Awake craniotomy is a surgical procedure where patients stay awake during part of the operation. It’s used to treat complex brain conditions. Knowing the disadvantages of this procedure is important for both patients and doctors.
Recent studies show awake craniotomy lets doctors watch critical brain functions in real-time. This might lower the chance of brain problems after surgery. But, the procedure also has its own challenges and risks.
Looking into awake craniotomy, we must consider its good points and bad points. This includes the risks of awake brain surgery
Key Takeaways
- Awake craniotomy is a complex procedure with unique challenges.
- The procedure allows for real-time monitoring of critical functions.
- Understanding the disadvantages is crucial for informed decision-making.
- Potential risks include neurological deficits and surgical complications.
- Patient selection and preparation are key to minimizing risks.
The Science Behind Awake Brain Surgery
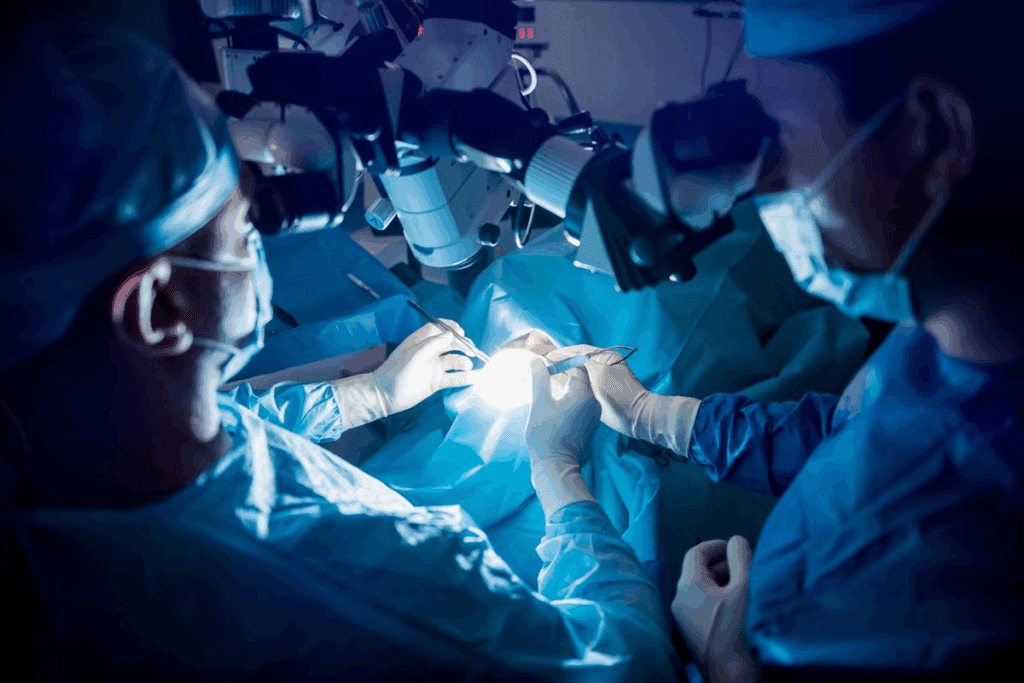
Awake brain surgery is a complex method that needs careful planning and patient cooperation. It involves removing or repairing damaged brain tissue while the patient is awake. This approach is crucial for precise surgery.
Definition and Medical Necessity
Awake brain surgery, also known as awake craniotomy, is a detailed procedure. It lets neurosurgeons work on the brain while the patient is awake. This is especially useful for surgeries near areas that control speech, movement, and sensation.
This surgery is needed when brain tumors, epilepsy, or other conditions require careful brain function preservation. Keeping the patient awake allows for real-time brain mapping. This helps in identifying and saving vital brain areas.
How the Procedure Works
At the start, the patient gets local anesthesia to numb the scalp and sedation to relax. As the surgery goes on, the sedation is adjusted to make the patient more alert. This “awake” phase is key for brain mapping and monitoring.
