Many patients worry about pain when they think of awake surgery. Awake craniotomy is a surgery where patients stay awake. It’s a complex procedure that needs careful thought.
Being awake during such a serious surgery can be scary. But, new medical tech and pain control have made it better for patients. Now, awake surgical procedures are less painful.
We focus on making our patients comfortable and safe. We use the latest methods to reduce pain during and after surgery. Our team cares for our patients’ health, mind, and spirit.
Get the definitive answer: is awake surgery painful? Understand the use of local anesthetic for a pain-free experience clearly.
Key Takeaways
- Awake surgery is a complex procedure that requires careful patient care.
- Advances in pain management have improved the patient experience.
- Our institution prioritizes patient comfort and safety.
- Comprehensive care includes addressing emotional and psychological well-being.
- Patients undergo thorough preparation to minimize discomfort.
What Is Awake Surgery?
Awake surgery, also known as conscious surgery, lets patients stay awake during surgery. It’s becoming more popular because it can lead to quicker recovery times and fewer risks from general anesthesia.
Definition and Basic Concepts
Awake surgery means doing operations while the patient is awake and can talk to the team. It needs careful planning, precise anesthesia, and a skilled team.
This method uses local or regional anesthesia to numb the area being operated on. This way, the patient stays awake and alert. It lets surgeons do complex surgeries safely, without the risks of general anesthesia.
Historical Development of Conscious Surgical Techniques
The history of awake surgery started in the early 1900s with local anesthesia experiments. Medical Expert, using local anesthesia for brain surgeries in the early 1900s.
As time went on, better anesthesia and surgical techniques made awake surgery better. New anesthetics and methods, like regional nerve blocks, have made these surgeries safer and more effective.
| Year | Milestone | Description |
| 1900s | Early Use of Local Anesthesia | Dr. Harvey Cushing pioneers the use of local anesthesia for brain surgeries. |
| 1950s | Advancements in Anesthetic Agents | Development of new anesthetic agents improves the safety and efficacy of awake surgery. |
| 2000s | Increased Adoption of Awake Surgery | Awake surgery becomes more widely accepted for various surgical procedures. |
The Truth About Pain During Awake Surgery
Many wonder if patients feel pain during awake surgery. This type of surgery keeps patients awake during the procedure. We’ll look into the truth about pain during these surgeries, the difference between pain and pressure, and what patients say to clear up myths.
Pain vs. Pressure Sensations
In awake surgery, patients often feel pressure, not pain. This is key to knowing what to expect. Local anesthesia numbs the area being operated on, making pain less likely.
But, patients might feel pressure or discomfort from the tools or the surgeon’s actions. This is different from pain and is usually bearable.
What Patients Actually Experience
Patient experiences in awake surgery vary, but many find it comfortable. Let’s examine what patients commonly report:
| Aspect | Patient Experience |
| Pain Level | Mostly minimal to moderate; some report no pain |
| Sensation | Pressure, discomfort, or a feeling of being touched |
| Anxiety Level | Varies; some report feeling calm, others anxious |
The table shows that while some discomfort is common, outright pain is not the usual experience for most patients in awake surgery.
Understanding the difference between pain and pressure, and learning from others, helps patients prepare for awake surgery. This knowledge can reduce fears and make the experience less scary.
Types of Anesthesia Used in Conscious Procedures
Anesthesia is key in awake surgery, keeping patients awake and comfortable. We use different anesthesia methods to make sure patients feel little pain during procedures.
Local Anesthesia Methods
Local anesthesia numbs a specific area of the body for surgery. It’s often used in awake surgery to keep patients awake and pain-free. Local anesthetics like lidocaine and bupivacaine are common choices.
Regional Nerve Blocks
Regional nerve blocks numb a larger area by injecting anesthetic around nerves. This method is great for surgeries on limbs or areas covered by specific nerves. Regional anesthesia offers good pain relief without general anesthesia.
Conscious Sedation Options
Conscious sedation relaxes patients without making them unconscious. It’s often paired with local or regional anesthesia to help patients relax. Sedatives like midazolam and propofol are used to control the level of sedation.
The right anesthesia depends on the surgery, patient history, and the surgical team’s preference. By mixing these methods, we create a personalized anesthesia plan. This ensures a safe and comfortable awake surgery experience for each patient.
- Local anesthesia numbs a specific surgical site.
- Regional nerve blocks anesthetize larger areas by targeting specific nerves.
- Conscious sedation helps patients relax during the procedure.
