Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 30% of all cancer diagnoses involve brain tumors. This makes surgery a key part of treatment.Learn the crucial success rate of brain tumor surgery. Understand how the type, grade, and location of the tumor influence outcomes clearly.
Dealing with brain tumor surgery can be scary. But, recent studies show that new surgical methods have greatly improved results for patients.
We’re dedicated to top-notch healthcare, including support for patients from abroad. Our team will help you from start to finish, guiding you through every step.
Key Takeaways
- Modern surgical techniques have improved outcomes for brain tumor patients.
- The success of brain tumor surgery depends on various factors, including tumor type and location.
- Our institution provides comprehensive support for international patients.
- Understanding the factors that influence surgical outcomes is key for patients and families.
- We’re committed to delivering world-class healthcare with personalized care.
Understanding Brain Tumors and Surgical Interventions
Brain tumors can greatly affect a person’s life. They are divided into two main types: benign and malignant. Knowing the type helps doctors plan the best treatment.
Types of Brain Tumors
Brain tumors come from different brain cells. Benign tumors grow slowly and don’t spread. But, they can cause problems because of where they are. Malignant tumors grow fast and spread, making them harder to remove.
Common brain tumors include:
- Meningiomas, which are usually benign and arise from the meninges, the protective membranes surrounding the brain.
- Glioma, a category that includes astrocytomas and glioblastomas, ranging from low-grade (less aggressive) to high-grade (more aggressive) tumors.
- Pituitary adenomas, benign tumors of the pituitary gland that can affect hormone production.
- Acoustic neuromas, benign tumors on the nerve connecting the inner ear to the brain, potentially affecting hearing and balance.
When Surgery is Recommended
Surgery is often the first choice for treating brain tumors. The decision to have surgery depends on the tumor’s type, size, and location. It also depends on the patient’s health and symptoms.
Surgery might be used with other treatments like radiation or chemotherapy. This approach is often needed for malignant tumors to increase treatment success.
Goals of Brain Tumor Surgery
The main goals of brain tumor surgery are:
- Tumor removal: Removing the tumor to ease symptoms and possibly cure the condition.
- Symptom relief: Reducing the tumor’s effects on the brain to improve the patient’s life.
- Diagnostic clarity: Getting tissue for tests to find the tumor type and plan further treatment.
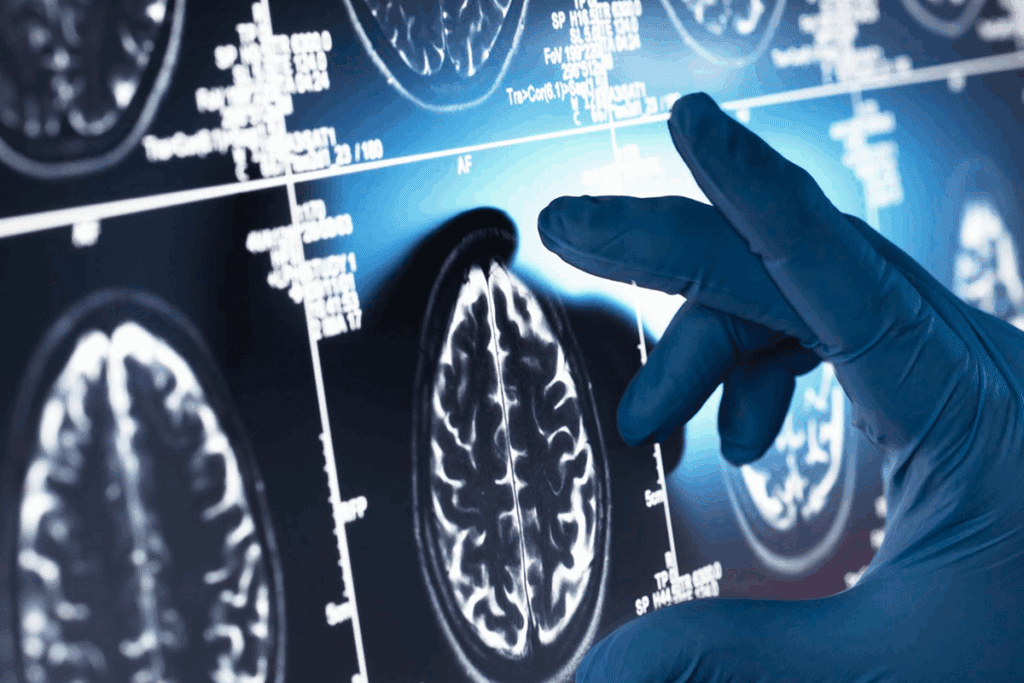
New techniques like neuronavigation and intraoperative imaging have made surgery safer and more precise. These tools help surgeons plan and perform complex surgeries better, improving patient results.
