Every year, millions of Americans visit the emergency room for immediate medical care. A big part of them need special attention. Trauma surgery is a special field for life-threatening injuries. It often needs surgery right away ER vs trauma surgery.
The difference between emergency room services and trauma surgery is key. It affects the care patients get. Both are vital in emergencies but serve different needs and require different skills.
Key Takeaways
- Trauma surgery is a specialized field that handles life-threatening injuries.
- Emergency rooms provide immediate care for a wide range of medical conditions.
- The level of care and expertise differs significantly between emergency room services and trauma surgery.
Understanding Emergency Medicine and Trauma Surgery
It’s important to know the difference between emergency medicine and trauma surgery. These two fields are closely related but have their own roles in healthcare.
Defining Emergency Medicine
Emergency medicine deals with urgent medical situations. ER doctors work in emergency rooms. They handle cases like heart attacks, strokes, and severe injuries.
Key aspects of emergency medicine include:
- Rapid assessment and decision-making
- Management of acute illnesses and injuries
- Coordination with other healthcare specialists
Defining Trauma Surgery
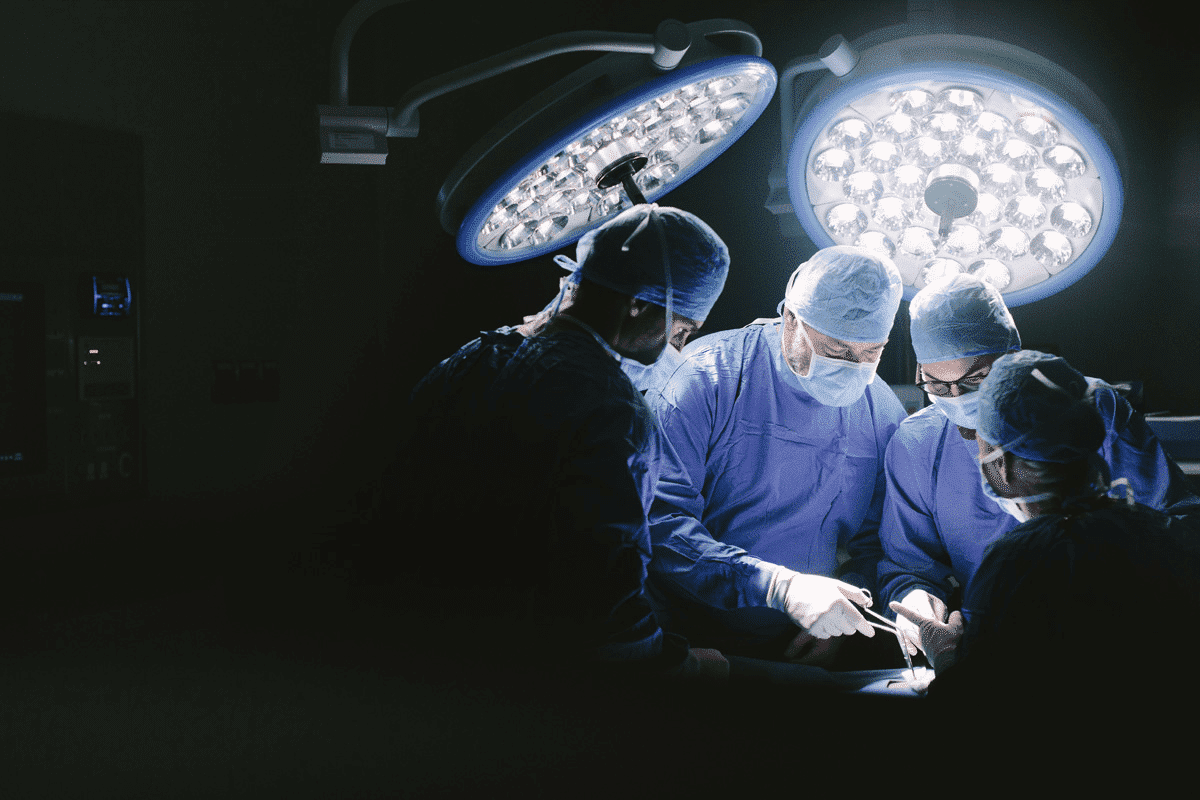
Trauma surgery focuses on treating injuries from accidents or violence. Trauma surgeons perform surgeries for complex injuries. They work with a team to care for trauma patients.
