A recent study on post-surgical mortality among Medicare enrollees found some surgeries are much riskier than others. Procedures like femur fracture reduction, hip arthroplasty, and coronary artery bypass grafting have high mortality rates.Find out which procedures are known as the lowest survival surgery and what factors influence patient outcomes.
It’s important to know the risks of these complex surgeries. Both patients and doctors need to understand this. The surgery’s complexity and the patient’s health condition greatly affect the outcome.
Key Takeaways
- Certain surgeries have significantly higher mortality rates.
- Femur fracture reduction and hip arthroplasty are among the surgeries with high mortality rates.
- Coronary artery bypass grafting is another complex procedure with a high risk.
- Patient’s health condition and surgery complexity are key factors in survival rates.
- Understanding these risks is key for making informed decisions.
Understanding Surgical Mortality: Key Factors That Determine Survival
Surgical mortality is complex, influenced by patient and procedure factors. Knowing these is key for patients and doctors to make smart surgery choices.
Patient-Related Risk Factors
Patient factors greatly affect surgical mortality. These include age, comorbidities, and health status. Older patients or those with health issues face higher risks.
Procedure-Related Risk Factors
The surgery’s complexity and the surgeon’s experience are key. More complex surgeries, like those involving many organs, are riskier.
How Surgical Mortality Is Measured and Reported
Mortality rates are tracked by hospitals and registries. This data shows the risks of various surgeries.
| Risk Factor | Description | Impact on Mortality |
| Age | Older patients are at higher risk | Higher mortality rates |
| Comorbidities | Presence of underlying health conditions | Increased risk of complications |
| Surgical Complexity | More complex surgeries carry higher risks | Higher mortality rates for complex procedures |
Cardiac Surgeries with the Lowest Survival Rates
Some cardiac surgeries have lower survival rates because they are very complex. These surgeries are lifesaving but carry big risks. Both surgeons and patients must think carefully about these risks.
Heart Transplantation: 30-Day and 5-Year Survival Statistics
Heart transplantation is a very complex surgery with a high mortality rate. About 15% of patients don’t make it past the first year. The 30-day survival rate shows the immediate risks and the patient’s health.
The 5-year survival rate shows how well the transplant lasts and the patient’s health over time.
Survival statistics for heart transplantation:
- 1-year survival rate: around 85%
- 5-year survival rate: approximately 69%
Complex Aortic Dissection Repair and Mortality Rates
Repairing a complex aortic dissection is a high-risk surgery. The mortality rate is high because of the surgery’s complexity and the patient’s critical condition. Emergency repairs are riskier than planned surgeries.
The challenges of aortic dissection repair include:
- Managing the dissection and preventing further complications
- Addressing associated conditions such as aneurysms or organ malperfusion
Multiple Valve Replacement Surgery Outcomes
Replacing multiple valves is a complex procedure with higher risks than single valve replacement. The outcomes depend on the patient’s condition, the valves involved, and the surgical method.
Risk Factors Specific to Valve Surgeries
Risk factors for valve surgeries include:
- Patient-related factors such as age, comorbidities, and cardiac function
- Surgery-related factors, including the type of valve replaced and the surgical approach
Knowing these risk factors is key to improving patient outcomes and making informed surgery decisions.
Neurosurgical Procedures with High Mortality
Neurosurgical procedures are very complex and risky. This is because the brain is delicate. These surgeries are in critical areas, so there’s little room for error.
The risk in neurosurgery is shown in its mortality rates. For example, removing brain tumors in key areas is very risky. Survival chances depend on the tumor’s location and the patient’s health.
Brain Tumor Resection in Critical Areas: Survival Statistics
Survival rates for brain tumor removal depend on several factors. These include the tumor’s location, size, and the patient’s health before surgery. “The location of the tumor is a critical determinant of surgical outcome,” experts say.
Cerebral Aneurysm Clipping: Risk vs. Benefit
Cerebral aneurysm clipping is also a high-risk procedure. It’s a choice between the risks of surgery and the risk of the aneurysm rupturing. Research shows that while clipping can work, it comes with a big risk of complications.
Traumatic Brain Injury Surgery: Factors Affecting Outcomes
Outcomes for traumatic brain injury surgery depend on several things. These include the injury’s severity, the patient’s age, and if there are other injuries. Predicting outcomes can be hard, making it important to make informed decisions.
A renowned neurosurgeon, noted, “Improving neurosurgery outcomes depends on choosing the right patients and being very precise in surgery.” This highlights the need for expertise in these complex surgeries.
