Craniotomy Positioning
Did you know that nearly 200,000 craniotomy procedures are done every year in the United States? The success of these operations depends a lot on precise surgical techniques. This includes patient positioning. The right surgical positioning techniques are key for the neurosurgeon to reach the brain safely. Learn which position is given in Craniotomy Positioning surgery. Understand how the head is positioned based on the location of the tumor clearly.
Patient positioning in surgery is very important. It needs careful planning and execution. In this guide, we’ll look at the key parts of craniotomy positioning. We’ll cover its importance, techniques, and best practices.
Key Takeaways
- Understanding the importance of patient positioning in craniotomy procedures.
- Exploring the different positions used for craniotomy surgeries.
- Discussing the equipment and devices used for optimal positioning.
- Best practices for achieving precise surgical positioning.
- The role of surgical teams in ensuring patient safety during craniotomy.
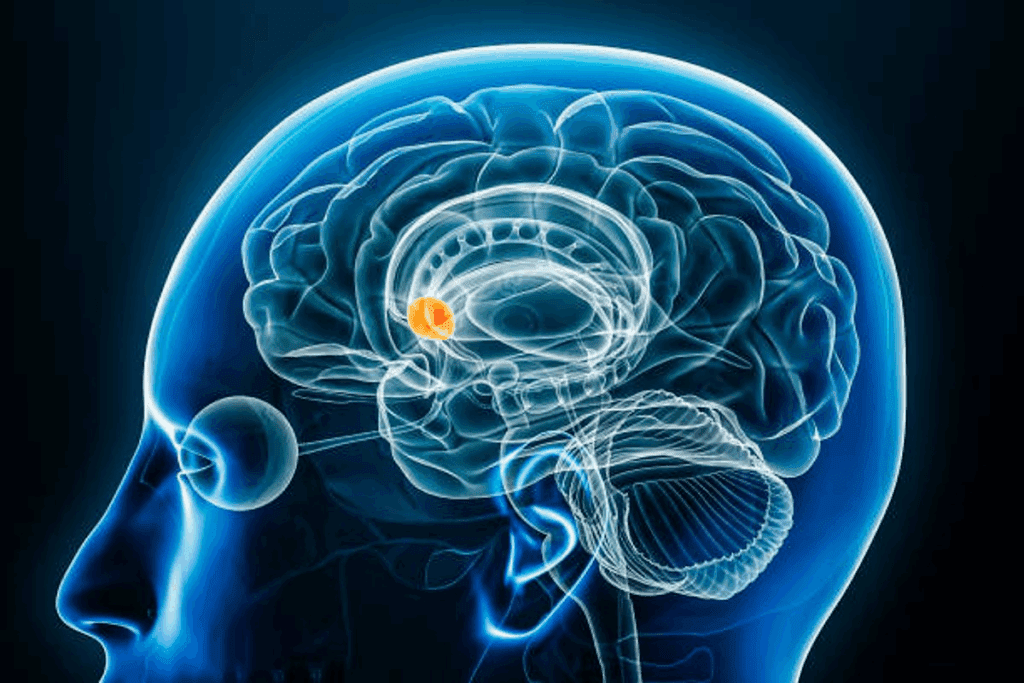
Understanding Craniotomy: Definition and Purpose

A detailed surgical view of a craniotomy procedure, showing careful exposure of the skull and brain tissue. The scene is meticulously lit, creating a clinical and professional atmosphere. The surgical instruments are precisely positioned, reflecting the surgeon’s expertise. The subject’s head is tilted to the side, allowing for a clear view of the incision and bone flap removal. The surrounding area is sterile and pristine, with medical equipment and monitors visible in the background. The image conveys the gravity and complexity of this delicate neurosurgical operation.
A craniotomy is a surgery where a part of the skull is taken off to reach the brain. It’s done for many brain issues like tumors, aneurysms, and injuries. Knowing about craniotomy helps us understand neurosurgery better.
What is a Craniotomy?
A craniotomy is a surgery where part of the skull is removed. This lets surgeons get to the brain. It’s needed for conditions that other treatments can’t fix. By taking off a skull part, surgeons can do operations that are hard or impossible otherwise.
