Last Updated on December 2, 2025 by Bilal Hasdemir
Invasive surgeries are complex medical procedures that need a lot of skill and precision. They are often life-saving but also come with big risks and challenges.brain surgeonBrain Surgeon vs. Cardiac: What is the Hardest Surgery?
Some of the most invasive surgeries include thoracic aortic dissection repair and craniectomy. These are critical for treating severe vascular and neurological conditions. These procedures are among the most complex and demanding in the medical field.
We will explore some of the most invasive surgeries, including those related to neurosurgery. We will discuss their significance in modern medicine.
Key Takeaways
- Invasive surgeries are complex and require great skill.
- Thoracic aortic dissection repair is a highly invasive procedure.
- Craniectomy is another critical invasive surgery.
- Neurosurgery is a field that involves highly invasive procedures.
- Invasive surgeries are often life-saving but come with significant risks.
Defining Invasive Surgery in Modern Medicine
In today’s medicine, ‘invasive surgery’ means procedures that deeply affect the body. These surgeries often require big cuts or special methods to reach inside organs or structures.
It’s important to know that how invasive a surgery is can differ a lot. Let’s look at what makes a surgery invasive.
Criteria That Determine Surgical Invasiveness
Several key factors help decide if a surgery is invasive. These include:
- The size and location of the incision
- The extent of tissue damage or disruption
- The duration of the procedure
- The risk of complications or morbidity
- The recovery time required
Surgeries with high scores on these factors are seen as more invasive. For example, open-heart surgery or organ transplants are very invasive. This is because they cause a lot of tissue damage and take a long time to recover.
Scales and Classifications Used by Medical Professionals
Doctors use different scales and classifications to measure surgery invasiveness. One way is to group surgeries by complexity and risk.
The Clavien-Dindo Classification is a well-known system. It ranks surgical complications by how severe they are. This helps standardize how invasive a surgery is and its risks.
Other systems might focus on surgery types, like minimally invasive surgery (MIS) versus open surgery. MIS, like laparoscopic surgery, is less invasive. This is because it uses smaller cuts and causes less tissue damage.
Understanding these criteria and classifications helps us see the details of surgical invasiveness. It also shows how they affect patient results.
The Critical Role of the Brain Surgeon in Complex Procedures
Brain surgery is very complex and needs a lot of training and skill from neurosurgeons. This field is not only crucial but also very challenging.
Educational Path and Specialized Training
The path to becoming a neurosurgeon is long and tough. After medical school, they enter a residency program. This gives them hands-on experience in treating neurological conditions.
Many neurosurgeons also do fellowship programs for one to two years. These programs help them specialize in areas like pediatric neurosurgery or spinal surgery.
The field of neurosurgery keeps changing with new technologies and techniques. So, brain surgeons must keep learning and updating their skills. They do this by going to conferences and workshops.
Why Neurosurgery Ranks Among the Most Demanding Specialties
Neurosurgery is very demanding because of its complexity and high stakes. Brain surgeons need to know a lot about neuroanatomy and be skilled in microsurgery. They also have to make important decisions quickly.
Even small mistakes in brain surgery can have big consequences. This adds to the stress and responsibility neurosurgeons face.
Craniotomy: The Gateway to Brain Surgery
Brain surgery often starts with a craniotomy. This lets surgeons get to the brain. They remove a part of the skull, called a bone flap, to treat the brain area. Craniotomy is key in neurosurgery, helping surgeons do many complex tasks.
Types of Craniotomy Procedures
There are different craniotomy procedures for various needs. These include:
- Standard Craniotomy: The traditional way, where a part of the skull is removed to get to the brain.
- Keyhole Craniotomy: A less invasive method with smaller incisions and a smaller bone flap.
- Decompressive Craniotomy: Done to take pressure off the brain by removing a bigger part of the skull.
As “The choice of craniotomy technique depends on the location and nature of the brain condition being treated.” – a principle that guides neurosurgeons in selecting the most appropriate method for each patient’s needs.
