Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 30% of all brain tumors are meningiomas, and surgery is often the chosen treatment path. For patients facing brain tumor surgery, concerns about pain are key. The thought of a craniotomy surgery can be scary, not just because of pain. It’s also because of the unknowns about the procedure and what comes after.
At our institution, we focus on the success of the neurosurgery and our patients’ comfort. The pain level during and after meningioma surgery can differ a lot. This depends on the tumor’s location, size, and the patient’s health.
Key Takeaways
- Pain is a big worry for those having brain tumor surgery.
- The pain level can change based on several factors, like tumor location and health.
- Knowing what affects pain can help manage expectations.
- Our institution puts a big focus on patient comfort and well-being, along with successful neurosurgery.
- Good pain management is key for recovery.
Understanding Brain Tumors and Meningiomas

It’s important to know about brain tumors, like meningiomas, if you’re facing surgery. Brain tumors can be either primary or secondary. Primary tumors start in the brain, while secondary ones spread from other parts of the body.
Types of Brain Tumors
Brain tumors are divided by where they come from. The main types are:
- Glioma: These tumors come from glial cells and can be either benign or malignant.
- Meningioma: Usually benign, these tumors grow in the meninges, which protect the brain.
- Pituitary Adenoma: These are tumors in the pituitary gland and are often benign.
What Are Meningiomas?
Meningiomas are tumors that grow from the meninges. They are mostly benign and can grow at different rates. Most meningiomas grow slowly, and some may not need treatment right away. But, bigger or faster-growing meningiomas can harm the brain or spinal cord, causing symptoms.
When Surgical Intervention Becomes Necessary
Surgery is needed when a meningioma:
- Causes big symptoms because of its size or where it is.
- Is growing fast.
- Is causing problems with the nervous system.
Choosing surgery depends on the tumor’s type and the patient’s health. Tumor resection is often the best choice for meningiomas that are causing trouble or might in the future.
Knowing about brain tumors and meningiomas helps patients understand neurosurgery operation better. This way, they can make better choices about their treatment.
The Reality of Pain in Brain Surgery
Many worry about pain during and after brain surgery. But what’s the truth about this pain? Knowing the facts can ease some of the fear.
Misconceptions About Brain Surgery Pain
Some think brain surgery is very painful because of the brain’s sensitivity. But, the brain itself doesn’t have pain receptors. The brain is a unique organ in that it doesn’t feel pain directly.
The surgery’s complexity and delicacy might make us think it’s very painful. But, thanks to new surgical methods and pain control, the pain after surgery is much less.
Pain Receptors in the Brain
The brain doesn’t have pain receptors. These are special nerve endings that send pain signals. This is key to understanding why some pain happens during and after brain surgery.
But, the scalp and skull, which are involved in a craniotomy, do have pain receptors. So, while the brain itself doesn’t feel pain, the areas around it do.
What Actually Causes Discomfort
So, what causes pain during and after brain surgery? The main reasons are the incision site, swelling, and how the body reacts to the surgery.
- Post-operative pain often comes from the incision and healing.
- Swelling and inflammation can cause discomfort and pressure.
- The body’s overall response to surgery can lead to fatigue and pain.
Knowing these reasons can help patients get ready for recovery and understand pain better.
By understanding the truth about brain surgery pain and how it’s managed, patients can feel less anxious about their surgery.
Pre-Surgical Evaluation and Preparation
Before brain tumor surgery, a thorough evaluation is key. This includes many steps. These are vital for a successful surgery and recovery.
Diagnostic Procedures
Diagnostic tests are very important. They help doctors understand the tumor and plan the surgery.
- MRI (Magnetic Resonance Imaging): Shows detailed brain and tumor images.
- CT (Computed Tomography) Scan: Checks the tumor’s size and where it is.
- Angiogram: Looks at the blood vessels around the tumor.
Physical and Psychological Preparation
Getting ready physically and mentally is also key. Patients should:
- Eat well and drink plenty of water.
- Use stress-relief methods like meditation or deep breathing.
- Follow the doctor’s advice on medication and lifestyle changes.
Having a support system is also important. Family or friends can offer emotional support.