Common Indications for Craniotomy
Craniotomies are done for many reasons. These include removing brain tumors, fixing aneurysms, and easing pressure from injuries. Doctors decide on a craniotomy after checking with tests like MRI or CT scans. Emergency craniotomy is needed for serious conditions like acute subdural hematoma.
Some common reasons include:
- Brain tumors
- Aneurysms
- Traumatic brain injuries
- Seizure disorders
Types of Craniotomy Procedures
There are many types of craniotomy surgeries. Each one is for a specific need. For example, supratentorial craniotomy is for the upper brain, and infratentorial craniotomy is for the lower parts. There are also occipital craniotomy and parietal craniotomy for different brain areas.
The type of craniotomy depends on the condition’s location and the patient’s health. Knowing these details is key for both doctors and patients to understand neurosurgery.
The Importance of Proper Patient Positioning in Craniotomy
A patient lying on their side, head slightly elevated, with a surgical drape covering the exposed area. The surgical site is clearly visible, with a focused light illuminating the area. The patient’s head is positioned with precision, supported by a specialized headrest or stabilizer. The room is sterile and well-lit, creating a clinical atmosphere. The angle of the image showcases the importance of proper patient positioning, highlighting the attention to detail required for a successful craniotomy procedure.
Proper patient positioning in craniotomy is very important. It affects how well the surgeon can see and how much pressure is in the brain. We will look at why it’s key for good surgery results.
Impact on Surgical Access and Visualization
Getting the patient’s position right is crucial for the surgeon. It helps them see better and makes the surgery easier. Adequate positioning can lead to better results for the patient.
“The positioning of the patient is a critical aspect of neurosurgery, as it directly affects the surgeon’s ability to access the target area safely and efficiently.”
— Neurosurgery Guidelines
Effects on Intracranial Pressure
How the patient is positioned can change the pressure inside the brain. Careful positioning can help keep this pressure stable. For example, raising the head can lower the pressure, while the wrong position can increase it.
| Positioning Technique | Effect on ICP |
| Head elevation | Decreased ICP |
| Neutral neck position | Optimal ICP management |
| Extreme flexion or extension | Increased ICP |
Influence on Patient Safety and Outcomes
The way a patient is positioned during a craniotomy greatly affects their safety and outcome. The right position can lower the risk of problems like nerve damage. It also helps the patient recover better, as shown in post craniotomy nursing care guidelines.
Understanding the importance of proper positioning in craniotomy helps improve surgery results and patient safety. This shows the need for careful attention to detail in patient positioning.
Craniotomy Positioning: Fundamental Principles and Considerations
A patient lying on an operating table, their head securely positioned with a Mayfield skull clamp, in preparation for a craniotomy procedure. The surgical field is illuminated by a bright, focused overhead light, casting sharp shadows and highlighting the contours of the patient’s anatomy. The surgical team, in sterile attire, stands ready with their instruments, creating a sense of clinical precision and professionalism. The background is blurred, emphasizing the central focus on the patient’s head and the critical positioning required for the delicate neurosurgical intervention.
Positioning a patient for craniotomy is a delicate task. It involves many factors like anatomy, physiology, and the patient’s health. Getting the positioning right is key for a successful surgery and the patient’s recovery.
Anatomical Considerations
Understanding the patient’s skull anatomy is crucial. The surgical team must know where the problem is and plan the best approach. Head positioning is especially important for access and clear views.
Headrest systems in craniotomy are vital for keeping the patient in the right spot. They provide support and can be adjusted during the surgery.
Physiological Factors
Physiological factors are also key in positioning for craniotomy. The team must think about how different positions affect pressure, blood flow, and breathing. For example, some positions might lower pressure or affect blood flow. Careful planning is needed to keep the patient stable.
Patient-Specific Factors
Every patient’s needs are different in craniotomy positioning. The team must consider the patient’s health, age, and any past medical issues. For instance, some patients might need special positioning due to heart or lung problems. The team must adapt their approach for each patient’s unique situation.