Risks and Recovery Expectations
Craniotomy, like any big surgery, has risks like infection, bleeding, and bad reactions to anesthesia. Recovery time varies based on health and the surgery’s complexity. Patients usually need to be watched closely in an ICU right after surgery. “Recovery can be a long and challenging journey, but with proper care and rehabilitation, many patients are able to return to their normal activities,” as emphasized by healthcare professionals.
After surgery, care includes managing pain, watching for problems, and rehab to get strength and thinking back. The medical team works with the patient and their family to help them recover well.
Deep Brain Interventions: Accessing the Core of Human Consciousness
Deep brain interventions are at the edge of neurosurgery, exploring new ways to treat complex brain issues. These surgeries reach deep into the brain, needing advanced skills and a deep knowledge of brain anatomy. They also rely on the latest technology.
Surgical Approaches to Deep Brain Structures
Surgeons use different methods to reach deep brain areas. Each method has its own challenges and things to consider. The choice depends on the condition, where the target is, and the patient’s health.
Stereotactic Surgery is a common method. It uses a stereotactic frame for precise targeting. This way, surgeons can access deep brain areas with less invasive methods.
- Frame-based stereotaxy
- Frameless stereotaxy using advanced imaging
- Functional neurosurgery for conditions like Parkinson’s disease
Technological Tools for Precision Navigation
The success of deep brain surgeries depends a lot on advanced technology. Intraoperative MRI and CT scans give surgeons real-time feedback. This helps them make adjustments during the surgery.
Other key technologies include:
- Advanced imaging techniques like diffusion tensor imaging
- Microelectrode recording for functional mapping
- Robot-assisted surgery for better precision
These technologies have greatly improved deep brain surgeries. They offer new hope to those with conditions that were once untreatable.
Hemispherectomy and Radical Brain Resections
Hemispherectomy is a surgery that removes half of the brain. It’s a drastic step for severe epilepsy or other brain conditions.
It’s considered when a patient’s life is greatly affected by their condition. Other treatments have failed. A team of healthcare experts carefully decides if it’s needed.
When Removing Half the Brain Becomes Necessary
Severe, uncontrolled epilepsy is the main reason for this surgery. Other conditions include:
- Rasmussen’s encephalitis, a rare inflammatory brain disease
- Hemimegalencephaly, where one brain half is too big
- Sturge-Weber syndrome, affecting blood vessel development
Removing the affected half can greatly reduce seizures. It improves the patient’s quality of life.
Awake Craniotomy: Surgery on the Conscious Brain
Modern medicine has made it possible to perform awake craniotomy. This surgery lets doctors work on the brain while the patient is awake. It’s a complex task that needs teamwork between the doctors and the patient.
Mapping Brain Function During Active Surgery
During an awake craniotomy, doctors use special techniques to map the brain. They stimulate different parts of the brain to see their roles. This helps them keep important functions like speech and movement safe.
Neurophysiological monitoring is key in this process. It helps doctors navigate the brain’s complex paths with care.
Mapping brain function is a delicate task. Patients must be involved and focused. They might be asked to count or name objects while their brain is being stimulated. This feedback is crucial for avoiding damage to important areas.
Patient Experience and Psychological Preparation
Having an awake craniotomy can be scary for patients. Psychological preparation is very important. Patients learn what to expect, including the sensations they might feel and their role in the surgery.
Being awake during brain surgery can be intimidating. But with the right preparation and support, many patients find it manageable. The surgical team works hard to keep the patient comfortable and cooperative.
Multi-Organ Transplantation: The Ultimate Surgical Marathon
Multi-organ transplantation is a top challenge in surgery. It pushes the limits of medical science and teamwork. This complex surgery involves transplanting many organs at once. It needs a team of experts working together.
Immunological Challenges and Rejection Prevention
Multi-organ transplantation also faces big immunological challenges. The risk of rejection is high because the body might see the new organs as threats. To prevent this, doctors use drugs to weaken the immune system.
Finding the right balance in these drugs is key. Monitoring and adjusting these drugs after the transplant is vital for success. Doctors often use a mix of drugs to keep the immune system in check.
In summary, multi-organ transplantation is a complex surgery. It needs careful planning, teamwork, and a deep understanding of the immune system. As medical science grows, so will the success of these surgeries.