Pain Management Techniques in Awake Surgery
Managing pain well is key for a successful awake surgery. It keeps patients comfortable during the whole procedure. Awake surgery means patients are awake and can respond, making pain control very important.
Pre-operative Medications
Medications before surgery help a lot. They can lower anxiety and ease pain, making the surgery easier to handle. Some common ones are:
- Anxiolytics: To calm nerves and relax.
- Pain relievers: For pain before, during, and after surgery.
- Sedatives: To relax without losing awareness.
Intra-operative Pain Control
During surgery, controlling pain is essential. This includes:
- Local anesthesia: Numbs the area being operated on.
- Regional nerve blocks: Blocks pain signals to nerves.
- Conscious sedation: Keeps patients relaxed and calm.
Psychological Support and Distraction Methods
Psychological support is also very important. Techniques like guided imagery and deep breathing help reduce pain and anxiety. Our team is ready to offer emotional support and use distractions to help patients.
Some support methods are:
- Guided imagery: Helps patients imagine positive outcomes and distracts them.
- Deep breathing exercises: Helps relax and lower stress.
- Positive reinforcement: Offers reassurance and encouragement.
Common Types of Awake Surgical Procedures
Awake surgery is now a safe choice for many complex surgeries. It’s safer than traditional surgery under general anesthesia. This method is great for surgeries that need the patient’s feedback or are risky under general anesthesia.
Awake Brain Surgery (Craniotomy)
Awake brain surgery, or awake craniotomy, keeps the patient awake during the surgery. It’s key for surgeries near brain areas that control speech, movement, and feeling. This way, surgeons can watch these functions closely and avoid harming important brain parts.
Awake Spine Surgery
Awake spine surgery keeps patients awake during the procedure. It’s often used for less invasive spine surgeries. The patient’s feedback is very helpful. This method lowers the risk of nerve damage and other problems seen with traditional surgery.
- Reduced risk of nerve damage due to real-time patient feedback.
- Less post-operative pain and discomfort.
- Shorter recovery times compared to traditional spine surgery.
Cosmetic Procedures Under Local Anesthesia
Cosmetic surgeries like facelifts, breast augmentations, and liposuction are now done under local anesthesia. This makes the experience more comfortable and safer. It avoids the dangers of general anesthesia.
Awake Brain Surgery: A Detailed Examination
Awake brain surgery is a complex technique. It uses detailed brain mapping and feedback from the patient. The patient must be awake and able to respond during parts of the surgery. This lets the team check how the brain is working in real-time.
Why Consciousness Is Necessary
Being awake during surgery is key. It lets the team watch brain areas that control important functions like speech and movement. This way, surgeons can map the brain and keep these functions safe.
Brain mapping helps find and protect brain areas. It’s very important when surgery is near areas that control speech and movement. The patient’s input helps the surgeons avoid damaging these areas.
Brain Mapping During Surgery
Brain mapping is a big part of awake brain surgery. It uses different methods to find and protect brain areas. Some methods include:
- Direct electrical stimulation to check brain function
- Functional MRI (fMRI) to find important brain areas before surgery
- Intraoperative neurophysiological monitoring to watch brain activity during surgery
These methods help create a detailed map of the brain. This map guides the surgeons during the surgery.
| Technique | Description | Benefits |
| Direct Electrical Stimulation | Electrical impulses are used to stimulate brain areas and assess their function. | Real-time feedback on brain function |
| Functional MRI (fMRI) | Imaging technique used before surgery to identify critical brain areas. | Preoperative planning and risk assessment |
| Intraoperative Neurophysiological Monitoring | Continuous monitoring of brain activity during surgery. | Immediate detection of possible neurological damage |
Patient Communication During the Procedure
Talking to the patient is very important during awake brain surgery. The patient does tasks like speaking and moving to help the team. A skilled anesthesiologist makes sure the patient is comfortable and can respond.
