
Nearly 1.9 million people have colorectal surgery every year in the U.S. Many are treated for colon cancer or diverticulitis. The thought of surgery can be scary, and knowing about anesthesia is key. Learn what kind of anesthesia colorectal surgery uses and how it ensures comfort during the procedure.
Colorectal surgery includes many types of procedures. Some are done with local anesthetics or sedation on an outpatient basis. Others are more complex and need general anesthesia in a hospital.
Key Takeaways
- The type of anesthesia used depends on the complexity and nature of the colorectal procedure.
- General anesthesia is commonly used for more complex surgeries.
- Patient comfort and safety are the top priorities during colorectal surgery.
- The choice between local, sedation, and general anesthesia is based on the patient’s health and the procedure’s needs.
- Knowing about anesthesia can help ease worries about colorectal surgery.
Understanding Colorectal Surgery and Anesthesia Basics
It’s important for patients to know about colorectal surgery and anesthesia before their procedures. These surgeries can range from simple to complex. They might need to stay in the hospital or go home the same day.
Common Types of Colorectal Procedures
There are many types of colorectal surgeries. Some are done in an outpatient setting. These include removing small skin tags, treating hemorrhoids, and draining abscesses.
Other surgeries are more serious. They might involve removing part or all of the colon. These are done in a hospital setting.
| Procedure Type | Setting | Description |
| Removing skin tags | Outpatient | Minor surgical removal of skin tags around the anus. |
| Rubber banding hemorrhoids | Outpatient | Procedure to treat internal hemorrhoids. |
| Botox injection for fissure | Outpatient | Injecting Botox to promote healing of anal fissures. |
| Draining an abscess | Outpatient | Draining infected abscesses in the colorectal area. |
| Colon removal surgery | Inpatient | Surgical removal of part or all of the colon. |
The Importance of Proper Anesthesia Management
Good anesthesia management is key for comfort and safety during colorectal surgery. The choice of anesthesia depends on the surgery, the patient’s health, and the surgeon’s choice. It helps reduce pain, anxiety, and stress.
Knowing about different surgeries and anesthesia helps patients prepare better. It makes them ready for the surgery and recovery.
Types of Anesthesia Used in Colorectal Surgery
Colorectal surgery can involve different types of anesthesia. This depends on the surgery’s complexity. Some surgeries are simple, while others, like bowel resections, are more complex.
General Anesthesia
General anesthesia is often used for complex surgeries like bowel resections in colon surgery. It makes sure the patient is completely asleep during the surgery.
Medications Used
General anesthesia uses several medications. These include propofol and sevoflurane to keep the patient unconscious.
Administration Methods
General anesthesia is given through intravenous injections and breathing in anesthetic gases.
Regional Anesthesia Options
Regional anesthesia, like epidural and spinal anesthesia, is another choice for colorectal surgery. It numbs a certain area of the body. This way, the patient doesn’t feel pain but isn’t asleep either.
Local Anesthesia Applications
For smaller surgeries, local anesthesia is used. It involves injecting anesthetic directly into the tissue at the surgery site. This numbs the area where the surgery is happening.
| Anesthesia Type | Application | Examples of Procedures |
| General Anesthesia | Major surgeries requiring full unconsciousness | Bowel resections, complex colon surgeries |
| Regional Anesthesia | Numbs a specific body region | Epidural for post-operative pain relief, spinal anesthesia for lower abdominal surgeries |
| Local Anesthesia | Minor procedures, numbs a small area | Simple colonoscopies, minor rectal surgeries |
General Anesthesia for Colon Surgery: The Deep Sleep Approach
General anesthesia is key in colon surgery, keeping patients asleep during the operation. It uses medications to induce a deep sleep. This lets surgeons do complex surgeries without pain or discomfort to the patient.
How General Anesthesia Works
General anesthesia works by calming the central nervous system. This makes the patient unconscious and unable to feel pain. It uses a mix of intravenous medications and inhaled anesthetics.
Medications Used During General Anesthesia
The drugs used include propofol, etomidate, and sevoflurane. These are chosen based on the patient’s health, age, and surgery type.
