Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that nearly 1.5 million people have surgical procedures on their colon and rectum each year in the U.S.? The success of these surgeries, like those for colorectal conditions, depends a lot on how the patient is positioned. The right position is key for the surgeon’s work and the patient’s safety. Learn about the colorectal surgery position patients are placed in for optimal surgical access and safety.
The position chosen depends on many things. This includes the surgery type, the patient’s body, and the surgeon’s choice. Knowing about different positions is important for the best results.
Key Takeaways
- Optimal patient positioning is key for surgery success.
- The position chosen depends on the surgery type, patient anatomy, and surgeon preference.
- Proper positioning improves surgical access and patient safety.
- Understanding different positions is vital for the best surgical outcomes.
- Patient positioning varies a lot across different surgeries.
The Fundamentals of Colorectal Surgery
The success of colorectal surgery depends on knowing surgical techniques and how to position patients. This surgery includes many procedures like resections and repairs. Each one needs the right patient position to work well and avoid problems.
Common Colorectal Procedures
In colorectal surgery, you’ll find procedures like colon resections and rectal repairs. These surgeries need specific patient positions to get the best view.
| Procedure | Common Position |
| Colon Resection | Supine or Lithotomy |
| Rectal Repair | Lithotomy or Prone |
Why Positioning Matters
Getting the patient’s position right is key for surgical exposure and anesthesia administration. It also helps avoid complications. The lithotomy position is best for pelvic area access. The supine position is for abdominal surgeries. The prone position is used for some rectal procedures.
Colorectal Surgery Position: An Overview
Choosing the right position for a patient during colorectal surgery is key. It affects both the surgery and how well the patient recovers. The position depends on the surgery type, the patient’s body, and the surgeon’s choice.
Anatomical Considerations
When deciding on a surgical position for colorectal surgery, anatomy matters a lot. The position must give good access to the area being operated on. It also needs to avoid nerve damage and other problems. For example, surgeries on the rectum might need a different setup than those on the colon.
Impact on Surgical Outcomes
The patient placement colorectal surgery greatly affects the surgery’s success. The right position can lower the chance of complications and make the surgery safer. On the other hand, a bad position can cause nerve injuries, heart issues, and breathing problems. So, picking the right colorectal operation position is very important.
Lithotomy Position in Colorectal Surgery
In colorectal surgery, the lithotomy position is key for reaching the pelvic area. It’s great for surgeries needing exact access to the rectum and nearby areas.
Proper Setup and Technique
Setting up the lithotomy position right is vital. Leg placement and support are critical to avoid nerve damage and other issues. Surgeons and staff must make sure the patient’s legs are in stirrups and their lower back is supported.
Ideal Procedures for Lithotomy Position
The lithotomy position is perfect for many colorectal surgeries, like rectal resections and repairs. It gives the best view and access to the area, making complex surgeries easier. It’s also good for surgeries needing to reach the pelvic area and other parts of the body at the same time.
| Procedure | Benefits of Lithotomy Position |
| Rectal Resection | Optimal access to the rectum, facilitating precise dissection and removal of diseased tissue. |
| Rectal Repair | Enhanced visualization of the rectal area, allowing for more accurate repair of damaged tissues. |
Potential Complications and Preventions
Though the lithotomy position has many benefits, it can also lead to problems. Nerve injuries and pressure points are major concerns. To avoid these, surgical teams must ensure the patient’s legs and lower back are well-padded and supported. Regular checks during the surgery can also help prevent issues.
Supine Position for Colorectal Procedures
The supine position is often chosen for colorectal surgeries because of its benefits. In this position, the patient lies on their back. It’s flexible and works well for many surgeries.
When to Use Supine Positioning
The supine position is common in colorectal surgery. It’s used for surgeries that don’t need to reach the pelvic area. It’s also good for the abdominal region, like the colon.