Standard Positions for Craniotomy Procedures
Supratentorial craniotomy position: A patient lies supine with their head secured in a rigid frame, exposing the crown of the skull. The scalp is cleanly shaved, and the surgical site is meticulously draped, revealing only the necessary area. Bright surgical lights illuminate the field, casting sharp shadows that accentuate the contours of the skull. The camera captures this precise, clinical scene from an elevated angle, conveying the gravity and technicality of the procedure.
Craniotomy procedures use different positions, each with its own benefits. The position chosen depends on the surgery’s location, type, and the patient’s health.
Supine Position
The supine position is very common in craniotomy surgeries. It has the patient lying on their back. This gives great access to the frontal, parietal, and temporal regions.
This position is best for supratentorial craniotomy. It’s above the tentorium cerebelli. It’s also good for the airway, making it a top choice for anesthesiologists.
Prone Position
The prone position has the patient on their stomach. It’s used for surgeries in the occipital region or the posterior fossa. However, it can be tricky because of airway risks and pressure injuries.
To avoid these problems, careful padding and airway security are key. This position helps reach the brain’s posterior parts.
Lateral Position
The lateral position has the patient on their side. It’s great for surgeries on the brain’s lateral side, like some temporal lobe surgeries.
This position can be adjusted for better access. It’s important to align the patient’s body to prevent neck and spine strain.
In summary, picking the right position for craniotomy is crucial. It depends on the surgery’s location and the patient’s health. Knowing the pros and cons of each position is key for the best surgical results.
Specialized Craniotomy Positions
a high-resolution, realistic, cinematic photograph of a person lying on their back on a wooden park bench, in a specialized surgical position for a craniotomy procedure. The person’s head is tilted back slightly, with their neck extended and the back of their head resting on the bench. Their arms are at their sides, palms facing up. The bench is situated in a peaceful, picturesque park setting, with lush green trees and bushes in the background. Soft, warm lighting illuminates the scene, creating a serene and clinical atmosphere. The perspective is from a slightly elevated angle, allowing the viewer to see the specialized position of the person on the bench in detail.
Specialized positions like the park bench, sitting, and semi-sitting are key in craniotomy procedures. They offer unique benefits for reaching specific brain areas.
Park Bench Surgical Position
The park bench position is a twist on the lateral decubitus position. It’s used for surgeries on the posterior fossa or cerebellum. This setup gives great access to these areas while keeping the patient stable.
Key Features of the Park Bench Position:
- Patient lies on their side with the dependent arm secured
- The head is fixed in a Mayfield skull clamp
- The upper leg is flexed, while the lower leg remains straight
Sitting Position
The sitting position is used for surgeries on the posterior fossa or cervical spine. It provides great exposure and cuts down on venous bleeding.
Advantages and Considerations:
- Improved surgical access to midline structures
- Reduced venous pressure
- Requires careful monitoring for air embolism
Semi-sitting Position
The semi-sitting position is a mix between sitting and supine positions. It’s used for similar reasons as the sitting position. It strikes a balance between access and safety.
| Position | Surgical Access | Patient Safety Considerations |
| Park Bench | Posterior fossa, cerebellum | Stability, nerve compression |
| Sitting | Posterior fossa, cervical spine | Air embolism, hemodynamic stability |
| Semi-sitting | Posterior fossa, cervical spine | Balance between access and safety |
Positioning for Specific Craniotomy Types
A patient lying on an operating table, their head secured in a specialized cranial positioning frame. The surgical area is shaved and sterilized, with a sterile drape covering the patient’s face and exposing the surgical site. Bright surgical lights illuminate the scene, casting a clean, clinical atmosphere. The surgeon and medical team are positioned around the patient, ready to perform the delicate craniotomy procedure. The image captures the precise positioning and setup required for this specialized neurosurgical operation, reflecting the technical details and focused intensity of the "Positioning for Specific Craniotomy Types" section.
Different craniotomy procedures need specific patient positioning. This is to get the best access and lower risks. The approach depends on the type of craniotomy, the area of the brain, and the surgical method.