Brain mapping uses gentle electrical stimulation to find brain areas for specific functions. This helps surgeons safely remove or repair the targeted area. It prevents damage to surrounding brain tissue.
| Procedure Stage | Anesthesia and Sedation | Patient State |
| Initial Stage | Local anesthesia and sedation | Relaxed, not fully awake |
| Awake Phase | Adjusted or reversed sedation | Alert and responsive |
| Final Stage | Sedation resumed | Relaxed, less responsive |
When Doctors Recommend This Approach
Doctors choose awake brain surgery for several reasons. It’s often used when the condition affects critical brain areas or when traditional surgery risks are high. The decision is based on the patient’s health, the brain condition, and the benefits of real-time brain mapping.
Understanding awake brain surgery helps patients see its complexities and benefits. As medical technology advances, awake brain surgery remains a crucial treatment option. It offers hope and better outcomes for many patients.
The Awake Craniotomy Procedure Step by Step
Understanding the awake craniotomy procedure is key to seeing the care and precision in neurosurgery. This complex operation needs a skilled team and a well-planned approach. It ensures patient safety and successful results.
Pre-surgical Preparation and Assessment
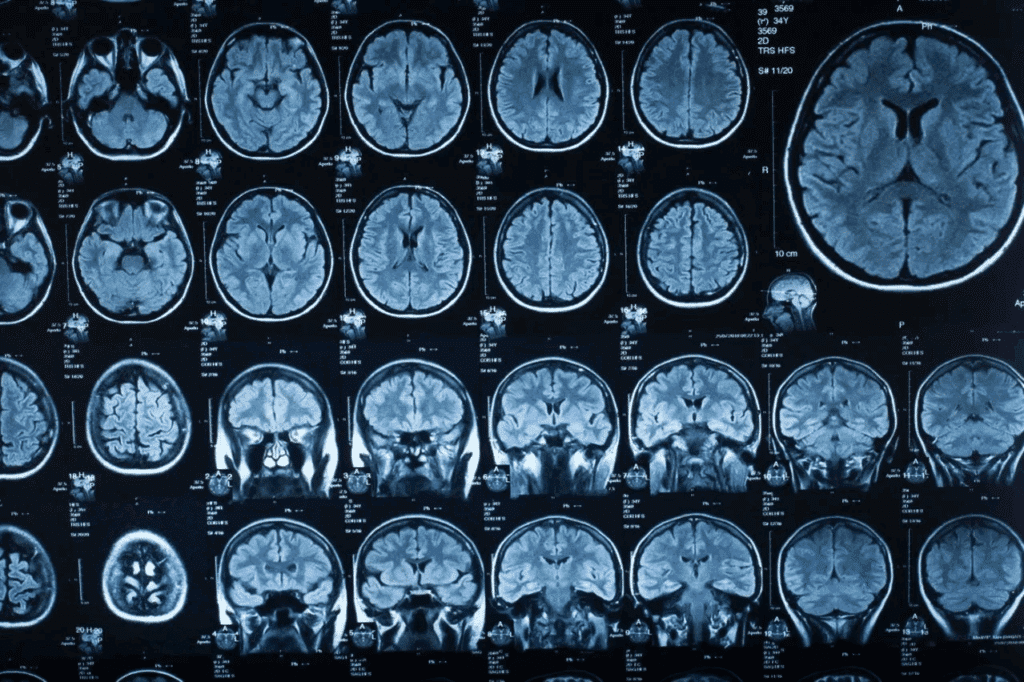
Before surgery, a detailed assessment is done. This includes a medical history, neurological checks, and imaging like MRI or CT scans. We use this info to plan the surgery carefully.
- Patient education on the procedure and what to expect
- Psychological evaluation to assess the patient’s ability to cooperate during the surgery
- Review of imaging studies to identify the location and extent of the brain lesion
Anesthesia Protocol: Asleep-Awake-Asleep Technique
The anesthesia for awake craniotomy is an “asleep-awake-asleep” method. The patient is first under general anesthesia, then awakened during the key part of surgery. This method ensures patient comfort and safety.