Pain Management Planning
Pain management is a big part of getting ready for surgery. Our team creates a pain plan for each patient. This plan may include:
- Medication: To control pain and discomfort.
- Alternative therapies: Like acupuncture or physical therapy to help with pain.
Planning ahead helps reduce pain and makes recovery easier.
Anesthesia Options for Brain Tumor Surgery
Choosing the right anesthesia for brain tumor surgery is complex. It involves different methods to meet each patient’s needs. Anesthesia is key to keeping patients comfortable and safe during surgery.
General Anesthesia
General anesthesia is a common choice for brain tumor surgery. It makes patients unconscious and blocks pain. General anesthesia helps the surgical team manage the patient’s vital signs and keeps them steady during surgery. This is great for complex surgeries needing precise work.
The benefits of general anesthesia include:
- Complete pain relief during the surgery
- Ability to control vital signs
- Patient remains steady, lowering the risk of problems
Awake Craniotomy
Awake craniotomy is a special method used in some brain tumor surgeries. It keeps the patient awake and able to follow commands during surgery. The main goal is to avoid harming important brain areas, like those for speech or movement. This way, surgeons can watch brain activity and adjust as needed.
The advantages of awake craniotomy include:
- Lower risk of brain damage
- More accurate tumor removal
- Quicker recovery in some cases
Local Anesthesia Techniques
Local anesthesia numbs a specific area, like the scalp, to lessen pain during brain tumor surgery. It’s not used alone but can be added to other methods to manage pain. This helps during and after surgery.
The benefits of local anesthesia include:
- Less pain after surgery
- Less need for strong pain meds
- Potential for quicker recovery
In conclusion, picking the right anesthesia for brain tumor surgery depends on many factors. These include the tumor’s size and location, and the patient’s health. Knowing about the different anesthesia options helps patients make better choices for their care.
Meningioma Surgery: Procedure and Techniques
Removing meningiomas involves different techniques based on the tumor’s size and location. This surgery is very delicate. It needs a deep understanding of neurosurgery.
Surgical Approaches for Meningioma Removal
There are many ways to remove meningiomas, each with its own benefits. The right approach depends on the tumor’s size, location, and the patient’s health.
- Craniotomy: This common method involves temporarily removing a part of the skull to reach the tumor.
- Keyhole Surgery: A less invasive option that uses a small incision and special tools.
- Endoscopic Surgery: Uses an endoscope for tumors near the brain’s surface.
Step-by-Step Procedure
The steps for meningioma surgery are critical:
- Pre-operative planning: Detailed imaging studies are done to understand the tumor’s anatomy.
- Anesthesia administration: General anesthesia is used to keep the patient comfortable.
- Craniotomy or surgical approach: The chosen method is used to access the tumor.
- Tumor removal: The meningioma is carefully removed.
- Closure: The skull is replaced, and the incision is closed.
Duration and Complexity Factors
The length and complexity of meningioma surgery vary based on several factors:
- Tumor size and location: Larger tumors or those in critical areas make the surgery harder.
- Patient’s health: Existing medical conditions can affect the surgery’s complexity.
- Surgeon’s experience: The neurosurgeon’s skill is key to the surgery’s success.
Types of Brain Surgery Procedures
Brain surgery includes many procedures, each for different conditions and needs. The choice of surgery depends on the tumor’s type, size, and where it is in the brain.
Traditional Craniotomy
A traditional craniotomy removes part of the skull to reach the brain. It lets surgeons see and remove tumors or lesions directly. Though it’s more invasive, better surgery and care have made it safer.
Key aspects of traditional craniotomy include:
- Direct access to the brain
- Ability to handle complex cases
- Requires a longer recovery period compared to minimally invasive techniques
Minimally Invasive Options
Minimally invasive brain surgery is becoming more popular. It aims to reduce recovery time and scarring. These surgeries use smaller cuts and special tools.
Benefits of minimally invasive surgery include:
- Smaller incisions, resulting in less scarring
- Reduced risk of infection
- Shorter hospital stays and recovery times
Transsphenoidal Approaches
Transsphenoidal surgery is for tumors near the pituitary gland. It goes through the sphenoid sinus, not needing a traditional craniotomy.