The Success Rate of Brain Tumor Surgery

The success of brain tumor surgery depends on many things. These include the type of tumor, where it is, and the patient’s health. It’s key to know what makes a surgery successful in neurosurgery.
Defining “Success” in Neurosurgical Outcomes
Success in brain tumor surgery means more than just removing the tumor. It also means keeping the patient’s brain function and improving their life quality. Complete resection of the tumor is a main goal. But, avoiding complications and helping the patient recover is just as important.
A study in the Journal of Neurosurgery says success in brain tumor surgery has changed. It now includes how well the patient functions and their quality of life, not just how much of the tumor is removed.
“The goal of brain tumor surgery is not just to remove the tumor, but to do so while preserving the patient’s neurological function and improving their overall survival and quality of life.”
General Statistics on Brain Tumor Surgery Outcomes
Statistics on brain tumor surgery outcomes give a general idea of what to expect. Modern surgery has greatly improved results for many patients. For example, a study found that survival rates have gone up thanks to better technology and care after surgery.
- Improved Survival Rates: Advances in surgery have led to better survival rates for many brain tumor patients.
- Reduced Complications: Modern techniques have minimized surgical complications.
- Better Quality of Life: Focus on preserving neurological function has improved patients’ quality of life post-surgery.
Measuring Short-term vs. Long-term Success
Measuring the success of brain tumor surgery looks at both short-term and long-term results. Short-term success is about how the patient does right after surgery. This includes how much of the tumor was removed and if there were any big problems. Long-term success looks at how long the patient lives, if the tumor comes back, and their quality of life over time.
- Short-term Success: Immediate post-surgery outcomes, including extent of resection and complication rates.
- Long-term Success: Patient survival, tumor recurrence rates, and long-term quality of life.
Knowing both short-term and long-term success rates helps set realistic hopes and guide care after surgery. As we keep improving in neurosurgery, we can do even better for brain tumor patients.
Benign Brain Tumor Surgery Success Rates
Benign brain tumors can really affect a person’s life. That’s why removing them surgically is so important. We’ll look at how well surgery works for different types of benign brain tumors.
Meningioma Surgical Outcomes
Meningiomas are tumors that grow on the meninges, which protect the brain and spinal cord. Most of the time, doctors remove them surgically. The good news is that many meningiomas can be fully removed.
Success rates for meningioma surgery depend on where the tumor is, how big it is, and the patient’s health. Tumors near important brain areas can be harder to remove completely.
- Most studies show that 80% to 90% of meningiomas can be removed fully.
- Less than 10% of meningiomas come back within 5 years.
Acoustic Neuroma Removal Success
Acoustic neuromas, or vestibular schwannomas, grow on the nerve from the inner ear to the brain. Surgery is a common treatment, aiming to save hearing and facial nerve function.
The success rate for removing acoustic neuromas is high. But, the surgery’s complexity depends on the tumor’s size and where it is.
- Most patients have their facial nerves saved, with success rates over 90%.
- How well hearing is saved varies, from 50% to 80%, based on the tumor and surgery.
Pituitary Adenoma Surgical Results
Pituitary adenomas are tumors in the pituitary gland that can mess with hormone levels. Surgery, often through the nose, is a common treatment.
Success rates for pituitary adenoma surgery are good, with many patients seeing big improvements. The success depends on the tumor’s size, type, and the surgeon’s skill.
- 50% to 80% of patients see their hormone levels get back to normal.
- Most patients have few complications and see big improvements.
The success rates for benign brain tumor surgery are promising. Advances in neurosurgery and technology are helping patients get better results.
Malignant Brain Tumor Surgical Outcomes
It’s important to know about the results of surgery for malignant brain tumors. These include glioblastoma, anaplastic astrocytoma, and metastatic brain tumors. Each one poses different challenges for neurosurgeons.