Indications for Supine Positioning:
- Surgeries involving the colon
- Procedures not requiring pelvic access
- Operations where abdominal access is necessary
Surgical experts say the supine position is great for the abdominal cavity. It’s perfect for many colorectal surgeries.
“The supine position is advantageous for its simplicity and the ease with which anesthesia can be administered and patient monitoring can be performed.”
Advantages and Limitations
The supine position is easy for anesthesia and monitoring. But, it might not work for all surgeries, like those needing pelvic access.
| Advantages | Limitations |
| Ease of anesthesia administration | Limited access to pelvic area |
| Simplified patient monitoring | Potential for nerve injuries if not properly positioned |
| Excellent access to abdominal cavity | May not be ideal for procedures requiring steep Trendelenburg position |
In conclusion, the supine position is key in colorectal surgery. It has many benefits but also some drawbacks. Knowing when and how to use it is vital for success.
Prone Position in Colorectal Surgery
For some colorectal procedures, the patient must be positioned prone. This is key for surgeries needing access to the back of the rectum and other parts of the pelvis.
Indications for Prone Positioning
The prone position is best for certain rectal surgeries and repairs. It gives surgeons a clear view of the area they need to work on. It’s also good for surgeries of the back of the pelvis.
Setup Techniques and Considerations
Setting up a patient in the prone position needs careful planning. It’s important to use the right padding and support to avoid injuries. The team must work together to get the position right, using special equipment when needed.
Managing Complications in Prone Position
Dealing with problems in the prone position can be tough. It’s important to watch the patient closely for any breathing or heart issues. The team must be ready to make changes to keep the patient safe during the surgery.
Trendelenburg Position Applications
For many colorectal operations, positioning the patient in Trendelenburg is a standard practice. It enhances surgical exposure. The Trendelenburg position involves tilting the patient so their feet are higher than their head. This can significantly improve access to the pelvic area.
Benefits for Pelvic Access
The primary benefit of using the Trendelenburg position in colorectal surgery is the improved access it provides to the pelvic organs. This is very important in procedures that involve the rectum and lower parts of the colon. By tilting the patient, surgeons can more easily visualize and manipulate the tissues in this complex anatomical region.
The benefits of Trendelenburg positioning for pelvic access include:
- Enhanced Visualization: The tilted position allows for better visualization of the pelvic structures.
- Increased Accessibility: Surgeons can more easily access the pelvic organs, facilitating complex procedures.
- Improved Surgical Precision: With better access and visualization, surgeons can perform procedures with greater precision.
Physiological Effects and Precautions
While the Trendelenburg position offers significant benefits for pelvic access, it also has physiological effects that need to be carefully managed. These include changes in blood pressure, respiratory function, and possible nerve injuries due to prolonged positioning.
To mitigate these risks, surgical teams should:
- Carefully monitor the patient’s vital signs throughout the procedure.
- Use appropriate supportive devices to prevent nerve injuries and pressure points.
- Adjust the patient’s position as needed to maintain optimal physiological stability.
By understanding both the benefits and the possible risks of the Trendelenburg position, colorectal surgeons can optimize its use. This helps improve surgical outcomes.
Lateral Positions for Specific Colorectal Procedures
In colorectal surgery, the lateral position is used for certain procedures. It allows surgeons to access the sides of the abdominal cavity. This is important for operations that need precise access.
The choice of right or left lateral positioning depends on the surgery’s location. For right colon procedures, a right lateral position is often used. Left-sided colon or rectal surgeries prefer a left lateral position.
Right vs. Left Lateral Positioning
Knowing the difference between right and left lateral positioning is key. Right lateral positioning is best for right colon or hepatic flexure surgeries. On the other hand, left lateral positioning is better for left colon, splenic flexure, or rectum surgeries.
Optimal Procedures for Lateral Positions
Lateral positions are great for colon resections and repairs. They allow surgeons to access the colon from the side. This makes complex procedures easier.
Surgeons must think about the patient’s anatomy and the procedure’s needs. This helps them position the patient correctly for a successful surgery.