Gastrointestinal Surgeries and Their Survival Rates
Complex surgeries in the gastrointestinal system, like the Whipple procedure, are key for treating cancers. But they have high death rates. These surgeries are for patients with serious conditions, making survival rates very important.
Pancreaticoduodenectomy (Whipple Procedure): Why It’s High-Risk
The Whipple procedure removes parts of the pancreas, duodenum, gallbladder, and sometimes stomach. It’s mainly for pancreatic cancer. The surgery’s complexity and patient health make it risky.
Survival statistics for the Whipple procedure show 30-day mortality rates from 2% to 5% in top centers. But, long-term survival depends on the cancer type and patient health.
Esophagectomy for Esophageal Cancer: Mortality Factors
Esophagectomy removes part or all of the esophagus for esophageal cancer. It’s a complex surgery with risks like infection and breathing problems.
The mortality rates for esophagectomy vary, with 30-day mortality from 2% to 10%. Long-term survival depends on cancer stage and surgery success.
Total Gastrectomy for Advanced Stomach Cancer: Survival Statistics
Total gastrectomy removes the whole stomach for advanced stomach cancer. It’s a complex surgery with possible complications.
The survival statistics for total gastrectomy depend on cancer stage and patient health. Five-year survival rates can be 20% to 50% or more, based on disease extent and surgery success.
Transplant Surgeries: Risk Assessment and Outcomes
Transplant surgeries are a key treatment for serious illnesses. But, they carry big risks. Success depends on the patient’s health and the surgery’s complexity.
Liver Transplantation Mortality Rates by Condition
Liver transplants save lives for those with severe liver disease. Mortality rates differ based on the patient’s condition. For example, those with acute liver failure face higher risks than those with chronic disease.
Lung Transplantation: Short and Long-Term Survival
Lung transplants help those with severe lung diseases. Thanks to better surgery and care, short-term survival has improved. But, long-term survival is harder due to rejection and infections.
Multi-Organ Transplant Procedures and Their Challenges
Multi-organ transplants are very complex. They involve transplanting several organs at once, like liver and kidney or heart and lung. This complexity raises the risk of problems and affects survival chances.
| Transplant Type | 1-Year Survival Rate | 5-Year Survival Rate |
| Liver Transplant | 85% | 70% |
| Lung Transplant | 80% | 50% |
| Multi-Organ Transplant | 75% | 60% |
Transplant surgery outcomes depend on many factors. These include the patient’s health, any existing conditions, and the surgeon’s experience. Knowing these factors helps understand the risks and benefits of transplant surgeries.
Thoracic Surgeries with Poor Prognosis
Some thoracic surgeries have a poor prognosis due to various risks. Procedures like pneumonectomy for lung cancer and extrapleural pneumonectomy for mesothelioma are complex. They carry significant risks.
Pneumonectomy for Advanced Lung Cancer: Survival Rates
Pneumonectomy removes a lung for advanced lung cancer. Survival rates depend on cancer stage and patient health. Studies show a 5-year survival rate of 20% to 50%.
Extrapleural Pneumonectomy for Mesothelioma: Risk-Benefit Analysis
Extrapleural pneumonectomy treats mesothelioma, a rare lung lining cancer. It removes the lung, diaphragm, and pericardium parts. Though it offers survival chances, it’s risky.
Complex Thoracoabdominal Aortic Aneurysm Repair Outcomes
Repairing thoracoabdominal aortic aneurysms is a high-risk surgery. It involves fixing aorta aneurysms from chest to abdomen. The surgery is complex and risky, with high mortality and complication rates.
| Surgery Type | 5-Year Survival Rate | Major Complications |
| Pneumonectomy for Lung Cancer | 20-50% | Respiratory failure, infection |
| Extrapleural Pneumonectomy for Mesothelioma | 10-30% | Mortality, cardiac complications |
| Thoracoabdominal Aortic Aneurysm Repair | 50-70% | Paraplegia, renal failure |
It’s important to understand the risks and outcomes of these surgeries. This helps surgeons and patients make informed decisions. By looking at survival rates and complications, healthcare can guide patients better.
Emergency Surgeries with the Lowest Survival Surgery Rates
Emergency surgeries are very urgent and often have tough outcomes. These surgeries, like fixing a ruptured aortic aneurysm and treating massive trauma, have high death rates. This is because the conditions are severe and the patients are in critical states.