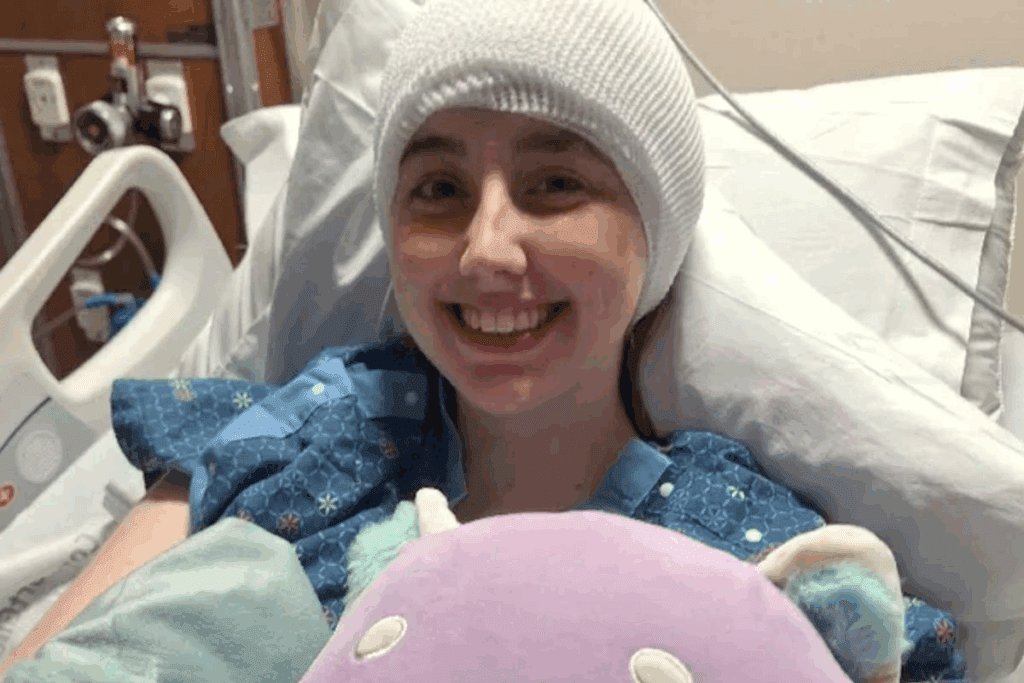
The Awake Surgery Experience: Patient Perspectives
Many patients find awake surgery surprisingly positive. Their stories show both the tough parts and the good surprises. This gives a full picture of what it’s like.
Common Concerns and Fears
Patients often worry about pain and being awake during surgery. They fear feeling pain and being awake during the procedure.
| Concern | Patient Experience |
| Pain during surgery | Most patients report feeling pressure but not pain, thanks to effective local anesthesia. |
| Anxiety about being awake | Patients often express initial anxiety, but many find the experience less daunting than expected, thanks to psychological support. |
Benefits of Choosing Awake Surgery
Awake surgery is becoming more popular because of its many benefits. It can make a patient’s surgery and recovery better. The advantages include less time to recover and better results.
Reduced Recovery Time
One big plus of awake surgery is quicker recovery. Patients wake up faster because they weren’t in deep sleep. They can start doing normal things sooner.
Research shows awake surgery patients stay in the hospital less. They also face fewer problems after surgery. This is because they use less medicine and less invasive methods.
Lower Risks Compared to General Anesthesia
Awake surgery is safer than traditional surgery under deep sleep. Deep sleep can lead to breathing problems, allergic reactions, and longer recovery times.
By not using deep sleep, patients face fewer risks. They also get closer to their health during surgery.
Improved Surgical Outcomes
Awake surgery lets patients give feedback in real time. This is very helpful in precise surgeries like brain surgery.
This feedback helps surgeons make better choices. It leads to better results. The teamwork between patient and surgeon makes treatment more effective.
Cost Advantages
Awake surgery can also save money. It needs less deep sleep medicine and shorter hospital stays. This makes it cheaper.
| Aspect | Awake Surgery | Traditional Surgery |
| Recovery Time | Shorter | Longer |
| Risks | Lower | Higher |
| Surgical Outcomes | Improved | Variable |
| Cost | Potentially Lower | Higher |
In conclusion, awake surgery is a good choice for many. Knowing its benefits helps patients decide better for their surgery.
Potential Discomforts and Limitations
Awake surgery has many benefits, but it also comes with some challenges. We want to give you a clear view of these aspects. This way, you can make a well-informed decision.
Physical Challenges During Procedures
Awake surgery can be physically demanding. Patients might feel discomfort from staying in one position for a long time. They might also feel pressure or pulling sensations at the surgical site, even though it’s numb. We use precise anesthesia and careful positioning to reduce these issues.
Some surgeries, like awake brain surgery, require patients to stay awake and alert. This means they have to stay very calm and not move while the doctors work. Our team works closely with patients to make sure they’re comfortable and can follow instructions.
Psychological Aspects of Being Conscious
Being awake during surgery can also affect your mind. Patients might feel anxiety or worry about being awake. We offer psychological support, like counseling and relaxation techniques, to help them prepare and cope.
