months, depending on the surgery’s complexity and the patient’s health.
What is the cost of brain surgery?
Brain surgery costs vary a lot. They depend on where you are, your insurance, and how complex the surgery is.
What are the alternative approaches to treating brain tumors?
Other ways to treat brain tumors include radiation, chemotherapy, and new treatments like immunotherapy and targeted therapy.
How does the size of a brain tumor affect survival rates?
Tumor size affects survival chances. Smaller tumors usually have better outcomes than larger ones.
What is the role of a neurosurgeon in brain surgery?
Neurosurgeons are key in brain surgery. They work with a team to plan and do the surgery. They aim for the best results for the patient.
What are the different types of craniotomy procedures?
There are many craniotomy types, like frontal and temporal lobe surgeries. Each has its own reasons and methods.
What is the difference between a craniotomy and a craniectomy?
A craniotomy removes part of the skull temporarily. A craniectomy removes it permanently.
Can brain tumors be removed completely?
Sometimes, brain tumors can be removed fully. But, it depends on the tumor’s type, location, and size.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31575389/