Ex Vivo Procedures: Removing Organs for Repair
Ex vivo procedures are a new way in surgery. They let doctors take out organs to fix them outside the body. This method has changed organ repair and transplant, giving hope to many patients.
Technical Challenges of Organ Removal and Reimplantation
Removing an organ for repair is very complex. Organ removal needs great care to not harm the organ or nearby tissues. After taking it out, the organ is fixed or treated outside the body, needing special tools and skills.
Reimplantation is the next big step. It’s when the fixed organ goes back into the body. This part is very careful to make sure the organ works right and the patient is safe.
Pioneering Cases That Defined the Field
Some cases have really moved forward ex vivo procedures. For example, a kidney was taken out, fixed, and put back in for a big tumor.
These cases show that ex vivo procedures work. They also show how they can help patients. As technology gets better, we’ll see even more progress in this area.
Ex vivo procedures are leading the way in surgery. They open up new ways to fix and transplant organs. As we explore more in medicine, these methods will be key in shaping healthcare’s future.
Separation of Conjoined Twins: Surgical Planning and Execution
Conjoined twins are a unique challenge in surgery. They need a team effort for a successful separation. This complex task requires surgical skill, careful planning, and ethical thought.
Ethical Considerations and Decision-Making
Deciding to separate conjoined twins is a big ethical issue. We must think about the benefits and risks. We look at the twins’ life after surgery and their condition.
Key ethical factors include:
- The chance of successful separation
- The twins’ long-term health and happiness
- The risk of losing one twin to save the other
Multidisciplinary Team Requirements
A team of experts is needed for the surgery. This team has surgeons, anesthesiologists, nurses, and more. Each one brings their skills to plan and do the surgery.
| Team Member | Role |
| Surgeons | Lead the surgery, do the separation |
| Anesthesiologists | Manage pain and anesthesia |
| Nurses | Give critical care and support |
Separating conjoined twins is very complex. It shows the importance of a skilled and coordinated team. Together, we can make a big difference in their lives.
Record-Breaking Surgical Durations in Medical History
Some surgeries are known for their complexity and long duration. They test the skills and stamina of the surgical teams. These operations push the limits of medical science and show the endurance of the teams.
Factors Contributing to Extended Operating Times
Several factors can make a surgery last longer. Complexity is a big one, as surgeries with many parts or detailed steps take more time. The experience and skill level of the team also matter, especially for complex cases.
Other factors include the patient’s overall health and any unexpected problems during the surgery. For example, a patient with past surgeries may need more time because of scar tissue or other issues.
“The success of long-duration surgeries depends on a multitude of factors, including meticulous planning, a skilled surgical team, and advanced medical technology.”
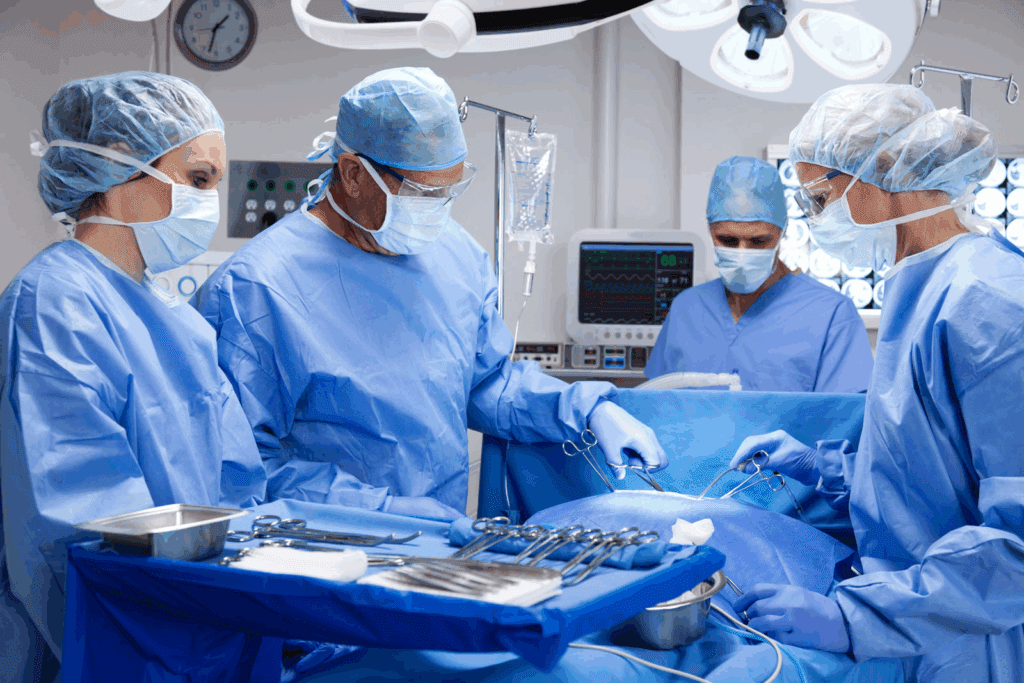
Physical and Mental Endurance of Surgical Teams
The demands on surgical teams during long surgeries are huge. They must stay focused for hours, often under a lot of pressure. The physical demands include standing for long periods, wearing heavy aprons, and the mental strain of making quick decisions under stress.