Ruptured Abdominal Aortic Aneurysm Repair: Mortality Statistics
Ruptured abdominal aortic aneurysm (AAA) repair is a critical emergency surgery with significant mortality rates. Studies show that the death rate for this surgery can be between 40% and over 80%. This depends on the patient’s age, health problems, and how quickly they get surgery.
Improving survival rates depends on quick diagnosis and fast surgery. Endovascular repair is a new method that might save more lives. It’s better for some patients than traditional open repair.
Emergency Surgery for Massive Trauma: Predictors of Survival
Emergency surgery for massive trauma also has low survival rates. Survival depends on the injury’s severity, the patient’s health, and the quality of care they get.
- Trauma severity scores are key in predicting outcomes.
- The presence of co-morbid conditions can make surgery harder.
- Prompt care is essential for better survival chances.
Surgery for Septic Shock and Multiple Organ Failure: When Is It Too Late?
Surgery for septic shock and multiple organ failure has poor outcomes. Deciding to operate is tough. It depends on the sepsis cause, organ failure extent, and the patient’s condition.
In septic shock, surgical intervention might be needed to find and treat the infection source. But, death rates are high, even more so with multiple organ failure.
It’s important for surgeons and patients to understand these surgeries and their outcomes. This shows the need for informed decision-making and timely intervention to boost survival chances.
Age and Comorbidity Impact on High-Risk Surgeries
It’s key to understand how age, health issues, and surgery risks are linked. With more older people getting surgery, knowing the effects of age and health on surgery results is vital.
Elderly Patients: Age-Related Surgical Risk Factors
Older patients face unique challenges in surgery. Age-related decline in physiological reserve can slow down recovery. Frailty and sarcopenia also raise the risk of complications after surgery.
For elderly patients with many health issues, a detailed check-up before surgery is needed. This helps spot risks and find ways to reduce them.
Impact of Diabetes, Heart Disease, and Respiratory Conditions
Health issues like diabetes, heart disease, and chronic respiratory diseases affect surgery results. Diabetes can slow down healing and raise infection risk. Heart disease may cause heart problems during surgery.
Respiratory issues, like COPD, make anesthesia and care after surgery harder. This increases the chance of breathing problems.
Obesity and Immunocompromised States: Special Considerations
Obesity and weakened immune systems add extra hurdles in surgery. Obesity makes surgery harder and raises the risk of infections and breathing issues.
Patients with weakened immune systems are more likely to get infections after surgery. They need special care before, during, and after surgery to lower these risks.
Informed Consent and Decision-Making for High-Risk Procedures
Informed consent is key for high-risk surgeries. These surgeries have big risks and unsure outcomes. It’s a deep talk between the patient, their family, and the doctor about the surgery’s risks and benefits.
Understanding and Communicating Surgical Risk
Talking about surgical risks is vital. It’s about the chance of problems, how it might affect life quality, and survival chances. Clear and compassionate communication helps patients and families make choices that fit their values.
Quality of Life Considerations vs. Survival
When thinking about risky surgeries, weighing benefits against risks is important. It’s about the patient’s health, values, and future hopes. Quality of life considerations are just as key as survival chances in making a decision.
| Factors | Quality of Life Considerations | Survival Benefits |
| Patient’s Health Status | Current functional status and comorbidities | Likelihood of survival post-surgery |
| Personal Values | Patient’s priorities regarding quality of life | Patient’s willingness to undergo risky procedures |
| Expectations | Expected improvement or decline in quality of life | Expected survival period and its quality |
When to Consider Alternative Treatments
At times, treatments other than surgery might be better. This choice should be made after talking with doctors. Alternative treatments like palliative care or medication can improve life quality without surgery risks.
The choice to have a risky surgery should be well-informed. By focusing on informed consent and patient-centered care, doctors help patients make the best decisions for themselves.
Improving Outcomes in High-Risk Surgeries
To improve outcomes in high-risk surgeries, we need to understand what affects surgical success. We must also stick to evidence-based practices. This approach helps increase patient survival rates and improves care quality.
Preoperative Optimization Strategies That Save Lives
Preoperative optimization is key to lowering surgical risks. It involves checking the patient’s health, including managing chronic conditions like diabetes and high blood pressure. Improving nutrition and lowering risk factors can greatly affect surgery results. A study found that preoperative care is vital for better postoperative outcomes.
“Preoperative care has a significant impact on postoperative outcomes, and optimization of the patient’s condition before surgery is critical.”