Endoscopic Techniques
Endoscopic brain surgery uses a thin, flexible tube with a camera and light. It’s often paired with transsphenoidal surgery.
Advantages of endoscopic techniques include:
- High-definition visualization
- Minimally invasive, reducing tissue damage
- Potential for faster recovery
Knowing about different brain surgery types helps patients understand their treatment. It lets them make better choices about their care.
Immediate Post-Operative Pain Experience
Understanding pain after brain surgery is key to managing it well. The first days after surgery are very important for recovery.
First 24-48 Hours After Surgery
The first 24 to 48 hours are critical for pain levels. Patients are watched closely in the ICU for any issues.
We use many ways to manage pain. This includes medicines and other methods to reduce discomfort.
Common Pain Locations and Sensations
Pain after craniotomy can be felt in different places. It often hurts at the incision site, the head, and sometimes the neck and shoulders.
People say the pain feels like a dull ache, but it can also be sharp or throbbing. The feeling can change based on the person’s pain level and the surgery type.
Factors Affecting Post-Operative Pain Levels
Many things can change how much pain a patient feels. These include how big the surgery was, the patient’s health, and how much pain they can handle.
| Factor | Description | Impact on Pain |
| Surgical Extent | The complexity and duration of the surgery | More extensive surgeries may result in higher pain levels |
| Individual Health | Pre-existing health conditions | Patients with certain conditions may experience more pain |
| Pain Tolerance | Individual threshold for pain | Higher tolerance may result in lower reported pain levels |
Knowing these factors helps us create better pain plans for our patients. This makes their recovery better.
Pain Management Strategies After Brain Surgery
Managing pain after brain tumor surgery is complex. It involves many strategies. Effective pain management is key for recovery and well-being. We will discuss the methods used, including medication and non-pharmaceutical approaches.
Medication Protocols
Medication is a big part of managing pain after surgery. We use a mix of analgesics, like opioids and non-opioids. This is to fit each patient’s needs.
The type of medication depends on the pain level, patient health, and side effects. We keep a close eye on how the medication is working. This lets us make changes as needed.
Non-Pharmaceutical Approaches
Non-pharmaceutical methods also play a big role in pain management. These include physical therapy, relaxation techniques, and cognitive-behavioral therapy.
These methods help lower pain perception and improve recovery. We encourage patients to try these as part of their care plan.
Managing Headaches and Incision Pain
Headaches and incision pain are common after brain surgery. We tackle these with a mix of medication and other strategies.
For headaches, we use specific medications and techniques. Incision pain is managed with local anesthesia and careful wound care.
Here’s an overview of common pain management strategies:
| Strategy | Description | Benefits |
| Medication | Use of analgesics to manage pain | Effective for severe pain, can be adjusted |
| Physical Therapy | Gentle exercises to improve mobility | Reduces pain, improves recovery |
| Relaxation Techniques | Methods like deep breathing, meditation | Reduces stress, helps in pain management |
Understanding pain management after brain surgery can be tough. Visual aids can help make it clearer.
Recovery Timeline and Pain Progression
Recovering from brain tumor surgery takes time, patience, and care. The recovery timeline varies for everyone. It depends on the surgery type, tumor size and location, and the patient’s health.
Hospital Recovery Phase
The first part of recovery happens in the hospital. It usually lasts a few days to a week after surgery. Medical staff watch over the patient, managing pain and looking for complications.
Managing pain well is key during this time. Patients get medicines to control pain, reduce swelling, and prevent seizures. The team also teaches patients and their caregivers about home recovery.
First Month at Home
After leaving the hospital, recovery continues at home. The first month is vital for healing and adjusting to surgery changes. Patients might feel tired, have headaches, or notice cognitive changes.
It’s important to follow the craniotomy recovery time advice from healthcare professionals. This helps ensure a smooth recovery.
| Week | Common Experiences | Recommended Actions |
| 1-2 | Fatigue, pain, swelling | Rest, elevate head, follow medication regimen |
| 2-4 | Gradual improvement, possible cognitive fog | Continue rest, start gentle exercises, monitor cognitive changes |
Long-Term Pain Resolution
Most patients see big improvements in the first few months. But, some pain or discomfort might last. How long pain lasts depends on surgery extent and individual pain tolerance.