| Factor | Description | Impact on Surgery Duration |
| Complexity | Intricate procedures or multiple organ involvement | Increases duration due to the need for precision and multiple interventions |
| Surgeon Experience | Skill level and expertise of the surgical team | Can reduce duration with efficient techniques, but complex cases may still be lengthy |
| Patient Health | Pre-existing conditions or complications | May increase duration due to additional precautions or interventions required |
To handle these challenges, teams use strategies like regular breaks and team rotations for long surgeries. They also use advanced ergonomic equipment to lessen physical strain. Mental endurance is helped by pre-operative planning and clear communication among the team.
High-Risk Cardiac and Vascular Interventions
High-risk cardiac and vascular interventions are complex surgeries. They need a lot of skill and precision. These surgeries are often lifesaving, treating serious heart and blood vessel problems.
Aortic Dissection and Aneurysm Repairs
Aortic dissection and aneurysm repairs are very challenging. An aortic dissection happens when there’s a tear in the aorta’s inner layer. This can cause serious problems if not treated quickly.
Doctors use different methods to fix these issues. They might do open surgery or use endovascular stent-grafts. The choice depends on where and how big the problem is.
Complex Congenital Heart Defect Corrections
Congenital heart defects are heart problems present at birth. Some are very complex and need surgery to fix. Doctors use various techniques, sometimes combining surgery and catheter-based procedures.
| Procedure | Description | Complexity Level |
| Aortic Dissection Repair | Surgical repair of a tear in the aorta | High |
| Aneurysm Repair | Repair of a bulge in a blood vessel | High |
| Congenital Heart Defect Correction | Surgical correction of heart defects present at birth | Very High |
These surgeries show how far medical technology and surgery have come. Thanks to these advancements, people with serious heart and blood vessel issues can live better lives.
Extensive Spinal Reconstructions and Vertebral Column Surgery
Spinal reconstructions are among the most complex surgeries today. They are key for fixing severe spinal problems and injuries. This greatly affects patients’ lives.
We handle these surgeries with great care. We know how important the spine is for our health. The surgery’s complexity requires a lot of skill and precision.
Severe Scoliosis Correction Procedures
Scoliosis causes the spine to curve abnormally. When it’s severe, surgery is needed. Correcting severe scoliosis requires careful realignment and stabilization with rods and screws.
The main goal is to straighten the spine, reduce deformity, and ease pain. We use advanced imaging and planning tools for the best results.
Spinal Cord Injury Interventions
Spinal cord injuries can happen due to trauma, infection, or other reasons. They can cause serious neurological problems. Surgery aims to relieve pressure, stabilize the spine, and improve function.
We know how crucial quick and effective treatment is for spinal cord injuries. Our teams work with rehab specialists for full care, from surgery to long-term recovery.
Spinal osteomyelitis surgery shows the complexity of vertebral column surgery. We use the latest methods and technology to help patients recover from extensive spinal reconstructions.
Recovery From Highly Invasive Procedures: The Patient Journey
Recovering from invasive procedures is a big deal. It’s about more than just the body; it’s about the mind too. Knowing what to expect is key for those facing major surgeries.