Trauma surgery involves:
- Surgical repair of injuries
- Management of trauma patients in critical care settings
- Collaboration with multidisciplinary teams
Let’s look at how emergency medicine and trauma surgery are different and similar:
Aspect | Emergency Medicine | Trauma Surgery |
Primary Focus | Acute medical conditions | Surgical treatment of injuries |
Work Environment | Emergency departments | Trauma centers, operating rooms |
Key Skills | Rapid assessment, broad medical knowledge | Surgical expertise, trauma care |
ER vs Trauma Surgery: Core Differences
ER and trauma surgery are key parts of healthcare but serve different needs. It’s important to know how they differ to appreciate their unique challenges.
Scope of Practice
ER doctors and trauma surgeons have different roles. ER doctors handle many emergencies, from serious illnesses to minor injuries. They focus on first aid and managing patients.
Trauma surgeons, by contrast, deal with severe injuries. They perform complex surgeries in urgent situations.
“Trauma surgeons are the unsung heroes of the medical world, requiring not only surgical skill but also the ability to make rapid decisions in life-threatening situations.”
Medical Expert, Trauma Surgeon
Here’s a table comparing their roles:
Aspect | ER Physicians | Trauma Surgeons |
Primary Focus | Emergency medical care for a wide range of conditions | Surgical interventions for critically injured patients |
Skill Set | Initial assessment, stabilization, and management | Complex surgical procedures, critical care |
Patient Population
ERs and trauma surgery teams see different patients. ERs handle a wide range of cases, from minor issues to emergencies.
Trauma surgeons focus on patients with severe injuries. These injuries often come from accidents or violence. They need quick and complex surgeries.
Key differences in patient population include:
- Condition severity: Trauma surgery patients are generally more critically injured.
- Urgency of care: Trauma surgery often requires immediate intervention.
- Complexity of care: Trauma surgery involves more complex surgical procedures.
Knowing these differences helps in providing better healthcare. It ensures patients get the right care.
Educational Pathways and Training Requirements
Becoming an ER doctor or trauma surgeon takes a lot of hard work and dedication. You need a strong base in medical sciences. This journey is filled with tough education and training.
Emergency Medicine Training
Emergency medicine training prepares doctors for urgent medical situations. It starts with a four-year college degree and four years of medical school. This earns you an MD or DO degree.
Then, you must do a three to four-year residency in emergency medicine. Here, you learn to diagnose and treat many medical issues in emergency rooms.
Key parts of emergency medicine training include learning emergency procedures and managing trauma. You also develop critical thinking skills. You’ll learn about different areas of emergency medicine, like pediatric and sports medicine.
Trauma Surgery Training
Trauma surgery training is more focused and requires a solid understanding of surgery. After medical school, you’ll do a five to seven-year general surgery residency. Some also get extra training through fellowships in trauma surgery or surgical critical care.
Trauma surgery training focuses on the technical skills needed for trauma surgeries. You’ll learn about damage control surgery, managing severe injuries, and trauma care specifics.
Both ER doctors and trauma surgeons must keep up with new medical knowledge. They need to attend workshops, conferences, and online courses. This helps them stay current in these fast-changing fields.
Work Environment and Hospital Settings
It’s important to know how emergency departments and trauma centers work. They are key parts of a hospital but are very different. They have different ways of organizing, caring for patients, and working.
Emergency Department Structure
The emergency department is always busy. It deals with many medical emergencies. It has different areas for different needs:
- Trauma bays for critical patients
- Examination rooms for less critical cases
- Waiting areas for patients and families
Many people work in the ER. This team includes doctors, nurses, and more. They work around the clock, needing a good plan to move patients quickly.