It’s important for patients to talk openly with their healthcare team about pain and concerns. This way, they get the right help and support for their recovery timeline.
Long-Term Side Effects of Craniotomy and Brain Surgery
When we talk about brain surgery recovery, we must think about long-term side effects. These can really affect a patient’s life quality.
Physical Side Effects
Physical side effects after craniotomy and brain surgery can differ a lot. Some common ones are:
- Weakness or numbness in parts of the body
- Seizures, which may need ongoing medication
- Changes in how you see or hear things
- Feeling very tired, which can last a long time
These physical changes can be tough. But, with the right help and support, many people can get better and live independently again.
Cognitive and Neurological Changes
Cognitive and neurological changes are also possible long-term effects. These can include:
- Memory problems or trouble focusing
- Mood changes, like feeling sad or anxious
- Changes in how you act or feel
- Difficulty with speaking or understanding language
It’s important for patients and their families to know about these possible changes. They should also get help from doctors if they notice any of these symptoms.
Chronic Pain Syndromes
Chronic pain is another long-term side effect of brain surgery. The pain can be different, like headaches or pain at the surgery site.
“Pain management is a critical aspect of recovery. Patients should work closely with their healthcare team to find the most effective strategies for managing chronic pain.” – Expert in Neurosurgery
Dealing with chronic pain often needs a mix of treatments. This can include medicine, physical therapy, and sometimes things like acupuncture or mindfulness.
Knowing about the long-term side effects of brain surgery is key. It helps patients make good choices about their care. It also prepares them for the recovery journey ahead.
Patient Experiences: What to Really Expect
Every patient’s journey through brain tumor surgery is unique. Hearing their stories can be enlightening and comforting. Patients share valuable insights into the recovery process, helping others prepare for challenges and triumphs.
Testimonials and Common Experiences
Many patients who have had meningioma surgery share a range of experiences. They talk about the initial diagnosis and the recovery phase. Some say the first few days were tough due to discomfort and swelling.
But as time went on, they started to feel more like themselves.
“The support from other patients who had gone through similar experiences was invaluable. It helped me understand what to expect and how to cope with the recovery process.”
— A meningioma surgery patient
Patients often face varying levels of pain, fatigue, and emotional changes. Knowing these common experiences can help prepare others for what’s ahead.
Coping Strategies from Former Patients
Former patients share their coping strategies to help others. Some effective strategies include:
- Maintaining a positive outlook and focusing on progress
- Engaging in gentle physical activities as recommended
- Seeking support from family, friends, and support groups
- Using pain management techniques as prescribed
These strategies can greatly help a patient manage their recovery.
Psychological Aspects of Recovery
The psychological aspect of recovery is just as important as the physical. Patients often feel a range of emotions, from anxiety and fear to relief and gratitude. It’s vital to address these emotional needs through:
- Counseling and therapy sessions
- Support groups where patients can share their experiences
- Family and friends providing emotional support
By acknowledging and addressing the psychological aspects of recovery, patients can better navigate their journey towards healing.
Advancements in Brain Tumor Surgery
Recent years have seen big changes in brain tumor surgery. These changes are making surgeries better and helping patients recover faster.
Technological Innovations
New technologies are leading these changes. Tools like intraoperative MRI and navigation systems help surgeons be more precise. Intraoperative MRI lets doctors see the tumor in real-time during surgery.
Robotic-assisted surgery is also a big step forward. It gives surgeons better control and vision, making complex surgeries more accurate.
Improved Pain Management Techniques
Pain management is key in brain tumor surgery. New pain management methods are making patients more comfortable and helping them recover faster. Multimodal analgesia is a popular approach, using different pain relief methods together.
The integration of advanced pain management strategies has revolutionized the way we care for our patients undergoing brain tumor surgery.
Other methods include local anesthetics and nerve blocks to lessen pain after surgery. These methods are not only improving patient results but also cutting down hospital stays.
| Pain Management Technique | Description | Benefits |
| Multimodal Analgesia | Combination of pain relief medications | Effective pain control, reduced opioid use |
| Local Anesthetics | Numbing specific areas | Reduced post-operative pain |
| Nerve Blocks | Blocking pain signals | Significant pain reduction |
Future Directions in Neurosurgery
The future of brain tumor surgery is bright, with new technologies and techniques coming. Gene therapy and immunotherapy are being looked at for better treatments.