- Initial anesthesia induction to ensure patient comfort during the opening stages of surgery
- Awakening the patient for intraoperative brain mapping and tumor resection
- Re-induction of anesthesia for the closure phase
Patient Selection Limitations for Awake Brain Surgery
Choosing the right patients for awake craniotomy is key to success. It’s about looking at many factors to see if a patient is right for the surgery.
Medical Contraindications
Some medical issues make awake brain surgery not safe. These include neurological deficits, uncontrolled epilepsy, and big cardiovascular disease. These conditions can raise the risk of problems during surgery.
- Severe neurological deficits that could complicate intraoperative monitoring.
- Uncontrolled epilepsy, which may increase the risk of seizures during the surgery.
- Significant cardiovascular disease, posing risks related to the stress of the surgery.
Psychological Readiness Requirements
Being mentally ready is also very important. Patients need to be able to stay still and listen during the awake part of the surgery. They must have good cognitive function and emotional stability.
- Ability to remain still and follow commands during the procedure.
- Understanding and consenting to the procedure, which involves being aware of the potential risks and benefits.
- Emotional stability to cope with the stress and discomfort associated with being awake during surgery.
Age and Physical Condition Considerations
The age and health of the patient are also big factors. Older adults or those with significant physical limitations might find the surgery harder.
We look at the patient’s health, strength, and how well they can handle the surgery position. For example, those with severe arthritis or trouble staying still for a long time might not be the best fit.
Physical Discomfort During the Procedure
During an awake craniotomy, patients may face physical discomfort. The procedure requires them to be awake and still for a long time. This can cause several physical challenges.
Pain Management Challenges
Pain management is a big concern during awake craniotomy. Even with local anesthesia, patients might still feel pain or discomfort. It’s important to manage pain well to keep patients comfortable and cooperative.
“The key to successful awake craniotomy lies in meticulous pain management and creating a comfortable environment for the patient.”
Positioning Discomfort and Restrictions
Patients must stay in one position for a long time, which can be uncomfortable. This discomfort can be mild or severe. It might make it hard for patients to stay still, which can make the procedure harder.
To help, medical teams use different methods to keep patients comfortable. They adjust the operating table and use supportive devices to help patients stay in the right position.
Duration-Related Physical Stress
An awake craniotomy can last several hours. This long time can cause physical stress. It can come from being still for too long, discomfort from the surgery, and the stress of being awake during surgery.
To manage this stress, doctors use good pain management, comfortable positioning, and support for the mind. They watch patients closely to quickly address any problems.
Psychological Burden on Patients
Awake craniotomy is a valuable surgery but comes with big psychological challenges. Being awake during brain surgery is scary. It’s key to understand the psychological burden to give the best care.
Preoperative Anxiety and Fear
Preoperative anxiety is a big challenge for patients. The fear of being awake and worried about the outcome is huge. Studies show that high anxiety before surgery can make recovery harder.
“The fear of the unknown is a big part of preoperative anxiety,” a study found (1).
To help, doctors use counseling and relaxation techniques. These methods help patients get ready mentally for the surgery.
Intraoperative Psychological Stress
During surgery, patients feel intraoperative psychological stress. The unfamiliar setting and the surgery itself add to the stress. The team’s calm words and reassurance are key to lowering this stress.
Using guided imagery or music therapy can also make the atmosphere calmer.
Postoperative Trauma and PTSD Risk
After surgery, some patients might face postoperative trauma or PTSD. Being awake during surgery, though needed, can leave lasting psychological scars. It’s crucial to have follow-up care and support to manage these risks.
A study found that “early support can greatly lower the risk of long-term psychological trauma in awake craniotomy patients” (2).
Understanding and tackling the psychological burden helps healthcare providers give better care. This improves the experience and outcomes for those having awake craniotomy.