Trauma Center Organization
Trauma centers handle very serious injuries. They are ranked by how well they can handle these cases. A trauma center has:
- A trauma team led by a trauma surgeon
- Advanced imaging and diagnostic tools
- Operating rooms for big surgeries
- Intensive care units for after surgery
Trauma centers work closely with many teams. They are ready for serious injuries. The team works fast to give the best care.
Key differences between ER and trauma center settings include:
- The level of injury or illness severity
- The scope of medical services provided
- The organizational structure and staffing
In summary, ERs and trauma centers are both critical but serve different needs. Knowing these differences helps everyone in healthcare and patients too.
Types of Medical Conditions Treated
It’s important to know what medical conditions emergency rooms and trauma surgery units treat. This helps us understand their roles.
Emergency rooms and trauma surgery units are key parts of a hospital. But they deal with different health issues.
Common ER Presentations
Emergency rooms see many health problems. Some common ones are:
- Chest pain and heart issues
- Respiratory problems, like asthma
- Severe infections, such as sepsis
- Neurological issues, like strokes
- Stomach problems, like bleeding
These issues need quick help. ER doctors are ready to assess, diagnose, and treat these emergencies.
Typical Trauma Surgery Cases
Trauma surgery deals with injuries needing surgery. Common cases include:
- Injuries from car accidents
- Wounds from guns or knives
- Blunt injuries, like from falls
- Burns needing surgery
- Complex bone and tissue injuries
Trauma surgeons work with a team to fix these serious injuries. They do this in a fast and changing environment.
The difference in what ERs and trauma surgery treat shows the special skills needed for each field.
Surgical Procedures and Techniques
Surgical procedures in emergency and trauma surgery are key to saving lives. They require precision, skill, and deep knowledge. This is because they deal with complex and often life-threatening conditions.
Emergency Surgical Procedures
Emergency surgeries are urgent, like for appendicitis or traumatic injuries. Emergency surgeons must make quick decisions and perform complex tasks under pressure. They use techniques like laparotomy and thoracotomy.
Some common emergency surgeries include:
- Appendectomy for acute appendicitis
- Laparotomy for abdominal trauma
- Thoracotomy for thoracic injuries
Trauma Surgery Techniques
Trauma surgery techniques are for complex injuries. Trauma surgeons must manage hemorrhage, repair tissues, and restore function. They use damage control surgery and vascular repair.
Advanced imaging and tools have improved trauma patient outcomes. Trauma surgeons work with a team for complete care.
Day-to-Day Responsibilities and Workflow
ER physicians and trauma surgeons have unique daily tasks that are key to patient care. Their work is shaped by the urgency and complexity of the cases they handle.
ER Physician Daily Routine
ER physicians deal with a wide range of medical issues in the emergency department. Their day begins with a shift briefing. Here, they review patient charts and discuss ongoing cases with the incoming team.
During their shift, ER physicians evaluate patients, order tests, and create treatment plans. They must quickly decide on the most urgent cases.
“The emergency department is a fast-paced environment that requires physicians to be highly adaptable and responsive to changing circumstances.”
ER physicians also work with nurses, specialists, and surgeons. This ensures patients get the best care possible.
Trauma Surgeon Daily Routine
Trauma surgeons handle surgical interventions for acute injuries. Their day includes preparing for surgeries, reviewing imaging, and consulting with specialists.
Trauma surgeons work with the trauma team, including anesthesiologists and nurses. They must make quick decisions in the operating room.
The workflow of trauma surgeons is highly specialized. It requires a deep understanding of surgical techniques and trauma care.
In summary, ER physicians and trauma surgeons work in high-stress environments. Their daily routines and responsibilities are unique and tailored to their expertise.
The Trauma Team: Roles and Collaboration
In the fast-paced world of trauma care, teamwork is key to saving lives. The trauma team is a group of different healthcare experts. They work together to give quick and effective care to patients who are badly hurt.
Composition of a Trauma Team
A trauma team includes trauma surgeons, emergency medicine physicians, nurses, and other support staff. Each person has a special role:
- Trauma surgeons do surgeries.
- Emergency medicine physicians do the first check-up and help stabilize the patient.
- Nurses help with both surgeries and non-surgeries, giving important support.