We will look at the results of surgery for these tumors. We’ll see how modern techniques help and what affects success rates.
Glioblastoma Surgery Success Rates
Glioblastoma is a very aggressive brain cancer. Surgery is a main treatment. Thanks to new techniques, outcomes have gotten better.
Success rates for glioblastoma surgery are improving. Studies show that removing most of the tumor can help patients live longer. New methods like microsurgery and neuronavigation make it easier to remove tumors precisely.
| Surgical Outcome | Glioblastoma | Anaplastic Astrocytoma | Metastatic Brain Tumor |
| Gross Total Resection Rate | 60-80% | 70-90% | 80-95% |
| Median Survival | 12-18 months | 24-36 months | Varies based on primary tumor |
Anaplastic Astrocytoma Surgical Results
Anaplastic astrocytoma is another aggressive brain tumor. Surgery is a key part of treatment. The results of surgery for this tumor are often better than for glioblastoma.
Factors influencing surgical success include how much of the tumor is removed and the tumor’s genetics. New surgical methods help surgeons remove more of the tumor, leading to better results for patients.
Metastatic Brain Tumor Removal Outcomes
Metastatic brain tumors come from cancers in other parts of the body. Surgery is a main treatment for some patients. The results of surgery depend on several things, like the original cancer and how many brain tumors there are.
Surgical benefits include feeling better and a better quality of life. Sometimes, surgery is used along with other treatments like radiation therapy to get even better results.
How Tumor Location Impacts Surgical Success
The place of a brain tumor is key to surgery success. Tumors in deep or important brain areas are harder to treat.
Superficial vs. Deep-seated Tumors
Superficial tumors are closer to the brain’s surface. They are easier to get to and remove. But, deep-seated tumors are harder to reach because they are buried deep in the brain.
Surgical Complexity: The deeper a tumor is, the harder the surgery. It’s because surgeons have to go around important brain parts. This increases the risk of brain damage.
Eloquent Brain Areas and Surgical Challenges
Tumors in areas that control important functions like speech and movement are tough to remove. Surgeons must carefully remove the tumor without harming these areas.
Advanced Techniques: To tackle these issues, neurosurgeons use new methods. They might do surgery while the patient is awake or use special tools to find and save important brain parts.
Brainstem and Spinal Cord Tumor Surgery
Tumors in the brainstem or spinal cord are very hard to treat. These areas control vital functions, making surgery risky.
Specialized Approaches: Neurosurgeons use special methods for these tumors. They might combine surgery with other treatments like radiation or chemotherapy. This is because these areas are so delicate.
The Effect of Tumor Size on Surgical Outcomes
The size of a brain tumor greatly affects how well surgery goes. Looking into brain tumor surgery shows that tumor size is key. It decides how well the surgery will do.
Small Tumors and Complete Resection Rates
Small brain tumors, under 3 cm, usually get removed fully. Early detection is key to finding these tumors early. This lets surgeons act fast.
When tumors are small, they’re easier to take out. This lowers the chance of harming nearby brain tissue. The success rate for removing small tumors is high. Many patients face few problems after surgery.
Large Tumors and Surgical Complexity
Larger brain tumors are harder for surgeons to deal with. Tumors over 5 cm are big and tough to remove fully. The surgery gets more complex with bigger tumors. They often mix with important brain parts.
Removing big tumors needs special skills and careful planning. Even so, skilled neurosurgeons can get good results. But, there’s a higher risk of problems.
The Importance of Early Detection
Early detection is very important for brain tumor patients. Finding tumors early boosts the chance of a successful surgery. New imaging and screening tools help find tumors sooner.
It’s vital to see a doctor regularly and get help right away if symptoms show up. Early diagnosis helps surgery success and improves life quality for patients.
Patient Factors Influencing Brain Surgery Success
Many patient factors affect the success of brain surgery. It’s important for doctors and patients to know these factors. This helps in making the right treatment choices.
Age and Overall Health
A patient’s age and health are key in brain tumor surgery success. Younger patients with fewer health problems usually do better. We look at heart health, chronic conditions, and overall well-being before surgery.
- Younger Age: Tends to be associated with better recovery and survival rates.
- Fewer Comorbidities: Patients with fewer health issues generally have a lower risk of complications.