Intraoperative Complications of Awake Brain Surgery
Awake brain surgery is complex and comes with risks. We must handle these risks carefully. It’s important to know the risks and how to manage them.
Seizure Risks During the Procedure
Seizures are a big risk during awake brain surgery. They can happen due to brain stimulation or surgery-related factors. We use advanced brain mapping and watch the patient’s brain closely to reduce this risk.
Seizure management strategies include:
- Preoperative assessment to identify patients at higher risk
- Intraoperative electrocorticography to monitor seizure activity
- Ready availability of antiepileptic medications
Neurological Deficits and Brain Swelling
Neurological deficits or brain swelling can happen during or after surgery. These issues can come from the surgery, tumor location, or patient health. We use:
| Risk Factor | Management Strategy |
| Tumor Location | Advanced imaging and brain mapping |
| Surgical Technique | Microsurgical techniques and intraoperative monitoring |
| Patient Condition | Preoperative assessment and optimization |
Anesthesia-Related Complications
The “asleep-awake-asleep” anesthesia technique is used in awake brain surgery. It keeps the patient comfortable and allows for brain checks. But, it also has risks like airway problems and anesthesia issues.
Careful patient selection and meticulous anesthesia planning are key to avoiding these risks. Our team is skilled in managing these challenges to keep patients safe and comfortable.
Communication and Cooperation Challenges
The success of awake craniotomy depends a lot on the patient’s ability to work with the surgical team. This complex surgery needs not just medical skill but also teamwork between the patient and the doctors.
“Effective communication is key for any surgery, and awake craniotomy is no different,” say top neurosurgeons. The challenges in talking and working together can really affect the surgery’s success.
Language and Cognitive Testing Limitations
One big challenge in awake craniotomy is doing language and cognitive tests. These tests help check the brain’s function during surgery. But, there are some limits to these tests, such as:
- The complexity of tasks that patients can do while still and cooperative.
- The limited scope of tests that can be done in a short time.
- The chance of patient fatigue affecting test results.
We need to plan these tests carefully for each patient’s needs and condition.
Patient Cooperation Difficulties
Getting the patient to cooperate is key for awake craniotomy. But, it can be hard because of:
- Preoperative anxiety and fear.
- Discomfort or pain during the surgery.
- Difficulty in understanding or following instructions.
Good preoperative counseling and support during surgery are key to overcoming these challenges and getting patient cooperation.
Cultural and Language Barriers
Cultural and language barriers can make communication harder during awake craniotomy. We need to:
- Have staff or interpreters who speak many languages.
- Be aware of cultural differences and patient preferences.
- Use visual aids and simple language to help understanding.
By tackling these challenges ahead of time, we can improve patient cooperation and the surgery’s success.
In conclusion, while communication and cooperation challenges are big in awake craniotomy, we can beat them with careful planning, patient education, and teamwork. This way, we can get the best results for our patients in this complex surgery.
Postoperative Recovery Complications
The time after an awake craniotomy is very important. It involves several complications that need careful management. This ensures the best outcomes for patients.
Immediate Recovery Challenges
Right after an awake craniotomy, managing pain is key. We also watch for signs of infection or swelling in the brain. Effective pain management is crucial for a smooth recovery.
We keep a close eye on patients for any neurological issues. These can range from mild weakness to severe impairments, depending on the brain area involved.
Long-term Physical Rehabilitation Needs
Many patients need long-term physical rehabilitation to regain lost functions. The amount of rehabilitation needed varies. It depends on the surgery’s complexity and the patient’s condition before surgery.
A good rehabilitation program includes physical, occupational, and speech therapy. It’s tailored to the patient’s specific needs.
Psychological Recovery Issues
Psychological recovery is also crucial. Patients may face anxiety, depression, or PTSD symptoms after the surgery. Supportive care, like counseling, is vital for these issues.