Everyone’s experience of being awake during surgery is different. Some might feel in control and empowered, while others might feel fear or unease. Our team aims to create a supportive environment. We want to make sure patients feel cared for and supported throughout the process.
It’s important to understand the possible discomforts and limitations of awake surgery. Knowing what to expect can help patients prepare better. This can lead to a more positive experience for them.
Ideal Candidates for Awake Surgery
Finding the right candidates for awake surgery is complex. It involves looking at many medical and psychological factors. Not everyone is a good fit, and choosing the right patients is key for success and safety.
Medical Considerations
When checking if a patient is right for awake surgery, several medical factors are looked at. These include the patient’s health, any other health issues, and the surgery’s purpose. For example, people with certain brain conditions might be good candidates. This is because awake brain surgery lets doctors watch the brain work during the surgery.
Key medical considerations include:
- The type and complexity of the surgical procedure
- The patient’s physical and neurological status
- Any previous surgical experiences or complications
Psychological Preparedness
Being mentally ready is also very important. Patients need to be able to follow the team’s instructions during surgery. This can be hard for those with anxiety or other mental health issues. Counseling and education before surgery can help prepare patients.
Factors influencing psychological preparedness include:
- The patient’s level of anxiety or fear regarding the procedure
- Their ability to remain calm and follow instructions during surgery
- Previous experiences with medical procedures
Contraindications and Risk Factors
Some conditions or situations might make awake surgery not suitable or riskier. These include severe anxiety, trouble staying calm during surgery, and some health issues that could make the surgery harder or the anesthesia riskier.
Contraindications and risk factors to be considered:
| Condition | Risk |
| Severe Anxiety | Inability to remain calm during the procedure |
| Claustrophobia | Discomfort or panic during the procedure |
In conclusion, finding the right candidates for awake surgery needs a detailed look at both medical and mental health factors. By carefully checking these, doctors can make sure patients are well-suited for awake surgery. This helps in getting better results and lowers risks.
Preparing for Your Awake Surgical Procedure
Getting ready for awake surgery is key. It’s about being physically and mentally prepared. We’ll show you how to get ready and what to expect.
Physical Preparation Steps
Being physically ready is important for a good surgery. We recommend a pre-op plan that includes:
- Eating healthy foods to help with recovery
- Drinking lots of water to stay hydrated
- Not doing too much before surgery to avoid problems
- Following any special instructions from your doctor, like fasting or changing meds
It’s also key to talk about any health issues or meds with your doctor for safety.
Mental and Emotional Readiness
Mental and emotional prep is just as vital. Try meditation, deep breathing, or therapy to handle anxiety and stress.
Knowing what the surgery is and talking openly with your team can help too. We suggest asking questions and sharing your fears.
Essential Questions for Your Surgical Consultation
At your surgery talk, ask important questions. Think about asking:
- What are the risks and benefits of my awake surgery?
- How will they manage pain during the surgery?
- Who will help me during and after the surgery?
- What should I do after surgery to care for myself?
Being well-prepared makes your surgery and recovery better.
The Medical Team’s Role During Awake Surgery
The medical team is key to the success and safety of awake surgeries. These surgeries need a team effort from many medical professionals.
Surgeon Responsibilities
The surgeon leads the surgery. They do more than just the surgery. They talk to the patient and watch how they react.
The surgeon’s skill in understanding patient feedback is very important.
Anesthesiologist’s Critical Function
The anesthesiologist keeps the patient comfortable and safe. They use local anesthesia or sedation to keep the patient relaxed. The anesthesiologist must adjust the sedation to keep the patient calm but awake.
Support Staff and Communication
Good communication is essential during awake surgery. Nurses, anesthesiologists, and others work together. They help anticipate and meet the patient’s needs, making the surgery safer and more successful.
Support staff also helps the patient feel less anxious. This makes the surgery smoother for the patient.
Knowing the roles of the medical team in awake surgery helps patients understand the care they receive. The team’s work together is vital for the best results for patients.
Recovery After Awake Surgery
Recovering from awake surgery is a journey with many steps. It includes care right after surgery, healing in the short term, and long-term results. Knowing what to expect at each stage is key.
Immediate Post-Procedure Experience
Right after surgery, patients go to a recovery area. There, doctors watch their health closely. They make sure patients are comfortable and pain-free.
Common experiences during this phase include:
- Mild pain or discomfort at the surgical site
- Drowsiness or fatigue due to sedation
- Nausea or dizziness
Our team is ready to help with these issues. They give medicine or other help as needed to keep patients comfortable.