- Good Physical Condition: Enhances the body’s ability to recover from major surgery.
Neurological Status Before Surgery
The neurological status before surgery is very important. Patients with less brain damage tend to do better.
Before surgery, we check:
- Cognitive function and level of consciousness
- Motor and sensory function
- Presence of seizures or other neurological symptoms
This helps doctors plan the surgery to reduce risks and improve results.
Genetic and Molecular Markers
Genetic and molecular diagnostics help us understand brain tumors better. They help predict how well a patient will do. Some genetic markers show how aggressive a tumor is and how it might respond to treatment.
For example, some markers in glioblastomas affect treatment choices and how well a patient will do. We keep learning about these markers to improve care.
Modern Surgical Techniques Improving Outcomes
Modern surgery, like microsurgery and neuronavigation, is changing how we treat brain tumors. These new methods have greatly improved surgery results. They help patients recover better and get better care.
Microsurgery and Precision Approaches
Microsurgery is key in brain tumor surgery. It lets doctors remove tumors precisely without harming the brain. They use special tools and high-powered microscopes for exact dissection and removal of tumor tissue.
The benefits of microsurgery are:
- Less risk of brain damage
- Better tumor removal rates
- Better patient results
Neuronavigation and Intraoperative Imaging
Neuronavigation and intraoperative imaging have changed brain tumor surgery. These tools give real-time feedback during surgery. They help doctors find tumors accurately and navigate the brain’s complex structure.
Neuronavigation’s main benefits are:
- More accurate tumor location
- Lower risk of complications
- Better chance of removing the tumor completely
Awake Craniotomy for Functional Preservation
Awake craniotomy is a complex surgery that lets doctors remove tumors while the patient is awake. This method lets them watch brain function in real-time. It helps them keep important brain areas safe and lower the risk of brain problems after surgery.
The advantages of awake craniotomy are:
- Better brain function preservation
- Lower risk of brain problems after surgery
- Better recovery and quality of life for patients
Minimally Invasive Brain Tumor Surgery Success
Minimally invasive brain tumor surgery is changing how we treat brain tumors. It offers hope to patients by reducing risks and speeding up recovery. This method also helps protect the brain around the tumor.
Endoscopic Approaches
Endoscopic surgery uses a thin, flexible tube with a camera and light. It lets surgeons remove tumors through small cuts. This method is great for tumors near the brain’s surface or hard to reach.
One big plus of endoscopic surgery is less chance of infection and scarring. Patients often feel less pain and can get back to normal faster. But, how well it works depends on the tumor’s size and where it is.
Laser Interstitial Thermal Therapy (LITT)
LITT uses laser heat to kill tumor cells. A laser probe is inserted into the tumor under imaging. The heat kills the cells, which the body then absorbs.
LITT is good for deep tumors that are hard to get to with regular surgery. It’s precise and causes little damage to the brain. Clinical trials show it can shrink tumors and improve symptoms.
Stereotactic Radiosurgery as an Alternative
Stereotactic radiosurgery (SRS) is a non-surgical way to treat tumors. It uses precise radiation doses. It’s a good option for tumors that can’t be removed or are in sensitive areas.
| Treatment Option | Description | Benefits |
| Endoscopic Approaches | Minimally invasive surgery using a thin tube with a camera | Less risk of infection, reduced scarring, quicker recovery |
| LITT | Laser heat destroys tumor cells | Precise tumor destruction, minimal damage to surrounding tissue |
| Stereotactic Radiosurgery | High doses of radiation delivered with precision | Non-invasive, effective for inoperable or sensitive area tumors |
Each minimally invasive method has its own benefits and uses. The right treatment depends on the tumor’s type, size, and location, and the patient’s health.
In conclusion, new brain tumor surgery methods like endoscopic and LITT offer hope. Stereotactic radiosurgery is another non-surgical option. Success depends on choosing the right treatment and the neurosurgical team’s skill.
Multimodal Treatment Approaches and Success Rates
Multimodal treatment strategies are changing how we treat brain tumors. They combine different methods to improve patient outcomes and quality of life.
Neurosurgery has advanced, showing that one treatment doesn’t fit all. Multimodal treatment approaches include surgery, chemotherapy, radiation, and targeted and immunotherapy. They offer a more complete strategy.