Monitoring During General Anesthesia
During general anesthesia, anesthesiologists watch the patient’s vital signs and anesthesia level. This includes:
Vital Signs Tracking
They keep an eye on heart rate, blood pressure, oxygen levels, and breathing rate. This ensures the patient’s safety.
Depth of Anesthesia Monitoring
They use special tools to check how deep the patient is asleep. This helps keep the patient asleep and pain-free.
Anesthesiologists manage general anesthesia carefully. This makes sure patients have a safe and successful colon surgery experience.
Regional Anesthesia Options: Epidural and Spinal Techniques
Epidural and spinal anesthesia are key for managing pain in colorectal surgery. They offer effective pain relief. These methods can be used alone or together, depending on the patient’s needs.
Epidural Anesthesia for Colorectal Procedures
Epidural anesthesia injects medication around the spinal cord. It’s great for epidural colorectal surgery because it relieves pain well. The epidural catheter can also give more pain medicine after surgery.
Spinal Anesthesia Applications
Spinal anesthesia injects medication into the spinal fluid. It’s often used for spinal anesthesia colorectal surgery because it works fast. It’s best for surgeries below the belly button.
Combined Spinal-Epidural Approaches
The combined spinal-epidural (CSE) method uses the best of both worlds. It starts working fast like spinal anesthesia and keeps working like epidural anesthesia. This is great for regional anesthesia in colorectal surgery, giving full pain relief.
Benefits for Pain Management
Regional anesthesia methods, like epidural and spinal, are very helpful for pain. They cut down on the need for strong opioids. This means fewer side effects and a better recovery.
Limitations and Considerations
While regional anesthesia is very effective, there are some things to think about. These include when it might not be safe, like with bleeding problems or if the patient doesn’t want it. Also, it needs skilled anesthesiologists to do it right.
| Anesthesia Technique | Benefits | Limitations |
| Epidural Anesthesia | Effective post-operative pain relief, flexibility with epidural catheter | Potential for epidural failure, risk of epidural hematoma |
| Spinal Anesthesia | Rapid onset, effective pain relief | Limited duration, potentially for spinal headache |
| Combined Spinal-Epidural | Combines benefits of both techniques, flexible pain management | Increased complexity, potentially for increased risk of complications |
The Anesthesia Process for Colorectal Surgery
Anesthesia is key in colorectal surgery, making sure patients are comfortable and safe. It has many stages, each important for a successful surgery.
Pre-operative Evaluation
First, a detailed check-up is done before surgery. This looks at the patient’s health history and current status. The anesthesiologist then creates a special anesthesia plan for them.
Induction of Anesthesia
The first step in anesthesia is the induction. Here, the patient gets medicine to make them sleepy or numb, depending on the anesthesia type.
Maintenance During Surgery
After the induction, the anesthesiologist keeps a close eye on the patient. They adjust the anesthesia as needed to keep the patient safe and comfortable during surgery.
Emergence from Anesthesia
When the surgery is over, the anesthesiologist slowly reverses the anesthesia. This helps the patient wake up smoothly and comfortably.
| Stage | Description | Key Considerations |
| Pre-operative Evaluation | Assessment of patient’s medical history and current health | Personalized anesthesia plan development |
| Induction of Anesthesia | Administration of anesthetic medications | Type of anesthesia, patient response |
| Maintenance During Surgery | Continuous monitoring and adjustment of anesthesia | Vital sign management, optimal surgical conditions |
| Emergence from Anesthesia | Reversal of anesthesia effects | Smooth recovery, pain management |
The Role of the Anesthesiologist in Colorectal Surgery
The anesthesiologist is key to a successful colorectal surgery. They make sure the patient is comfortable and pain-free during the procedure.
Pre-surgical Assessment and Planning
Before surgery, the anesthesiologist checks the patient’s health history and current status. They also look at any medications that might affect the anesthesia. This helps them choose the best anesthesia plan.