Short-term Recovery Timeline
The first few days to weeks after surgery are the short-term recovery. This time varies based on the surgery and the patient. Patients must follow specific instructions to heal well.
| Day | Expected Recovery Progress | Care Instructions |
| 1-2 | Rest and initial healing | Rest, avoid strenuous activities |
| 3-7 | Gradual improvement, reduction in pain | Continue rest, follow medication schedule |
| 7-14 | Significant improvement, return to light activities | Resume light activities, attend follow-up appointments |
Long-term Outcomes and Follow-up
Most patients see big improvements after awake surgery. We check on them at follow-up visits. This helps us catch any problems early.
It’s important for patients to follow our instructions and keep their follow-up appointments. This helps ensure the best recovery.
Understanding the recovery process helps patients prepare. It makes the healing journey smoother and more successful.
Advancements in Awake Surgery Techniques
The world of awake surgery is changing fast. New technologies and a better understanding of patient needs are driving these changes. Awake surgery is leading the way, bringing better results and new options for patients.
Technological Innovations
New technologies are key to improving awake surgery. Intraoperative imaging technologies like functional MRI and real-time ultrasound help surgeons see better. This means they can work on complex areas with more accuracy.
Electrophysiological monitoring is another big step. It lets surgeons check how important nerves are working during surgery. This makes awake surgery safer and more precise.
Future Directions in Minimally Invasive Procedures
Looking ahead, awake surgery will get even better with minimally invasive techniques. These methods cause less damage and help patients recover faster. They’re being used more in awake surgery.
| Technique | Benefits | Future Applications |
| Intraoperative Imaging | Enhanced precision, real-time feedback | Expanded use in complex surgeries |
| Electrophysiological Monitoring | Improved safety, functional preservation | Integration with AI for predictive analytics |
| Minimally Invasive Techniques | Reduced recovery time, less tissue damage | Broader application in various surgical specialties |
These new steps are making awake surgery better and more available. As the field grows, we’ll see even more creative ways to improve it. This will bring even more benefits to patients.
Conclusion
Awake surgery has many benefits, like shorter recovery times and fewer risks than general anesthesia. We’ve looked at different parts of awake surgery, like the types of anesthesia and who can have it.
Awake surgery might seem scary, but it’s safe and works well for many people. Knowing about pain control, the medical team’s role, and new techniques helps patients choose wisely.
In short, awake surgery is a big step forward in medicine. It offers many advantages but needs careful thought for each patient. As technology gets better, we’ll see even more improvements in awake surgery, making care better for everyone.
FAQ
Is awake surgery painful?
Awake surgery is not usually painful. This is because local anesthesia and other pain control methods are used. Patients might feel some pressure or sensations, but these are usually not too uncomfortable.
What is the difference between pain and pressure sensations during awake surgery?
Pain is a sharp, uncomfortable feeling. Pressure sensations are more like a dull ache or feeling of tension. During awake surgery, patients might feel pressure, but it’s not usually painful.
What types of anesthesia are used in awake surgery?
Local anesthesia, regional nerve blocks, and conscious sedation are used in awake surgery. These help keep patients comfortable and reduce discomfort.
How is pain managed during awake surgery?
To manage pain, several methods are used. These include pre-operative medications, pain control during the surgery, and psychological support. These help keep patients comfortable during awake surgery.
What are the benefits of choosing awake surgery?
Choosing awake surgery has many benefits. It can lead to faster recovery times and lower risks compared to general anesthesia. It also might improve surgical outcomes and could be more cost-effective.
Who is a good candidate for awake surgery?
Good candidates for awake surgery are those who are medically fit and mentally prepared. They should not have any conditions that would make the surgery unsafe.
How can I prepare for awake surgery?
To prepare, follow physical preparation steps and mentally and emotionally get ready. Also, ask important questions during your surgical consultation.
What is the role of the medical team during awake surgery?
The medical team, including the surgeon, anesthesiologist, and support staff, are key to the success and safety of awake surgery. They focus on effective communication and patient care.
What can I expect during recovery after awake surgery?
After the surgery, you might feel some discomfort. But, the recovery time is usually short. The long-term outcomes are often very good.
Is awake surgery painful?
Awake surgery is not usually painful. This is because local anesthesia and other pain control methods are used. Patients might feel some pressure or sensations, but these are usually not too uncomfortable.
What is the difference between pain and pressure sensations during awake surgery?
Pain is a sharp, uncomfortable feeling. Pressure sensations are more like a dull ache or feeling of tension. During awake surgery, patients might feel pressure, but it’s not usually painful.