Surgery Plus Chemotherapy Outcomes
Using surgery and chemotherapy together has shown great results. Chemotherapy can be used before or after surgery. It helps shrink the tumor or kill any remaining cancer cells.
Adding chemotherapy has been a big change in treating aggressive brain tumors. It shows how combining treatments can improve patient outcomes.
Surgery Plus Radiation Therapy Results
Radiation therapy is key in treating brain tumors. It helps control tumor growth and lower the chance of it coming back. New radiation techniques allow for more precise targeting, protecting the brain.
- Improved local control of tumor growth
- Reduced risk of recurrence
- Enhanced patient survival rates
Targeted and Immunotherapy Combinations
Targeted therapy and immunotherapy are new in treating brain tumors. They target specific molecules or boost the immune system against cancer. When used with surgery, they offer extra benefits for some patients.
The research on targeted and immunotherapy combinations is promising. As we learn more about brain tumors, we can make treatments more effective and personalized.
In summary, multimodal treatment approaches are making brain tumor surgery more successful. By using surgery with chemotherapy, radiation, and targeted and immunotherapy, we can give patients better care and improve their lives.
Quality of Life After Brain Tumor Surgery
Medical technology has improved a lot. Now, we focus on making patients thrive after brain tumor surgery. “The goal of brain tumor surgery is not only to remove the tumor but to preserve the patient’s quality of life,” says a leading neurosurgeon. We know the journey doesn’t end with surgery; it’s just the start of a new chapter in a patient’s life.
Neurological Function Preservation
Keeping neurological function intact is key in brain tumor surgery. We use advanced methods like microsurgery and intraoperative imaging. This helps us avoid damaging the brain and keeps the patient’s functions intact.
Research shows that these advanced techniques lead to better outcomes. For example, a study found that microsurgery for brain tumors greatly improved patients’ neurological functions after surgery.
Cognitive and Psychological Outcomes
Cognitive and psychological outcomes are also vital for quality of life after surgery. The surgery and tumor can affect a patient’s mind and mental health. So, we offer not just surgery but also care that addresses these issues.
Our patients get support like cognitive rehab and counseling. One patient said, “The support I got after surgery was priceless. It helped me regain my confidence and adjust to my new life.”
Return to Daily Activities and Work
Getting back to daily life and work is a big step for patients after surgery. We help our patients get back to their normal lives as much as they can. Being able to work or do daily activities shows how well a patient is doing after surgery.
The type of tumor, its location, and the patient’s health are important for getting back to normal. We make treatment plans that fit each patient’s needs. Our goal is to help them recover well and get back to their daily lives.
Recurrence Risks After Brain Tumor Surgery
It’s important for patients and their families to know about the risks of brain tumor recurrence after surgery. Surgery can save lives but doesn’t always remove the tumor completely. This means there’s a chance the tumor could come back.
Predicting Tumor Recurrence
Several things can tell us if a tumor might come back. The type of tumor is a big factor. For example, benign tumors like meningiomas usually don’t come back as often as malignant tumors like glioblastomas. Genetic markers also play a big role. Tumors with certain genes might grow back faster.
How much of the tumor is removed during surgery also matters. Tumors that are fully removed have a lower chance of coming back. But if only part of the tumor is taken out, the risk is higher.
Monitoring and Follow-up Protocols
It’s key to keep an eye on things after surgery to catch any recurrence early. This means regular imaging studies like MRI or CT scans, and checking for any new symptoms. How often you need to go back for these checks depends on the tumor type, how much was removed, and your health.
Some patients might also need treatments like radiation or chemotherapy after surgery. This can help lower the chance of the tumor coming back.
Treatment Options for Recurrent Tumors
If a tumor does come back, there are different ways to treat it. The choice depends on the tumor type, where it is, and what treatments you’ve had before. Repeat surgery might be an option if the tumor is in a place that’s easy to get to.
Other treatments include stereotactic radiosurgery, chemotherapy, and targeted therapy. The right treatment for you will depend on your situation and the tumor’s characteristics.
Knowing about the risks and how to manage them is important for patients with brain tumors. By working with their healthcare team, patients can make a plan to watch for and deal with any recurrence.
Making Informed Decisions About Brain Tumor Surgery
Choosing brain tumor surgery is a big decision. It can change how well you live and feel. Knowing what affects surgery success is key. This helps in making smart choices about your care.