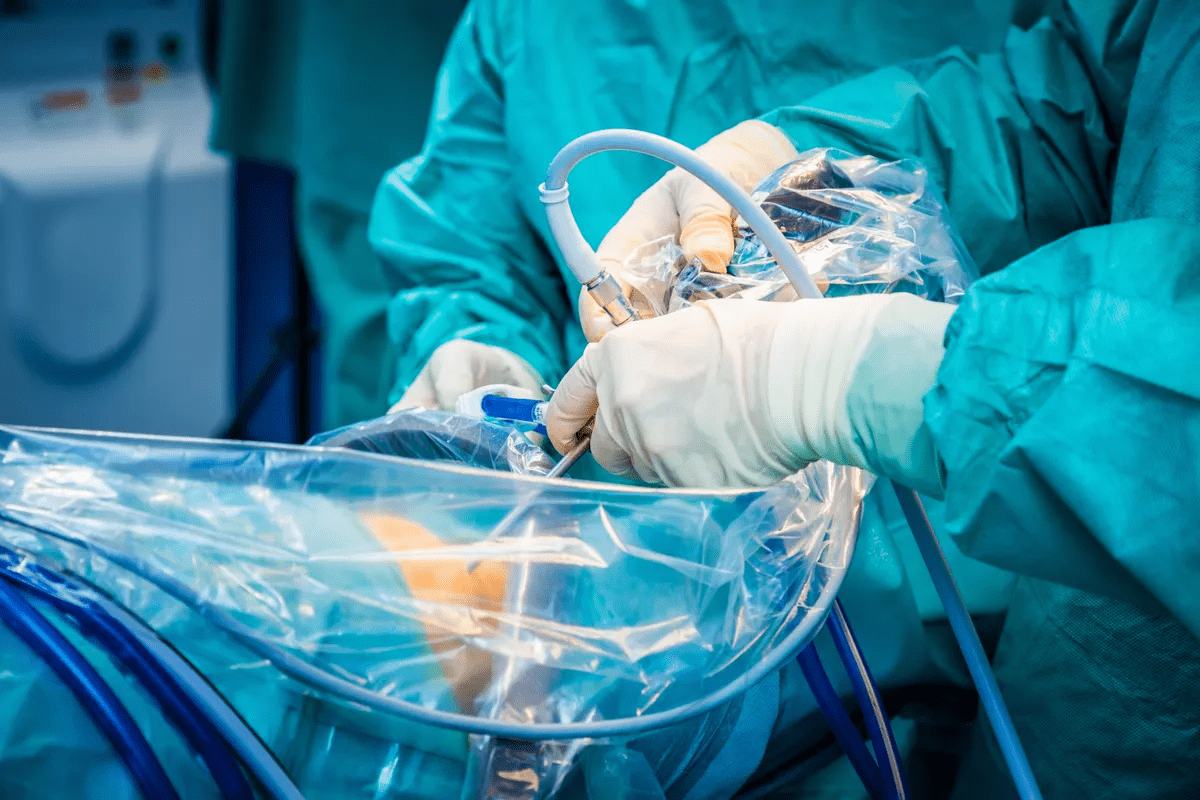
Intraoperative Management
During surgery, the anesthesiologist gives and watches the anesthesia. They keep an eye on the patient’s vital signs. They adjust the anesthesia as needed to keep the patient comfortable and safe.
Post-operative Care Coordination
After surgery, the anesthesiologist helps the patient recover from the anesthesia. They manage any pain or side effects. They work with other healthcare teams to make sure the patient has a smooth recovery.
The role of the anesthesiologist is not just in the operating room. It also includes pre-operative and post-operative care. Good anesthesia care is essential for a good surgical experience.
| Role | Description |
| Pre-surgical Assessment | Evaluating patient’s medical history and health status |
| Intraoperative Management | Administering and monitoring anesthesia during surgery |
| Post-operative Care | Managing recovery and post-operative pain |
Are You Awake During Colorectal Surgery? Patient Experience Explained
The level of consciousness during colorectal surgery depends on the anesthesia type. Patients often worry about being awake or asleep. Knowing about anesthesia can ease these worries.
Level of Consciousness with Different Anesthesia Types
Patients may get general, regional, or local anesthesia for colorectal surgery. General anesthesia makes patients completely unconscious. On the other hand, regional anesthesia, like epidural or spinal, numbs a part of the body. This lets patients stay awake or lightly sedated.