What types of anesthesia are used in awake surgery?
Local anesthesia, regional nerve blocks, and conscious sedation are used in awake surgery. These help keep patients comfortable and reduce discomfort.
How is pain managed during awake surgery?
To manage pain, several methods are used. These include pre-operative medications, pain control during the surgery, and psychological support. These help keep patients comfortable during awake surgery.
What are the benefits of choosing awake surgery?
Choosing awake surgery has many benefits. It can lead to faster recovery times and lower risks compared to general anesthesia. It also might improve surgical outcomes and could be more cost-effective.
Who is a good candidate for awake surgery?
Good candidates for awake surgery are those who are medically fit and mentally prepared. They should not have any conditions that would make the surgery unsafe.
How can I prepare for awake surgery?
To prepare, follow physical preparation steps and mentally and emotionally get ready. Also, ask important questions during your surgical consultation.
What is the role of the medical team during awake surgery?
The medical team, including the surgeon, anesthesiologist, and support staff, are key to the success and safety of awake surgery. They focus on effective communication and patient care.
What can I expect during recovery after awake surgery?
After the surgery, you might feel some discomfort. But, the recovery time is usually short. The long-term outcomes are often very good.
Is awake surgery painful?
Awake surgery is not usually painful. This is because local anesthesia and other pain control methods are used. Patients might feel some pressure or sensations, but these are usually not too uncomfortable.
What is the difference between pain and pressure sensations during awake surgery?
Pain is a sharp, uncomfortable feeling. Pressure sensations are more like a dull ache or feeling of tension. During awake surgery, patients might feel pressure, but it’s not usually painful.
What types of anesthesia are used in awake surgery?
Local anesthesia, regional nerve blocks, and conscious sedation are used in awake surgery. These help keep patients comfortable and reduce discomfort.
How is pain managed during awake surgery?
To manage pain, several methods are used. These include pre-operative medications, pain control during the surgery, and psychological support. These help keep patients comfortable during awake surgery.
What are the benefits of choosing awake surgery?
Choosing awake surgery has many benefits. It can lead to faster recovery times and lower risks compared to general anesthesia. It also might improve surgical outcomes and could be more cost-effective.
Who is a good candidate for awake surgery?
Good candidates for awake surgery are those who are medically fit and mentally prepared. They should not have any conditions that would make the surgery unsafe.
How can I prepare for awake surgery?
To prepare, follow physical preparation steps and mentally and emotionally get ready. Also, ask important questions during your surgical consultation.
What is the role of the medical team during awake surgery?
The medical team, including the surgeon, anesthesiologist, and support staff, are key to the success and safety of awake surgery. They focus on effective communication and patient care.
What can I expect during recovery after awake surgery?
After the surgery, you might feel some discomfort. But, the recovery time is usually short. The long-term outcomes are often very good.
Is awake surgery painful?
Awake surgery is not usually painful. This is because local anesthesia and other pain control methods are used. Patients might feel some pressure or sensations, but these are usually not too uncomfortable.
What is the difference between pain and pressure sensations during awake surgery?
Pain is a sharp, uncomfortable feeling. Pressure sensations are more like a dull ache or feeling of tension. During awake surgery, patients might feel pressure, but it’s not usually painful.
What types of anesthesia are used in awake surgery?
Local anesthesia, regional nerve blocks, and conscious sedation are used in awake surgery. These help keep patients comfortable and reduce discomfort.
How is pain managed during awake surgery?
To manage pain, several methods are used. These include pre-operative medications, pain control during the surgery, and psychological support. These help keep patients comfortable during awake surgery.
What are the benefits of choosing awake surgery?
Choosing awake surgery has many benefits. It can lead to faster recovery times and lower risks compared to general anesthesia. It also might improve surgical outcomes and could be more cost-effective.
Who is a good candidate for awake surgery?
Good candidates for awake surgery are those who are medically fit and mentally prepared. They should not have any conditions that would make the surgery unsafe.
How can I prepare for awake surgery?
To prepare, follow physical preparation steps and mentally and emotionally get ready. Also, ask important questions during your surgical consultation.
What is the role of the medical team during awake surgery?
The medical team, including the surgeon, anesthesiologist, and support staff, are key to the success and safety of awake surgery. They focus on effective communication and patient care.
What can I expect during recovery after awake surgery?
After the surgery, you might feel some discomfort. But, the recovery time is usually short. The long-term outcomes are often very good.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28162256/