ER and Trauma Surgery Coordination
It’s important for the ER and trauma surgery teams to work well together. This means:
- They talk clearly about the patient’s status and needs.
- They make quick decisions to focus on what’s most important.
- They have a clear plan for moving patients from the ER to surgery.
This teamwork makes sure patients get smooth and fast care. This helps improve their chances of getting better in emergency situations.
Trauma Centers vs. Emergency Departments
Trauma centers and emergency departments are two different places for emergency care. They have different levels of care, patient types, and ways of working.
Trauma Center Levels and Capabilities
Trauma centers are ranked from Level I to Level III or IV. Level I trauma centers offer the most advanced care. They have doctors on call 24/7 for complex cases.
Level II trauma centers also provide top-notch care but with fewer specialized services. They can handle most trauma cases and have doctors ready at all times. Level III centers start care and might send patients to higher-level centers if needed.
When Patients Go to ER vs. Trauma Center
Where patients go depends on their injury’s severity. Minor injuries or non-traumatic conditions go to emergency departments. Severe injuries go straight to trauma centers by ambulance or helicopter.
EMS decides who goes to a trauma center. They look at the injury’s severity, vital signs, and if surgery is needed right away.
In short, knowing the difference between trauma centers and emergency departments is key. It helps ensure patients get the right care. Healthcare providers make better decisions about where to send patients based on these differences.
Patient Journey Through ER and Trauma Systems
Understanding ER and trauma care is complex. It involves knowing how patients move through these systems. This journey has many stages and involves different healthcare workers.
Emergency Department Patient Flow
The emergency department (ED) is where patients with urgent needs go first. Efficient patient flow in the ED is key for quick care. The process includes:
- Triage: First check to see who needs help most.
- Registration: Getting patient details.
- Assessment: Doctors and nurses do a full check-up.
- Treatment: Care based on what the doctor finds.
- Disposition: Deciding if the patient needs to stay, go home, or be sent elsewhere.
Good management of patient flow in the ED can cut down wait times. It also makes patients happier and care better.
Trauma Patient Pathway
For those with serious injuries, a special trauma pathway is used. It involves a team working together. The steps are:
- Pre-hospital care: Stabilizing and moving the patient to a trauma center.
- Trauma team activation: The trauma team gets ready for the patient’s arrival.
- Resuscitation: Quick care to stabilize the patient’s vital signs.
- Diagnostic evaluation: Using tools to check for injuries.
- Definitive care: Surgery or other treatments for injuries.
The American College of Surgeons says, “The trauma system is a complex process. It needs a team effort to give the best care to injured patients.”
Knowing these pathways helps healthcare providers give better care. It improves outcomes for patients in ER and trauma settings.
Career Outlook and Compensation
The medical field offers many career paths, including emergency medicine and trauma surgery. Both ER doctors and trauma surgeons are vital in healthcare. They have different career paths and salaries.
Emergency Medicine Career Path
Emergency medicine doctors are always in demand. They work in emergency departments, making quick decisions and treating many conditions. Their job is fast-paced and challenging.
Key aspects of an ER doctor’s career include:
- Varied work environments, from community hospitals to large urban centers
- Opportunities for advancement into leadership or administrative roles
- Flexibility in scheduling, including shifts and on-call duties
ER doctors in the U.S. earn about $350,000 a year. But, their salary can change based on location, experience, and employer.
Trauma Surgery Career Path
Trauma surgeons focus on surgeries for acute injuries. Their career requires intense training and a dedication to critical care.
Notable aspects of a trauma surgeon’s career include:
- High-stakes decision-making in high-pressure situations
- Collaboration with multidisciplinary teams to manage complex cases
- Opportunities for research and innovation in trauma care
Trauma surgeons are among the highest-paid, with salaries over $400,000 in the U.S. Their pay can depend on the trauma center, experience, and extra duties.
Specialty | Median Annual Compensation | Work Environment |
ER Doctors | $350,000 | Emergency Departments, Urgent Care Centers |
Trauma Surgeons | $400,000+ | Trauma Centers, Surgical Units |
In conclusion, ER doctors and trauma surgeons have rewarding careers with good pay. Knowing the details of each specialty helps future medical professionals choose their path wisely.