Consulting with Neurosurgical Teams
Talking to neurosurgical teams is a big step. They offer personalized neurosurgical care. They make plans that fit your needs and situation.
These teams include experts from many fields. They work together to care for you fully. This means they look at your tumor and how it affects your health.
Understanding Personal Risk Factors
Knowing your personal risks is important. Things like age, health, and genetics can affect surgery. Understanding these helps you see the risks and benefits of surgery.
Talk about your health and worries with your team. This helps find and plan for risks. It prepares you for what surgery might bring.
Second Opinions and Specialized Centers
Getting second opinions and care at specialized centers is wise. These places have the newest treatments and technologies. They offer the best care available.
A second opinion can confirm or suggest better plans. Look for centers with brain tumor experience. They have the teams and treatments for the best results.
By working with neurosurgical teams, understanding risks, and getting second opinions, you make smart choices. This approach lets you be involved in your care. It helps you face treatment with confidence and clarity.
Conclusion
Neurosurgery has made big strides, thanks to new techniques and treatments. This has led to better success rates in brain tumor surgeries. We’ve looked at how things like the tumor’s type, location, size, and the patient’s health play a role.
It’s clear that a full care approach is key for the best results in brain tumor surgery. Using modern surgery, along with chemotherapy, radiation, and targeted therapy, can greatly improve patient outcomes. This way, we can make patients’ lives better and more fulfilling.
At our institution, we’re all about top-notch healthcare for international patients. Our team of experts works hard to understand each patient’s needs. We create personalized treatment plans to ensure the highest success rates in neurosurgery.
We’re always pushing forward in neurosurgery, aiming to give our patients the best care. Our goal is to keep improving brain tumor surgery stats. We want to make a real difference in the lives of those fighting brain tumors.
FAQ
What is the overall success rate of brain tumor surgery?
The success rate of brain tumor surgery depends on several factors. These include the type of tumor, its location, and the patient’s health. Generally, surgery for benign tumors has a higher success rate than for malignant ones.
How does tumor location affect surgical success?
The location of a tumor greatly affects surgical success. Tumors in easy-to-reach areas usually have better outcomes. This is compared to those in deep or sensitive brain areas.
What are the success rates for benign brain tumor surgery?
Surgery for benign brain tumors, like meningioma, acoustic neuroma, and pituitary adenoma, often has high success rates. Many patients see their tumors completely removed and experience significant symptom relief.
How effective is surgery for malignant brain tumors?
Surgery for malignant brain tumors, such as glioblastoma, can improve survival and quality of life. This is when combined with treatments like chemotherapy and radiation therapy.
What role does tumor size play in surgical outcomes?
Tumor size impacts the complexity and outcome of surgery. Smaller tumors are easier to remove completely. Larger tumors may need more complex surgical approaches.
How do patient factors influence brain surgery success?
Patient factors like age, overall health, and neurological status before surgery greatly impact success. Patients with fewer health issues and better neurological function tend to have better outcomes.
What modern surgical techniques have improved brain tumor surgery outcomes?
Modern techniques like microsurgery, neuronavigation, and awake craniotomy have improved precision and safety. This has led to better outcomes for patients.
What are the benefits of minimally invasive brain tumor surgery?
Minimally invasive techniques, such as endoscopic approaches and LITT, offer benefits. These include smaller incisions, less tissue damage, and quicker recovery times. Their suitability depends on the tumor characteristics.
How does multimodal treatment impact brain tumor surgery success?
Combining surgery with treatments like chemotherapy, radiation therapy, and targeted or immunotherapy can significantly improve outcomes. This can also increase survival rates.
What factors influence quality of life after brain tumor surgery?
Factors like preserving neurological function, cognitive and psychological outcomes, and returning to daily activities and work are key. These influence quality of life after surgery.
What are the risks of tumor recurrence after brain tumor surgery?
The risk of tumor recurrence varies based on tumor type, removal completeness, and other factors. Regular monitoring and follow-up are essential for early detection of recurrence.
How can patients make informed decisions about brain tumor surgery?
Patients should consult with neurosurgical teams to understand their personal risk factors and treatment options. They should also consider the benefits and risks of surgery. Seeking second opinions at specialized centers is also recommended.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa043330