We stress the need for a supportive environment. This is true both at the hospital and at home. It helps patients deal with the psychological challenges of recovery.
In conclusion, the recovery after an awake craniotomy is complex. It requires a detailed approach to manage both physical and psychological challenges effectively.
Surgical Team Expertise Requirements
Awake craniotomy is a complex task that needs a lot of expertise from the surgical team. It requires a skilled neurosurgeon and a team of anesthesiologists, nurses, and other healthcare professionals working together.
Specialized Training and Experience Needed
The surgical team must get specialized training for awake craniotomy. They need to know about asleep-awake-asleep anesthesia, keeping the patient comfortable, and doing intraoperative brain mapping and monitoring.
- Training in awake craniotomy techniques
- Experience with intraoperative neurophysiological monitoring
- Familiarity with patient communication strategies during the procedure
This specialized training helps the team handle awake craniotomy’s unique challenges. It improves patient outcomes.
Team Communication Complexity
Good team communication is key in awake craniotomy. The team must work together to watch the patient’s neurological status, adjust anesthesia, and perform the surgery with precision.
Important parts of team communication include:
- Clear and concise updates on the patient’s status
- Preoperative briefing to discuss potential challenges
- Coordination between the neurosurgeon, anesthesiologist, and nursing staff
Seamless team communication helps reduce risks and improves the procedure’s success.
Surgeon Stress and Decision Fatigue
Surgeon stress and decision fatigue are big concerns in awake craniotomy. The neurosurgeon must make quick decisions based on real-time feedback and monitoring, all while staying focused for a long time.
- Preoperative planning and simulation
- Intraoperative support from experienced teams
- Postoperative debriefing to discuss challenges and outcomes
By understanding and tackling surgeon stress, hospitals can help their surgical teams provide the best care.
Institutional and Resource Limitations
The success of awake craniotomy depends on many factors. These include the resources and facilities available. We will explore what makes this procedure work well.
Specialized Facility Requirements
Awake craniotomy needs a place with top-notch neurosurgical tools. A team skilled in neuroanesthesia and neuromonitoring is also key. Specialized facilities are vital for safety and success.
These places must be ready for any problems that might happen. Having the latest equipment and trained staff is essential for a good outcome.
Equipment and Technology Needs
The tools needed for awake craniotomy are very specific. This includes MRI and intraoperative MRI for precise tumor location. Intraoperative neuromonitoring is also crucial for checking brain activity during surgery.
- Advanced imaging technologies
- Intraoperative neuromonitoring equipment
- Specialized neurosurgical instruments
These technologies make the surgery safer and more effective. They help in achieving better results for patients.
Cost and Insurance Considerations
The cost of awake craniotomy is high. It depends on the facility, the team, and the technology used. Insurance is key to making it affordable for patients.
Thinking about the cost and insurance is important. The complexity of the surgery and the need for specialized care affect what patients pay.
| Factor | Impact on Cost |
| Facility Charges | High |
| Surgical Team Fees | High |
| Advanced Technology | Moderate to High |
Comparing Awake Craniotomy to Alternative Approaches
Awake craniotomy and other surgical methods have their own benefits and challenges. It’s important to look at the unique advantages and issues of each method.
Traditional Craniotomy Under General Anesthesia
Traditional craniotomy uses general anesthesia. This is for patients who can’t have awake craniotomy due to health or mental reasons.
Key differences between awake craniotomy and traditional craniotomy include:
| Criteria | Awake Craniotomy | Traditional Craniotomy |
| Patient State | Awake and responsive | Fully anesthetized |
| Intraoperative Monitoring | Real-time brain function monitoring | No intraoperative brain function monitoring |
| Recovery Time | Generally shorter recovery | Longer recovery due to anesthesia |
Minimally Invasive Surgical Options
Options like stereotactic radiosurgery or endoscopic surgery are less invasive. They might have fewer complications and quicker recovery. But, they might not work for all brain issues.