What Patients May Experience or Remember
Under general anesthesia, patients are not awake and don’t remember the surgery. With regional or local anesthesia, patients might be aware but won’t feel pain in the surgical area.
Addressing Concerns About Awareness During Surgery
Some patients worry about being aware during surgery. Awareness is rare but can happen. It depends on:
- The type and dosage of anesthesia used
- The patient’s health and medical history
- The surgery’s complexity and length
Incidence of Awareness
Awareness during general anesthesia is rare, happening in less than 1% of cases.
Prevention Strategies
To lower awareness risk, anesthesiologists use monitoring like bispectral index (BIS) monitoring. They adjust anesthesia levels as needed.
Pain Management Strategies in Colorectal Surgery
Advanced pain management is key to better outcomes after colorectal surgery. It makes patients more comfortable and helps prevent complications. It also speeds up recovery.
Multimodal Analgesia Approaches
Multimodal analgesia combines different pain relief methods. This way, patients need lower doses of each medication. It reduces side effects and improves pain control.
Common parts of this approach include acetaminophen, NSAIDs, and opioids. They work together to give full pain relief.
Post-operative Pain Control Methods
After colorectal surgery, managing pain is vital. Techniques like epidural analgesia and patient-controlled analgesia (PCA) let patients manage their pain. These methods lower pain scores and boost patient happiness.
Enhanced Recovery After Surgery (ERAS) Protocols
ERAS protocols are guidelines for better perioperative care. They aim to reduce stress, improve pain management, and enhance recovery. Key parts include preoperative counseling, optimized nutrition, and standardized pain and anesthetic plans.
Using ERAS protocols can greatly improve patient outcomes. It also shortens hospital stays.
Risks and Complications of Anesthesia Colorectal Surgery
Anesthesia for colorectal surgery is usually safe. But, there are risks and complications to know about. It’s important to understand these to make good choices about your care.
Common Side Effects
Side effects of anesthesia include nausea, vomiting, sore throat, and confusion. These usually go away by themselves.
Nausea and Vomiting
Nausea and vomiting are common. Antiemetic medications help to reduce these symptoms.
Sore Throat and Confusion
A sore throat can happen from the breathing tube used in surgery. Elderly patients might also experience confusion or memory problems.
Serious Complications
Though rare, serious issues can happen. These include allergic reactions, breathing problems, and heart issues. The anesthesia team closely watches to lower these risks.
Risk Factors for Anesthesia Complications
Some factors can raise the risk of complications. These include pre-existing health conditions, age, and smoking. Knowing these helps prepare and manage better.
Recovery from Anesthesia After Colorectal Surgery
Recovering from anesthesia after colorectal surgery is key. It’s a time when patients need close watch. The goal is to keep them safe and comfortable as they wake up and get over the anesthesia.
Immediate Post-Anesthesia Care
Right after surgery, doctors keep a close eye on patients in the recovery room. They check vital signs and overall health. This is important to spot and handle any quick problems or side effects from the anesthesia.
Timeline for Anesthesia Clearance
How long it takes to get clear of anesthesia varies. But usually, most people start to feel better a few hours after surgery.
Managing Post-Anesthesia Side Effects
It’s important to manage side effects after anesthesia. This helps patients feel better and more comfortable.
Short-term Management
At first, doctors might give medication for pain, nausea, or other discomforts. They also watch for side effects like breathing problems or allergic reactions.
Long-term Considerations
While most people get over anesthesia quickly, some might take longer. It’s important to follow up to deal with any ongoing issues or problems.
| Aspect of Care | Immediate Post-Anesthesia | Short-term Recovery |
| Monitoring | Vital signs and overall condition | Pain and side effect management |
| Interventions | Oxygen therapy, pain management | Medication for nausea, pain |
| Care Focus | Safety and comfort | Comfort and recovery |
Special Considerations for Anesthesia in Colorectal Surgery
Administering anesthesia for colorectal surgery is not a simple task. Different patients and situations need special care to ensure safe and effective anesthesia.