- Gene therapy aims to modify genes to prevent or treat diseases.
- Immunotherapy harnesses the body’s immune system to fight cancer.
These new developments are expected to make brain tumor surgery even better. They offer hope and new possibilities for patients.
The Financial Aspect: Cost of Brain Tumor Surgery
Understanding the financial side of brain tumor surgery is key for patients. The cost can be high, and knowing the details is the first step to handle these expenses.
Average Costs in the United States
The cost of brain tumor surgery in the U.S. varies a lot. It depends on the surgery’s complexity, the surgeon’s fees, and the hospital’s charges. On average, it can cost from $80,000 to over $200,000. This includes costs before, during, and after the surgery.
Insurance Considerations
Insurance is a big factor in managing surgery costs. Most insurance plans cover a lot of the costs. But, it’s important to know your policy’s details, like deductibles and co-payments.
Financial Resources and Support
There are many ways to help manage surgery costs. Non-profit groups, government programs, and hospital financial help are available.
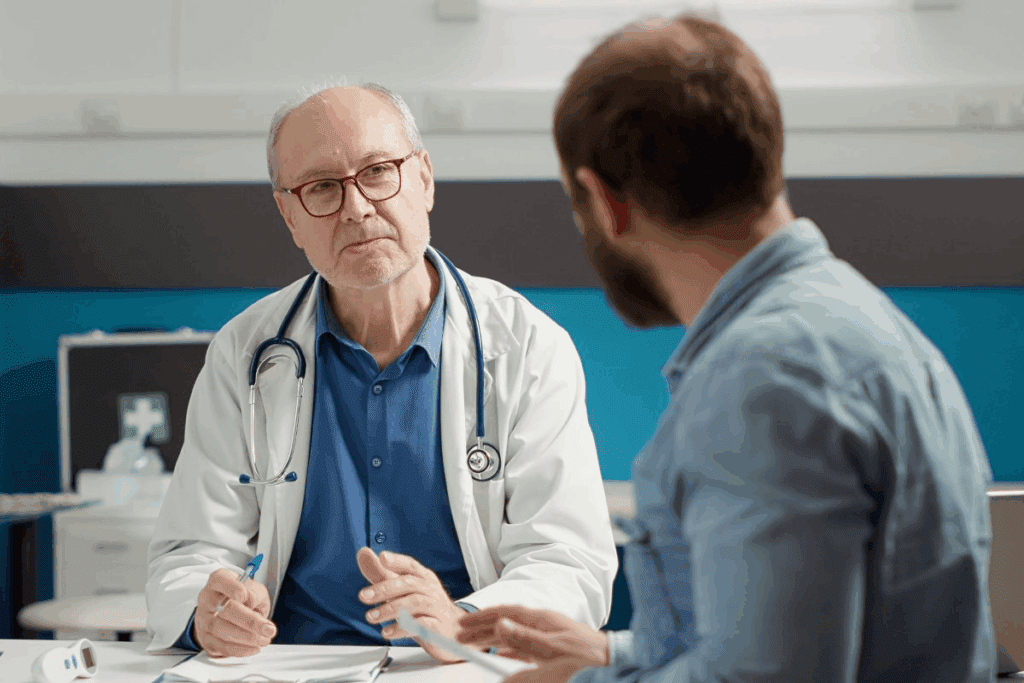
Choosing the Right Neurosurgeon and Hospital
Choosing the right neurosurgeon and hospital is key for brain tumor surgery. It greatly affects patient outcomes. This choice is vital for the best care.
Qualifications to Look For
When picking a neurosurgeon, look at their qualifications and experience. Board certification in neurosurgery is a must. Also, find surgeons with brain tumor surgery training and good results.
As a top neurosurgeon says, “Experience is key in neurosurgery. It affects how precise and caring the care is.”
The best outcomes in brain tumor surgery are often achieved by teams with extensive experience and a multidisciplinary approach.”
Questions to Ask Your Surgeon
Prepare questions for your surgeon. Ask about their experience with similar cases, pain management, and recovery time. Also, ask about the hospital’s support services and post-operative care.