Position-Related Complications and Prevention
Complications from patient position can greatly affect outcomes in colorectal surgery. It’s key to avoid nerve injuries, pressure sores, and heart issues by using the right patient position.
Nerve Injuries and Pressure Points
Nerve injuries are a big worry in colorectal surgery because of the long time patients stay in one position. The ulnar nerve is at high risk, mainly when the elbow is bent. To lower this risk, it’s important to support the patient’s arms well and avoid putting pressure on the ulnar nerve.
Managing pressure points is also critical. Using pressure-relieving devices can spread out the patient’s weight, reducing sore risk. Changing the patient’s position during long surgeries can also help avoid pressure on sensitive spots.
| Nerve | Common Injury Causes | Prevention Strategies |
| Ulnar Nerve | Elbow flexion, direct pressure | Proper arm support, minimize elbow flexion |
| Brachial Plexus | Arm abduction, shoulder brace pressure | Careful arm positioning, avoid excessive abduction |
| Peroneal Nerve | Pressure on the fibular head | Padding around the fibular head |
Cardiovascular and Respiratory Considerations
The way a patient is positioned during surgery can affect their heart and breathing. For example, the Trendelenburg position can raise venous pressure and might harm breathing by pushing the diaphragm up. Surgeons need to adjust the patient’s position to keep their heart and lungs working well.
Keeping an eye on hemodynamic parameters and adjusting the surgery as needed can help avoid these problems. Also, managing fluids and using the right breathing strategies can help keep the heart stable during surgery.
| Position | Cardiovascular Effects | Respiratory Effects |
| Trendelenburg | Increased venous pressure | Reduced lung capacity |