Intensive Care Requirements and Monitoring
Right after surgery, many patients go to the ICU. Here, they get watched over closely and get help when they need it. Joseph Dearani, M.D., says, “Post-operative care is super important, especially in heart surgery.”
Good care in the ICU helps avoid problems and keeps patients safe.
What happens in the ICU includes:
- Watching vital signs and organ health
- Using machines to help breathe
- Medicine to manage pain and prevent infections
- Food tailored to what the patient needs
Long-term Rehabilitation Pathways
After the ICU, patients start a long journey of getting better. They work on getting strong, moving well, and doing things on their own again. Every person’s path is different, based on their health before surgery, the surgery itself, and any issues after.
Rehab might include:
- Therapy to improve movement and strength
- Help to get back to daily tasks
- Speech therapy for communication or swallowing issues
- Psychological support for emotional healing
Helping patients recover takes a team effort. With the right care, therapy, and support, we can help them get back to their lives.
“The care team plays a vital role in the recovery process, providing not only medical expertise but also emotional support and guidance.”
FAQ
What is considered the most invasive surgery?
The most invasive surgeries are complex procedures like brain surgery and multi-organ transplantation. They require great skill and precision. These surgeries often involve significant tissue damage and longer recovery times.
What makes a surgery invasive?
A surgery is invasive based on tissue damage and procedure complexity. Invasive surgeries need larger incisions. They can lead to longer recovery times and higher risks of complications.
What is a craniotomy, and why is it performed?
A craniotomy is a surgery where part of the skull is removed to access the brain. It’s done to relieve brain pressure, remove tumors, or repair vascular issues.
What is deep brain intervention, and what are the challenges?
Deep brain intervention accesses deep brain structures. Challenges include navigating complex brain anatomy and using advanced tools for precision. It also involves minimizing damage to surrounding tissue.
What is hemispherectomy, and when is it necessary?
Hemispherectomy removes half of the brain. It’s considered for severe epilepsy or conditions affecting one brain hemisphere. Removing the affected part can improve the patient’s quality of life.
What is awake craniotomy, and how does it work?
Awake craniotomy keeps the patient conscious during surgery. It allows surgeons to map brain function in real-time. This ensures critical areas are preserved and requires careful preparation for the patient.
What are the challenges of multi-organ transplantation?
Multi-organ transplantation involves coordinating the procurement and transplantation of multiple organs. It manages complex immunological challenges and prevents rejection. A highly coordinated team effort and advanced immunosuppressive strategies are needed.
What are ex vivo procedures, and what are the technical challenges?
Ex vivo procedures remove organs or tissues for repair or treatment outside the body. The challenges include maintaining organ viability and managing complex surgical techniques. Ensuring successful reimplantation is also crucial.
What are the considerations for separating conjoined twins?
Separating conjoined twins requires complex surgical planning and ethical considerations. A multidisciplinary team is involved. The decision to separate depends on the twins’ anatomy and shared organs, along with potential outcomes for each twin.
What are some of the longest surgeries recorded?
Longest surgeries include complex procedures like multi-organ transplants and separations of conjoined twins. These can last several hours or even days. They require immense physical and mental endurance from the surgical team.
What are high-risk cardiac and vascular interventions?
High-risk cardiac and vascular interventions include surgeries for aortic dissection and aneurysm repairs. They also include corrections of complex congenital heart defects. These procedures are complex, involving delicate vascular structures and requiring precise surgical techniques.
What is involved in extensive spinal reconstructions?
Extensive spinal reconstructions correct severe scoliosis and spinal cord injuries. They require precise techniques and advanced instrumentation. Careful planning is needed to achieve successful outcomes.
What is the patient journey during recovery from highly invasive surgeries?
Recovery from highly invasive surgeries involves intensive care and close monitoring. Long-term rehabilitation is often needed. Patients require significant support, including physical therapy, pain management, and psychological care, to regain strength and adapt to changes.
Why is balancing surgical invasiveness with patient outcomes important?
Balancing surgical invasiveness with patient outcomes is crucial. It ensures the benefits of the surgery outweigh the risks. It involves considering the patient’s condition, procedure complexity, and potential for recovery and improvement.
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/publications/i/item/9789241549882