Supratentorial Craniotomy Position
Supratentorial craniotomies access the upper brain. The patient is placed in a supine position with the head slightly up and turned to the other side. This reduces pressure and improves blood flow.
A neurosurgical expert says, “Proper positioning for supratentorial craniotomy is key. It helps avoid brain retraction and gets the best view.”
“The key to successful supratentorial craniotomy lies in the precise positioning of the patient, allowing for optimal access to the surgical site with minimal brain displacement.”
Infratentorial Craniotomy Position
Infratentorial craniotomies need different strategies. The park bench or semi-sitting position is often used. These positions reduce venous pressure and improve access.
The position chosen depends on the surgical approach and the patient’s anatomy. It’s important to avoid complications like air embolism in the sitting position.
Occipital Craniotomy Positioning
Occipital craniotomies access the back of the brain. Patients are placed in a prone or modified prone position for the best access. It’s crucial to manage the head and neck to prevent injuries.
- Ensure proper padding to prevent pressure points.
- Carefully manage the endotracheal tube to prevent displacement.
- Monitor for signs of neurovascular compromise.
Parietal Craniotomy Positioning
Parietal craniotomies access the parietal lobe. The positioning often involves a lateral or supine position with the head turned to expose the area. The goal is to give the surgeon the best access while avoiding complications.
Effective positioning for parietal craniotomy requires understanding the patient’s anatomy and the surgical plan. It’s crucial for a successful surgery.
Equipment and Devices for Optimal Craniotomy Positioning
A highly detailed, clinically accurate medical image of headrest systems used in craniotomy procedures, showcasing the precise mechanisms and components that ensure optimal positioning and support for the patient’s head during the surgery. The image should be captured from a slightly elevated angle, providing a comprehensive view of the headrest apparatus, including the adjustable base, padded cradle, and any specialized components designed to immobilize the head and neck. Crisp lighting and sharp focus should highlight the intricate engineering and high-quality materials used in the construction of these specialized medical devices. The overall tone should convey a sense of professionalism, attention to detail, and a commitment to patient safety and comfort during this delicate neurosurgical procedure.
For a successful craniotomy, the right equipment is key. Neurosurgical positioning devices and operating room gear are crucial. They help keep the patient stable and aligned, which is vital for the surgery’s success.
Headrest Systems in Craniotomy
Headrest systems are essential in craniotomy. They support and stabilize the patient’s head. This setup allows surgeons to work accurately on complex procedures.
Advanced headrest systems offer adjustable and lockable features. This adds stability and flexibility during surgery. It’s critical in procedures where small movements could be harmful.
Neurosurgical Positioning Devices
Neurosurgical positioning devices are made for optimal patient positioning. They’re designed to be flexible, fitting various patient positions and surgical methods.
| Device Type | Description | Application in Craniotomy |
| Adjustable Headrests | Allows for precise positioning and adjustment of the patient’s head. | Supratentorial and infratentorial craniotomies. |
| Body Supports | Provides additional support to maintain the patient’s position. | Lateral and prone positioning. |
| Surgical Tables | Specialized tables designed for neurosurgical procedures, offering flexibility and adjustability. | All types of craniotomies. |
Operating Room Positioning Equipment
Positioning equipment in the operating room is vital for craniotomy. It includes surgical tables, patient supports, and more. These tools work with neurosurgical devices to position patients perfectly.
Using advanced equipment ensures patients are positioned right. This improves surgical access and vision. Neurosurgeons can then perform craniotomy procedures more effectively, leading to better patient results.
Anesthesia for Craniotomy: Positioning Considerations
Effective anesthesia management is key during craniotomy procedures. It’s especially important when considering patient positioning. The way anesthesia and positioning work together can greatly affect the surgery’s success and the patient’s recovery.
Anesthetic Management During Positioning
During a craniotomy, managing anesthesia is crucial. We must watch and adjust the anesthesia as the patient’s position changes. This ensures the patient stays stable and avoids complications.