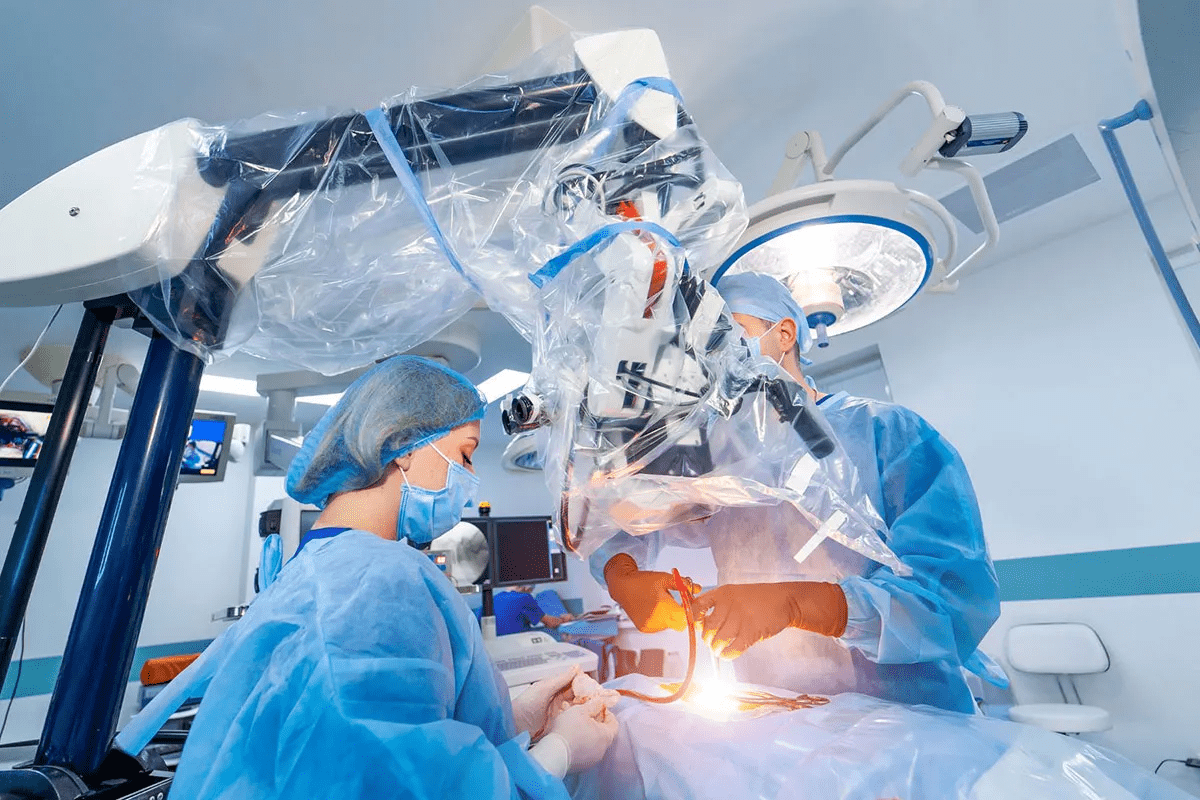
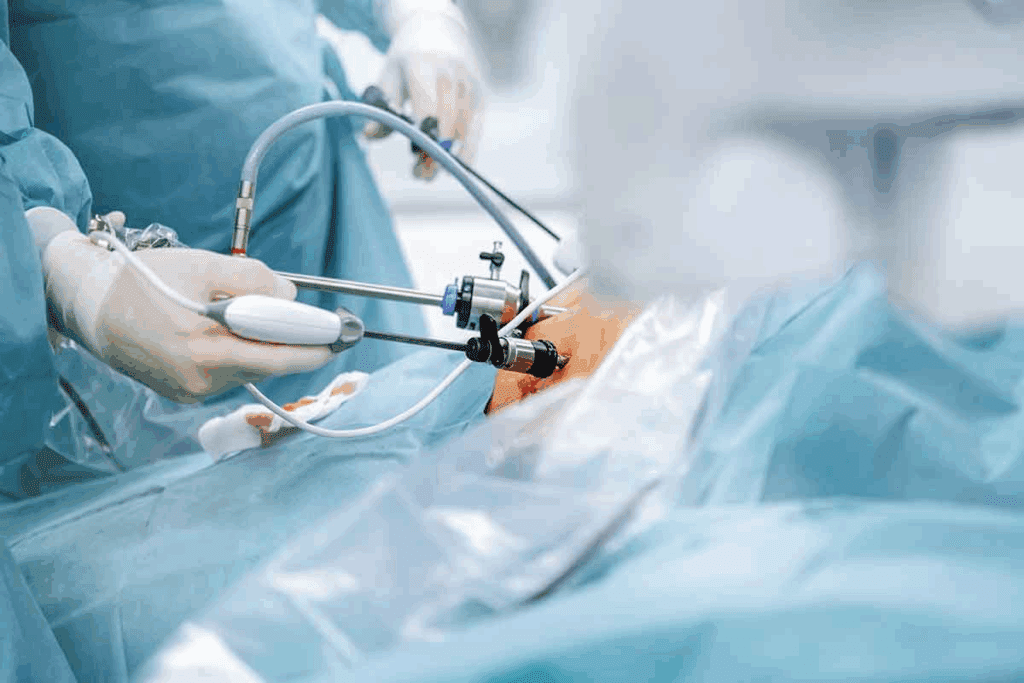
Advances in Surgical Techniques and Technology
New surgical techniques and technology have changed surgery. Minimally invasive and robotic-assisted surgery improve precision and cut recovery times. Better imaging technologies help surgeons plan and perform complex surgeries.