Elderly Patients
Elderly patients face unique challenges during colorectal surgery. Their age and health issues require careful preoperative assessment. This helps identify risks and prepare them for surgery.
Patients with Comorbidities
Those with heart disease or diabetes need meticulous anesthesia planning. Choosing the right anesthetic agents and monitoring closely during surgery is key to reducing risks.
Emergency Colorectal Surgery
Emergency surgeries, like those for bowel obstruction or perforation, are tough for anesthesia. Rapid sequence induction and aggressive fluid resuscitation might be needed.
Anesthesia Challenges
Emergency cases often have less time for preoperative evaluation and optimization.
Modified Approaches
Anesthesiologists might use special techniques, like regional anesthesia or adjust anesthetic doses.
| Patient Group | Anesthesia Considerations | Key Strategies |
| Elderly Patients | Age-related physiological changes, comorbidities | Careful preoperative assessment, tailored anesthetic agent selection |
| Patients with Comorbidities | Presence of significant comorbid conditions | Meticulous anesthesia planning, close intraoperative monitoring |
| Emergency Surgery Patients | Urgent need for surgery, limited preoperative evaluation | Rapid sequence induction, aggressive fluid management |
Understanding these special considerations helps healthcare providers manage anesthesia risks better. This improves patient outcomes in colorectal surgery.
Conclusion: Making Informed Decisions About Anesthesia for Colorectal Surgery
It’s important to know about the different types of anesthesia for colorectal surgery. Patients need to understand the options like general, regional, and local anesthesia. This helps them choose the best one for their needs.
Anesthesia is key to making sure patients are comfortable and safe during surgery. Talking to the anesthesiologist about medical history, concerns, and preferences is important. This way, patients can make the best decisions for their care.
Good communication between patients and healthcare providers is critical for a good outcome. Patients who know about anesthesia options can handle their surgery better.
To make good choices about anesthesia for colorectal surgery, patients need to understand the options and their effects. Working with their healthcare team ensures a safe and successful surgery.
FAQ
Are you asleep during colorectal surgery?
Yes, most patients are under general anesthesia. This means they are asleep and don’t feel pain during the surgery.
What type of anesthesia is used for colorectal surgery?
General anesthesia is often used for colorectal surgery. Sometimes, regional anesthesia like epidural or spinal is used too.
Is colorectal surgery painful?
The surgery itself isn’t painful because of the anesthesia. But, patients might feel pain after the surgery. This pain is managed with pain control and ERAS protocols.
What are the risks associated with anesthesia in colorectal surgery?
Anesthesia can cause side effects like nausea, vomiting, and dizziness. Though rare, serious complications can happen. These are more likely in people with health issues or older adults.
How long does it take to recover from anesthesia after colorectal surgery?
Recovery time from anesthesia varies. Most patients stay in the PACU for a while before moving to a hospital room.
Can elderly patients undergo colorectal surgery with anesthesia?
Yes, elderly patients can have surgery with anesthesia. Doctors take extra steps to manage health issues and adjust anesthesia plans.
What is the role of the anesthesiologist in colorectal surgery?
Anesthesiologists are key in pre-surgery checks, managing during surgery, and post-surgery care. They ensure patient safety and comfort.
Are there different anesthesia options for colon surgery?
Yes, there are different options like general, regional, and local anesthesia. The choice depends on the surgery, patient health, and the surgeon’s preference.
Can patients with comorbidities undergo colorectal surgery with anesthesia?
Yes, patients with health issues can have surgery with anesthesia. But, careful planning and evaluation are needed to reduce risks.
What is Enhanced Recovery After Surgery (ERAS) protocol?
ERAS is a care approach that aims to reduce stress and promote recovery after surgery. It helps minimize complications.
How is pain managed during and after colorectal surgery?
Pain is managed with anesthesia during surgery and pain medications after. Other methods are also used to help with pain.
Is it possible to be aware during colorectal surgery?
Awareness during surgery is rare. Anesthesiologists closely monitor anesthesia levels to prevent this.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339719/



