Important parts of managing anesthesia during positioning include:
- Keeping the brain’s blood flow optimal
- Controlling the pressure inside the skull through positioning and anesthesia
- Ensuring the patient gets enough oxygen and air
Monitoring During Position Changes
It’s vital to keep a close eye on the patient during position changes. We use different monitoring methods to quickly spot and fix any issues. These methods include:
| Monitoring Technique | Purpose |
| Electroencephalogram (EEG) | To watch the brain’s activity and catch any signs of trouble like ischemia or seizures |
| Invasive Blood Pressure Monitoring | To closely watch the blood pressure and make sure the brain gets enough blood |
| End-tidal CO2 Monitoring | To check how well the patient is breathing and spot any changes in CO2 levels that could affect the skull’s pressure |
Managing Complications Related to Positioning
Even with careful planning, problems can still happen due to positioning. We need to be ready to handle these issues quickly to lessen their impact on the patient’s outcome.
Common complications include:
- Air embolism
- Nerve injuries from bad positioning
- Stability problems with blood flow
Understanding anesthesia during craniotomy positioning helps us manage these complex procedures better. This improves patient care.
Craniotomy Precautions During Positioning
To keep patients safe during craniotomy, following best practices for positioning is key. It’s not just about getting to the brain. It’s also about avoiding problems that can happen during and after surgery.
Preventing Pressure Injuries
Pressure injuries are a big worry during long surgeries like craniotomy. We must protect patients by supporting their body and avoiding pressure points. Using the right padding and devices helps a lot.
Key strategies include checking the skin for pressure damage often. We also move the patient to avoid pressure on sensitive areas.
Avoiding Neurovascular Compression
Neurovascular compression can cause serious issues like nerve damage and blood flow problems. We position patients carefully to avoid this. We pay close attention to their body alignment and use supports to keep them in the right spot.
Managing Airway and Ventilation
Keeping the airway and ventilation working right is very important during craniotomy. We make sure the patient’s airway is safe and ventilation is good. This planning is done with the anesthesia team.
Preventing Venous Air Embolism
Venous air embolism is a serious risk during craniotomy, especially when patients are sitting or semi-sitting. We watch for signs of air embolism and use safe positions to lower the risk.
Knowing about venous air embolism and acting early can greatly improve patient safety during craniotomy.
Emergency Craniotomy: Positioning Considerations
When doing an emergency craniotomy, the team must position the patient fast and safely. Every second is crucial. The need for good intraoperative patient positioning is very important.
Rapid Positioning Techniques
Rapid positioning is key in emergency craniotomies. We use neurosurgical positioning devices for quick and secure positioning. These devices help get the patient in the best position for surgery safely.
Adjustable headrests and flexible tables let us make quick changes. This is crucial in emergencies where the patient’s needs can change fast.
Balancing Speed and Safety
Speed and safety must be balanced in emergency craniotomies. Quick action is needed, but safety is just as important. We follow protocols and use advanced neurosurgical positioning devices to keep both in check.
Good communication among the team is also key. It helps us position the patient correctly and safely.
Team Coordination in Emergency Situations
Teamwork is essential in emergency craniotomies. Clear communication among team members is vital. We focus on a coordinated approach to positioning, making sure everyone knows their role.
Working together, we can position the patient fast and safely. This improves the outcome of the emergency craniotomy.
Post-Operative Positioning for Craniotomy Patients
Proper positioning after craniotomy surgery is key to good outcomes. It helps prevent complications and aids in recovery. Careful thought goes into positioning to ensure the best results.
Immediate Post-Operative Positioning
Right after surgery, craniotomy patients need special care in their position. Elevating the head of the bed helps manage pressure and blood flow. This is a common method used.
It’s important to watch patients closely for any signs of trouble. Adjusting their position helps keep pressure and comfort levels right.
Post Craniotomy Nursing Care Related to Positioning
Nurses play a big role in caring for craniotomy patients after surgery. They check the patient’s brain function often. This helps avoid problems like pressure sores or nerve issues.
Frequent turning and repositioning are key to avoiding sores. Nurses also watch for breathing problems and manage airways well.