Postoperative Care Improvements and Their Impact
Postoperative care is essential for recovery. Enhanced Recovery After Surgery (ERAS) protocols have been shown to lower complications and speed up recovery. ERAS focuses on early movement, nutrition, and pain control.
Enhanced Recovery After Surgery (ERAS) Protocols
ERAS protocols have proven to improve outcomes in many surgeries. They include:
- Preoperative counseling and education
- Optimized pain management
- Early mobilization and nutrition
- Standardized care pathways
By using these strategies, healthcare providers can greatly improve patient results and lower surgery risks.
Conclusion: Balancing Surgical Risks and Benefits
It’s key for patients and doctors to know the risks and benefits of high-risk surgeries. Surgeries with low survival rates, like some heart, brain, and stomach surgeries, need careful thought. Decisions should be made with all the facts.
Patients need to understand the risks and benefits to choose wisely. By weighing these and looking at other treatment options, people can handle tough medical choices. The survival rates for risky surgeries depend on the patient’s health, the surgeon’s skill, and aftercare.
Choosing to have a risky surgery should be a well-thought-out decision. It’s best to talk it over with doctors, considering the possible outcomes and recovery chances. This way, patients can make choices that fit their health and personal needs.
FAQ
What are the surgeries with the worst survival rates?
The surgeries with the worst survival rates include heart transplants and brain tumor removals. Also, surgeries like the Whipple procedure and liver and lung transplants are risky.
What factors contribute to the high mortality rates of certain surgeries?
High mortality rates are due to patient and procedure risks. Patient risks include age and health conditions. Procedure risks include surgery complexity.
How does age impact surgical outcomes?
Older patients face higher risks. This is because of physical decline, health conditions, and less ability to recover.
What is the impact of comorbidities on surgical survival rates?
Conditions like diabetes and obesity can greatly affect survival rates. They increase the risk of complications and death.
What are some of the most complex cardiac surgeries with low survival rates?
Heart transplants and complex aortic repairs have low survival rates. So does multiple valve replacement surgery.
How do neurosurgical procedures like brain tumor resection affect survival rates?
Brain tumor surgeries are risky due to brain complexity. The tumor’s location also plays a role in survival rates.
What are the survival rates for gastrointestinal surgeries like the Whipple procedure?
The Whipple procedure has high mortality rates. This is because of its complexity and the patients’ health.
How do transplant surgeries like liver and lung transplants impact survival rates?
Liver and lung transplants are risky. Survival depends on the patient’s condition and the surgery’s complexity.
What role does informed consent play in high-risk surgeries?
Informed consent is key. It involves explaining risks and benefits clearly to patients and their families. It also considers other treatment options.
How can outcomes be improved in high-risk surgeries?
Improving outcomes requires a team effort. This includes better preparation before surgery, new surgical techniques, and enhanced care after surgery.
What is the significance of ERAS protocols in surgical recovery?
ERAS protocols help improve recovery and reduce complications. They are very effective in surgical care.
What are some emergency surgeries with low survival rates?
Emergency surgeries like aortic aneurysm repair and trauma surgery have low survival rates. They are urgent and severe.
How do complex aortic aneurysm repairs affect survival rates?
Complex aortic repairs are risky. They have poor outcomes due to their complexity and the patients’ health.
What are the survival rates for thoracic surgeries like pneumonectomy?
Pneumonectomy has poor outcomes. It’s complex and often for serious conditions like lung cancer.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41598-023-43790-8