| Lithotomy | Potential for hypotension | Minimal direct effect |
| Prone | Variable effects on venous return | Potential for respiratory compromise |
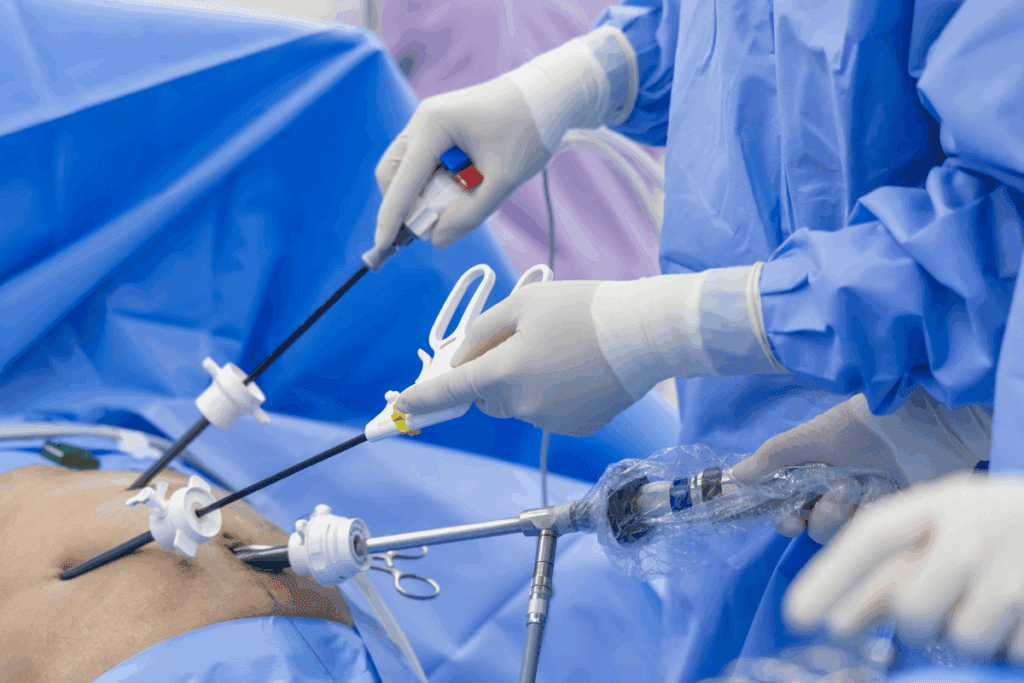
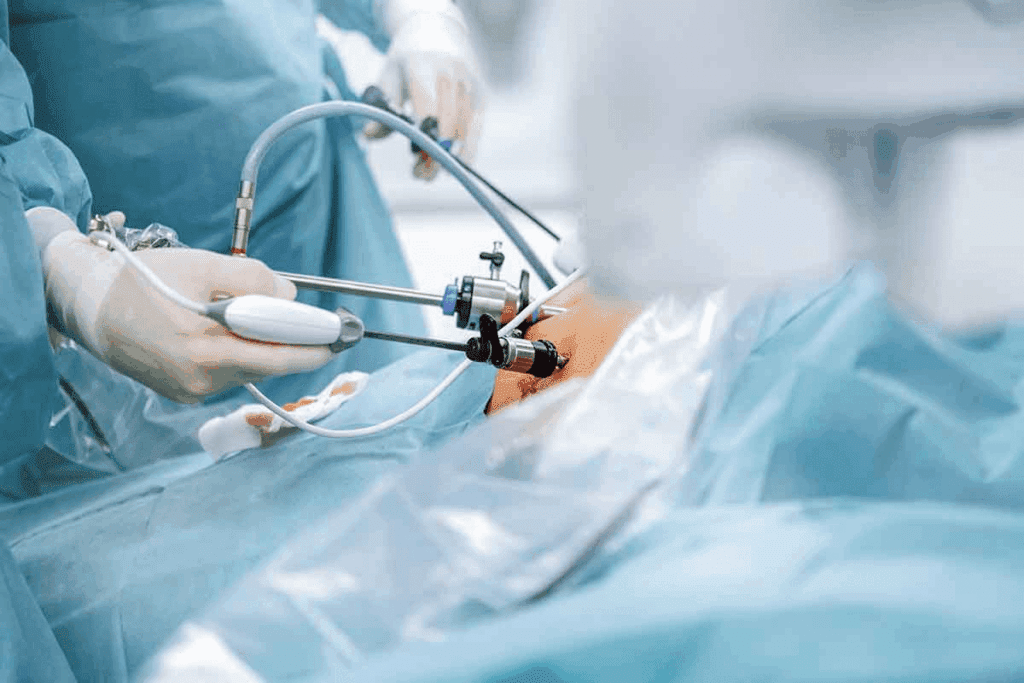
Positioning for Robotic and Laparoscopic Colorectal Surgery
In colorectal surgery, robotic and laparoscopic methods need special patient positioning. This ensures the best results. It’s important to know how to position patients right for these advanced surgeries.
Specialized Requirements for Robotic Systems
Robotic systems need exact patient positioning. This lets the robotic arms dock properly and gives the surgeon the best view. Proper positioning cuts down on risks and makes the surgery smoother. For example, Trendelenburg positioning is key in some robotic surgeries for better pelvic access.
Position Adjustments for Minimally Invasive Approaches
Laparoscopic colorectal surgery also needs careful patient positioning. This ensures the surgical team can easily see and work in the abdominal cavity. Adjusting the patient’s position helps in getting the best view and control of laparoscopic tools. Lateral positioning, for instance, is useful in some surgeries for better colon access.
Rectal vs. Colon Surgery: Position Differences
Rectal and colon surgeries are both part of colorectal surgery. But they need different ways to position patients. This is because of where the surgery is and what it’s for.
Optimizing Access to the Rectum
For rectal surgery, getting the patient in the right position is key. The lithotomy position is often used. It lets surgeons easily reach the rectum.
This position is great for things like fixing rectal prolapse. Sometimes, the prone position is better for the back part of the rectum. It helps surgeons see and work on the area better.