Transitioning to Recovery Positions
As patients get better, changing positions is important. It helps prevent issues and supports healing. We slowly move patients to more comfortable and useful positions.
It’s a balance between rest and movement. This helps avoid problems like blood clots or lung infections. Good positioning care improves patient outcomes and quality of life.
Complications and Outcomes Related to Craniotomy Positioning
It’s important to know about the problems that can happen with craniotomy positioning. This knowledge helps us improve care and results for patients. Craniotomy positioning can cause different issues, and knowing them helps us prevent and improve recovery.
Common Positioning-Related Complications
Craniotomy procedures need special positioning, which can lead to problems. These include:
- Pressure injuries from long-term pressure on certain body parts
- Neurovascular compression from bad alignment
- Issues with breathing and airways from head and neck positioning
Table 1: Common Complications and Their Prevention Strategies
| Complication | Prevention Strategy |
| Pressure Injuries | Regular repositioning, use of pressure-relieving devices |
| Neurovascular Compression | Careful alignment, monitoring of neurovascular status |
| Airway and Ventilation Issues | Proper head and neck positioning, continuous monitoring |
Prevention Strategies
To prevent problems with craniotomy positioning, we need a few steps. This includes planning before surgery, precise positioning, and watching the patient during the surgery. Optimizing patient alignment is key to lowering risks.
Impact on Patient Recovery and Quality of Life
The way a patient is positioned during a craniotomy affects their recovery and life quality after surgery. Good positioning can lower complication risks, making recovery better and long-term results better. We stress the need for optimizing head and neck positioning in brain surgery for the best results.
By knowing the possible problems and using good prevention methods, we can make patient outcomes and life quality after craniotomy better.
Conclusion
Proper craniotomy positioning is key in neurosurgery. It affects how well a patient does after surgery, their safety, and how fast they recover. We’ve looked at the basics, different positions, and the tools needed for the best results.
To do craniotomy positioning right, you need to know a lot about the body and each patient. Using the best methods and latest techniques helps doctors and nurses give better care. This leads to better results for patients.
As we get better at neurosurgery, keeping the right position is more important than ever. By focusing on the best positioning and following guidelines, we can make sure patients are safe and surgery is successful.
FAQ
What is the purpose of craniotomy positioning?
Craniotomy positioning aims to give the best access for surgery. It also helps keep pressure in the brain low and keeps the patient safe.
What are the standard positions used in craniotomy procedures?
Craniotomy procedures use three main positions: supine, prone, and lateral. Each has its own benefits and when to use them.
What is the park bench surgical position used for?
The park bench position is special. It’s used to reach certain brain areas, especially in surgeries of the lateral or posterior fossa.
How is patient positioning achieved during craniotomy?
To position patients for craniotomy, a mix of tools is used. These include headrests, neurosurgical devices, and equipment from the operating room.
What are the key considerations for anesthesia during craniotomy positioning?
Anesthesia during craniotomy needs careful planning. It involves managing anesthesia, monitoring changes, and handling any positioning-related issues.
What precautions are necessary during craniotomy positioning?
Important precautions include avoiding pressure injuries and neurovascular compression. It’s also crucial to manage airway and ventilation and prevent air embolism.
How is post-operative positioning managed for craniotomy patients?
Post-operative care for craniotomy patients focuses on positioning. It includes immediate care, nursing tasks related to positioning, and moving to recovery positions.
What are the common complications related to craniotomy positioning?
Common issues include pressure injuries, neurovascular compression, airway and ventilation problems, and air embolism.
How can complications related to craniotomy positioning be prevented?
To prevent complications, careful planning and precise positioning are key. Monitoring during and after the surgery is also vital.
What is the impact of craniotomy positioning on patient recovery and quality of life?
Good positioning in craniotomy can greatly improve recovery and quality of life. It reduces complications, pain, and promotes better neurological outcomes.
What is the role of team coordination in emergency craniotomy situations?
Teamwork is crucial in emergency craniotomies. It ensures quick and safe positioning and helps in clear communication among the team.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560922/