Evolution of Emergency Medicine and Trauma Surgery
The history of emergency medicine and trauma surgery is complex. It involves historical context, new technologies, and changes in healthcare. These changes have greatly improved how we handle emergencies and trauma cases.
Historical Development
Emergency medicine and trauma surgery started in the early 20th century. World War II was a key time for growth in these fields. The first emergency departments opened in the 1960s, creating a new way to give urgent care.
“The development of trauma systems has been driven by the need to provide timely and effective care to critically injured patients.”
— A past president of the American Association for the Surgery of Trauma
The history of trauma surgery is linked to better surgical techniques and trauma care systems. Advances in critical care have greatly improved trauma patient outcomes.
Period | Emergency Medicine Advancements | Trauma Surgery Advancements |
Early 20th Century | Establishment of first emergency departments | Development of basic surgical techniques for trauma |
Mid-20th Century | Advances in emergency medical services (EMS) | Improvements in trauma care during World War II |
Late 20th Century | Specialization in emergency medicine | Advances in surgical critical care |
Modern Advancements and Future Trends
Today, ER and trauma surgery see big changes thanks to new tech. Robotics and advanced imaging are just the start. Telemedicine has also made it easier to get specialist care, helping patients more.
The future looks bright with more personalized medicine and tech integration. Pre-hospital care will also see big improvements. Artificial intelligence will likely change how we diagnose and treat patients.
- Advancements in surgical techniques and technology
- Increased focus on pre-hospital care and EMS
- Integration of AI and machine learning in diagnostics
As these fields keep growing, they will be shaped by research, new tech, and changing patient needs.
Conclusion
ER and trauma surgery have different focuses. The ER handles a wide range of urgent conditions. Trauma surgery handles severe injuries that need surgery.
Knowing the difference helps patients choose the right care. Trauma surgery needs a team and special places.
Both ER and trauma surgery are key in healthcare. They offer different but important care. Patients can make better choices by understanding these roles.
The choice between ER and trauma surgery depends on the patient’s needs. It’s about getting the right care fast. The right path depends on the injury’s severity.
FAQ
What is the primary difference between ER and trauma surgery?
ER doctors treat many acute medical conditions. Trauma surgeons focus on surgeries for serious injuries.
What kind of training do ER doctors receive compared to trauma surgeons?
ER doctors learn about diagnosing and managing acute illnesses and injuries. Trauma surgeons get more training in surgery, focusing on trauma.
Can ER doctors perform surgical procedures?
ER doctors can do some minor procedures. But they can’t do complex surgeries. Trauma surgeons are trained for that.
What are the typical cases handled by ER and trauma surgery?
ERs see many cases, including minor injuries. Trauma surgery deals with severe, life-threatening injuries.
How do trauma centers differ from emergency departments?
Trauma centers handle severe injuries and have a team of trauma surgeons. ERs provide initial care and stabilize patients before transferring them.
What is the role of a trauma team, and how do they collaborate with ER staff?
A trauma team includes trauma surgeons and nurses. They work with ER staff to care for trauma patients. They take over once the patient’s condition is assessed.
Are trauma surgeons and ER doctors compensated differently?
Yes, trauma surgeons are often paid more. This is because of their specialized training and complex work.
How do patients get directed to either ER or trauma centers?
Patients first go to ERs for acute conditions. Those needing immediate surgery are either treated in ER and then moved or go straight to trauma center.
What are the career paths like for ER doctors versus trauma surgeons?
ER doctors and trauma surgeons have different paths. ER doctors can specialize in various emergency medicine areas. Trauma surgeons focus on surgical disciplines.
How have emergency medicine and trauma surgery evolved over time?
Both fields have grown a lot. Advances include better technology, treatment, and patient care. This includes better pre-hospital care and surgical techniques.
What are some future trends in emergency medicine and trauma surgery?
Future trends include more technology, like telemedicine and AI. There will also be more specialization and a focus on better patient outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558916/