Positioning for Various Colon Segments
Colon surgery needs a position that helps reach the right part of the colon. For the sigmoid colon or descending colon, a right lateral position works well. The ascending colon or cecum might need a left lateral position.
| Colon Segment | Preferred Position | Surgical Access |
| Sigmoid/Descending Colon | Right Lateral | Improved visualization of the sigmoid and descending colon |
| Ascending Colon/Cecum | Left Lateral | Enhanced access to the right-sided colon |
| Transverse Colon | Supine or Modified Lithotomy | Flexibility for complex procedures |
The position chosen depends on the surgery type, like open, laparoscopic, or robotic. Knowing these details helps make surgery better for everyone involved.
Specialized Equipment for Optimal Positioning
Advanced surgical tables and positioning aids are key for the best patient positioning in colorectal surgery. These tools offer the support and flexibility needed for complex surgeries.
Surgical Tables and Attachments
Surgical tables for colorectal surgery are highly adjustable. This lets the surgical team position patients precisely. Modern tables have attachments like stirrups and leg rests. These are vital for procedures like lithotomy positioning.
| Feature | Description | Benefit |
| Adjustable Height | Allows for easy patient positioning | Reduces strain on surgical team |
| Trendelenburg Tilt | Facilitates pelvic access | Improves surgical visibility |
| Lateral Tilt | Enables optimal access to colon segments | Enhances surgical precision |
Positioning Aids and Protective Devices
Positioning aids and protective devices are also vital for patient safety and comfort in colorectal surgery. They include protective padding to prevent pressure injuries and straps to keep the patient secure.
Using these devices improves patient safety. It also lets the surgical team concentrate on the surgery without worrying about positioning.
Conclusion
Proper patient positioning is key for successful colorectal surgery. It affects how easy the surgery is, keeps the patient safe, and improves results. Knowing the different colorectal surgery positions is vital for surgeons and healthcare teams.
The right surgical position for colorectal surgery depends on the surgery type, the patient’s body, and avoiding problems. To position patients well, surgeons need to know the patient’s body, the surgery method, and possible risks.
Choosing the right colorectal surgery position helps surgeons do complex surgeries better. It lowers the chance of problems and makes patients do better. As surgery methods and tools get better, precise patient positioning will keep being important.
FAQ
What are the most common positions used in colorectal surgery?
In colorectal surgery, the most common positions are lithotomy, supine, and prone. Each has its own use and considerations.
How does patient positioning impact surgical outcomes in colorectal surgery?
Patient positioning greatly affects surgical outcomes. It ensures the best access and reduces risks, leading to better results.
What are the benefits and risks of using the lithotomy position in colorectal surgery?
The lithotomy position is often used for rectal surgeries. It’s important to place legs carefully to avoid nerve damage.
When is the supine position used in colorectal surgery?
The supine position is used for surgeries not needing pelvic access. It’s easier for anesthesia and monitoring.
What are the indications for using the prone position in colorectal surgery?
The prone position is used for certain surgeries like rectal repairs. It requires careful setup for safety and access.
How does the Trendelenburg position enhance access to the pelvic organs?
The Trendelenburg position helps access the pelvic organs. It offers better exposure but needs careful management of physiological effects.
What are the possible complications from patient positioning in colorectal surgery?
Complications from positioning include nerve injuries, pressure sores, and heart issues. Preventive measures are key to avoid these.
How does robotic and laparoscopic colorectal surgery impact patient positioning?
Robotic and laparoscopic surgeries need specific positioning for the equipment. Understanding these needs is vital for success.
What are the differences in patient positioning for rectal and colon surgery?
Rectal and colon surgeries need different positions. This is based on the procedure and location, for better access.
What role do surgical tables and positioning aids play in achieving optimal patient positioning?
Surgical tables and aids are key for optimal positioning. They ensure safety, comfort, and access during surgery.
How can nerve injuries and pressure points be prevented during colorectal surgery?
Knowing the risks of nerve injuries and pressure points is important. Preventive measures are essential for patient safety during surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513320/