The choice between awake craniotomy and minimally invasive surgery depends on various factors, including the nature and location of the lesion, patient health, and surgical team expertise.
When Benefits Outweigh the Disadvantages
Awake craniotomy’s benefits, like real-time brain mapping, often outweigh its drawbacks for the right patients. It allows for more precise surgery and helps avoid harming important brain areas.
Choosing awake craniotomy should be a careful decision. It should be made after talking to a neurosurgeon and considering the patient’s needs and the brain issue’s specifics.
Technological and Procedural Advancements
Technological innovations are changing awake craniotomy procedures. Medical technology keeps getting better. This leads to improved surgical techniques and better patient experiences.
Emerging Technologies Addressing Current Limitations
New neuroimaging and brain mapping technologies are making awake craniotomy more precise. Functional MRI (fMRI) and diffusion tensor imaging (DTI) help see brain structures and functions better. This lets surgeons plan and do surgeries more accurately, lowering the risk of brain damage.
Intraoperative MRI is also being used in awake craniotomy. It lets surgeons see the brain in real-time during surgery. This helps them check how much of the tumor or lesion they’ve removed and make changes if needed.
Improved Protocols for Patient Comfort and Safety
There are also new ways to make patients more comfortable and safe during awake craniotomy. The asleep-awake-asleep technique lets patients relax during the start and end of surgery. They are awake only during the most important part.
Better pain management is another big improvement. Doctors use new anesthetic methods and medicines to control pain without serious side effects. Patient-controlled analgesia (PCA) also lets patients control their pain during surgery.
Monitoring and support for patients during awake craniotomy are getting better too. Techniques like electrocorticography (ECoG) give feedback on brain activity in real-time. This helps avoid brain injuries. Also, having a neuroanesthesiologist and a skilled nursing team ensures patients get the best care.
Conclusion
Awake craniotomy is a complex surgery with big benefits for some patients. But, it also has its downsides. We’ve talked about the challenges, like physical pain, mental stress, and risks during surgery.
Choosing the right patients, having skilled doctors, and improving technology are key. These steps help lessen the problems. Looking ahead, we need more innovation to make the surgery better and help more people.
By tackling the challenges of awake craniotomy, we can improve care for those undergoing it. This means better technology and surgical methods. Our goal is to give the best care possible to these patients.
FAQ
Are you awake during brain surgery?
Yes, in awake craniotomy, patients are awake during part of the surgery. This lets the team map and monitor the brain. It helps them keep important brain functions safe.
Are there alternatives to awake craniotomy?
Yes, there are other options like traditional surgery under general anesthesia and less invasive methods. The choice depends on the patient’s condition and the brain issue.
What are the benefits of awake brain surgery?
Benefits include more precise tumor removal and keeping important brain functions safe. It can also lead to shorter recovery times. Awake craniotomy gives real-time feedback during surgery.
How long does it take to recover from awake brain surgery?
Recovery times vary based on the surgery’s extent and the individual. Good postoperative care, including physical and mental support, is key for a good recovery.
Is awake brain surgery risky?
Like any surgery, awake craniotomy has risks. But, with the right patient selection, skilled teams, and new technology, these risks can be managed well.
What kind of anesthesia is used in awake craniotomy?
The asleep-awake-asleep technique is often used. It involves general anesthesia at the start and end, with the patient awake during the brain mapping phase.
Can anyone undergo awake brain surgery?
No, choosing the right patients is crucial. Doctors consider medical issues, mental readiness, age, and physical condition to decide if someone can have awake craniotomy.
What are the institutional requirements for performing awake craniotomy?
Specialized facilities, advanced equipment, and skilled staff are needed. The quality of these resources can affect the surgery’s success.
How is patient cooperation ensured during awake craniotomy?
Ensuring cooperation involves good preoperative preparation, clear communication, and sometimes sedation. These help manage anxiety and stress during the surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7955997/


