- What is your experience with brain tumor surgeries?
- What are the possible risks and complications?
- How will pain be managed during recovery?
Specialized Centers for Brain Tumor Treatment
Choosing a hospital that specializes in brain tumors is wise. These centers have expert teams and the latest technology. This can greatly improve results.
By thinking about these points, patients can make smart choices. This leads to better health outcomes.
When to Contact Your Doctor After Surgery
Knowing when to seek medical help after brain tumor surgery is key to a smooth recovery. It’s important to watch for signs that may mean you need more care. These signs can help you avoid serious complications.
Warning Signs of Complications
Keep an eye on your body for any odd symptoms after surgery. Severe headache, confusion, or trouble speaking are big warning signs. Also, look out for fever, redness, or swelling at the surgery site.
Normal vs. Abnormal Pain Patterns
It’s important to know the difference between normal pain and pain that might be a problem. Some pain is okay after surgery, but pain that gets worse or comes with other bad symptoms needs your doctor’s attention.
| Symptom | Normal | Abnormal |
| Headache | Mild to moderate | Severe or worsening |
| Fever | Less than 100.4°F (38°C) | Greater than 100.4°F (38°C) |
| Surgical Site | Mild redness or swelling | Increasing redness, swelling, or discharge |
Emergency Situations
If you have severe symptoms like trouble breathing, chest pain, or sudden bad headache, get emergency help right away. It’s always safer to be cautious with your health after surgery.
Conclusion: The Journey Through Brain Tumor Surgery
Going through brain tumor surgery, like meningioma surgery, is a big deal. We’ve looked at the different parts of this journey. This includes learning about brain tumors and the surgery, managing pain, and getting better.
Brain tumor surgery, like meningioma surgery, needs careful neurosurgery. The road to recovery is tough, but with the right pain care and after-surgery help, many do well. New advances in neurosurgery have helped many patients live longer and better.
For those starting this journey, knowing what to expect and getting support is key. Picking the right neurosurgeon and hospital, understanding costs, and knowing possible issues can help a lot. We urge patients to stay hopeful and active in their healing.
With the right help and support, many people can get back to their usual lives after surgery. We aim to provide top-notch healthcare and support for international patients needing neurosurgery.
FAQ
What is a craniotomy, and how is it related to brain tumor surgery?
A craniotomy is a surgery where part of the skull is removed to reach the brain. It’s often used for brain tumor surgeries, like removing meningiomas. This lets surgeons safely remove the tumor.
How painful is brain tumor surgery, and what kind of pain can I expect?
Brain tumor surgery isn’t usually painful because of anesthesia. But, after surgery, pain is common. People might feel discomfort, headaches, or pain where the incision was. These can be managed with medicine and other strategies.
What are the long-term side effects of craniotomy and brain surgery?
Long-term effects can differ based on the person, the tumor’s location, and the surgery’s extent. Some might experience physical, cognitive, or neurological changes, or chronic pain. Yet, many recover well or with minor lasting effects.
How long does it take to recover from brain tumor surgery?
Recovery times vary greatly. Hospital stays are usually a few days to a week. Full recovery at home can take weeks to months. Recovery depends on the surgery’s complexity, the patient’s health, and any complications.
What are the different types of brain surgery for tumor removal?
There are various brain surgeries, like traditional craniotomy and minimally invasive options. The choice depends on the tumor’s location, size, and type, and the patient’s condition. The surgeon’s judgment also plays a role.
How much does brain tumor surgery cost, and what are the insurance considerations?
The cost of brain tumor surgery varies based on location, procedure complexity, and provider. Insurance coverage also differs. It’s important to check with your insurance to understand what’s covered and what you might pay out-of-pocket.
When should I contact my doctor after brain tumor surgery?
Call your doctor if you have severe headache, fever, confusion, or trouble speaking. Knowing what normal and abnormal pain is can help you seek medical help when needed.
Can I manage pain effectively after brain surgery?
Yes, managing pain after surgery is key. This includes medication, non-pharmaceutical methods, and strategies for headaches and incision pain. Working with your healthcare team can help find the right pain management plan for you.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4027119/