Last Updated on December 4, 2025 by Bilal Hasdemir
Every year, millions of people in the United States face severe injuries. Trauma surgery is key in saving their lives trauma surgery definition.
Trauma surgery fixes or removes damaged tissues and organs. It aims to keep the patient stable and prevent more harm.
Knowing about trauma surgery helps us see its vital role in healthcare.
Key Takeaways
- Trauma surgery is a critical field that provides lifesaving care for severe injuries.
- It involves surgical interventions to repair or remove damaged tissues and organs.
- The goal of trauma surgery is to stabilize the patient’s condition.
- Trauma surgery is a complex and highly specialized field.
- It requires a high level of skill and expertise.
Understanding Trauma Surgery Definition
Understanding trauma surgery means knowing its medical definition and how it differs from other surgeries. It’s a critical area of surgery that deals with serious injuries. These injuries are either life-threatening or could cause significant harm.
Medical Definition of Trauma Surgery
Trauma surgery is about treating injuries from different causes, like blunt or penetrating trauma. It involves emergency surgeries to keep patients stable and treat serious conditions. This definition covers a wide range of surgeries, from initial assessment to final repair.
The main goal of trauma surgery is to save lives and prevent more harm. Trauma surgeons must make quick decisions in stressful situations, often with little information. They need a solid base in general surgery and specialized trauma knowledge.
Key Components | Description |
Emergency Surgical Intervention | Immediate surgical action to address life-threatening injuries. |
Trauma Assessment | Rapid evaluation of the patient’s condition to identify the extent of injuries. |
Resuscitation | Initial treatment to stabilize the patient’s vital signs. |
Distinction from Other Surgical Fields
Trauma surgery stands out because it focuses on emergency care for sudden injuries. Unlike planned surgeries, trauma surgery is urgent and requires quick action. Trauma surgeons handle complex, multi-system injuries in a fast-paced setting.
The main difference between trauma surgery and other specialties is its all-encompassing approach to care. Trauma surgeons work with other healthcare teams to ensure patients get the best care. This includes from the first check-up to rehabilitation.
- Trauma surgery involves immediate surgical intervention for life-threatening injuries.
- It requires a broad skill set, including general surgery and specialized trauma care knowledge.
- Trauma surgeons work as part of a multidisciplinary team to provide complete patient care.
The Evolution of Trauma Surgery
Trauma surgery has a rich history, filled with key moments and groundbreaking research. Over the years, it has changed a lot. This change came from new medical tech, shifts in how doctors work, and the work of leading surgeons.
Historical Development
The history of trauma surgery is filled with important milestones. World War I and II were key times for this field. Surgeons had to get better at treating serious injuries because of these wars.
New tech and trauma centers also helped the field grow. Early trauma surgery techniques were simple and just aimed at keeping patients alive. But as doctors learned more, so did the surgery.
Modern Advancements
Today, trauma surgery keeps getting better, thanks to modern trauma surgery techniques. Surgeons like Michael Rotondo have made big changes. His work on damage control surgery has helped save more lives.
New imaging tech, like CT scans, and smaller surgeries have also made a big difference. These changes have not only made patients healthier but have also opened up new possibilities in trauma surgery.
Types of Trauma Requiring Surgical Intervention
Different types of trauma need different surgical approaches. Trauma surgery is complex, dealing with many injuries. The severity of the trauma decides the surgery needed.
Blunt Trauma
Blunt trauma happens when forces don’t directly enter the body, like in car accidents or falls. It can cause serious internal injuries without visible wounds. Surgical intervention is often required to fix internal bleeding, organ damage, or fractures.
For example, a severe blunt trauma to the abdomen might need an emergency laparotomy. This is to repair or remove damaged organs.
Penetrating Trauma
Penetrating trauma happens when an object pierces the skin and tissues, like from gunshot wounds or stabbings. The injury’s severity and location guide the surgery. Prompt surgical intervention is key to prevent infection and control bleeding.
Surgeons must carefully check the wound’s path to find all damaged areas. This is to ensure all injuries are treated.
Burn Trauma
Burn trauma is caused by heat, cold, electricity, chemicals, or radiation. Severe burns can harm not just the skin but also deeper tissues and organs. Surgery for burn trauma includes removing dead tissue, skin grafting, and reconstructive surgery.
Early surgical intervention can greatly improve recovery. It lowers the risk of infection and aids in healing. Burn care is a team effort, with surgeons and other healthcare professionals working together.
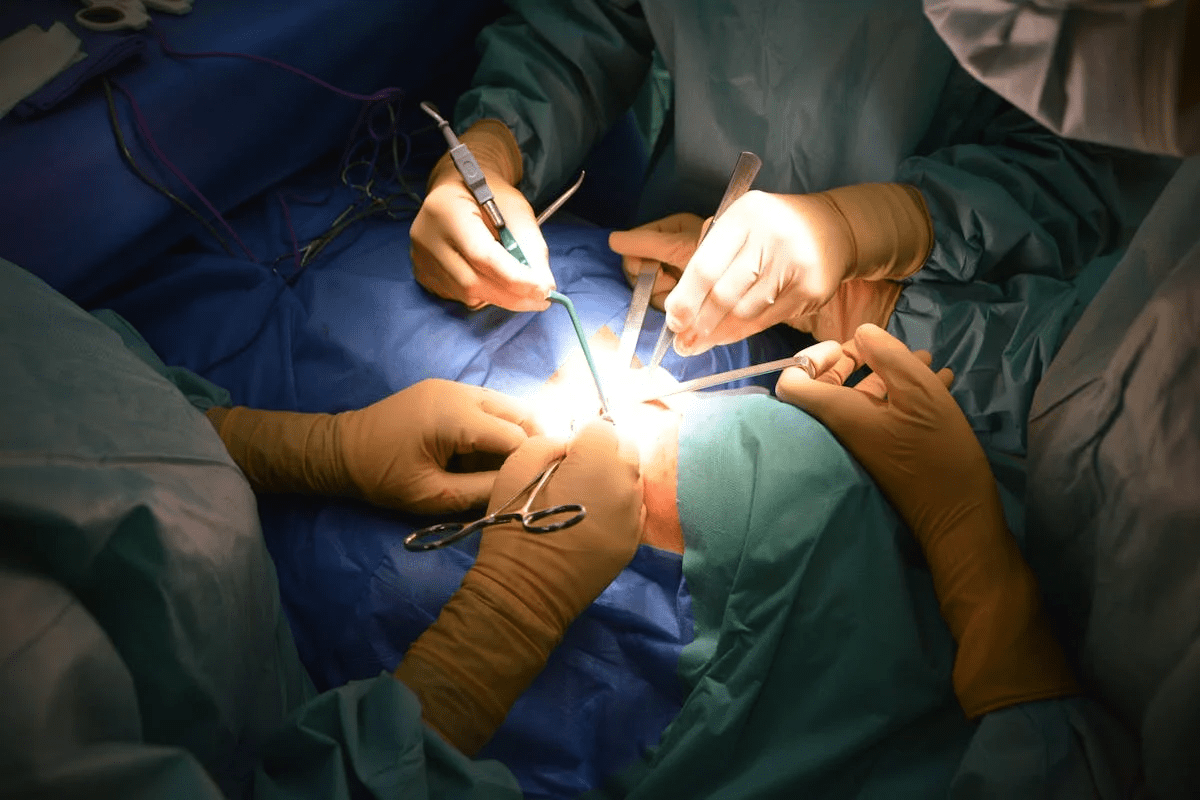
Common Trauma Surgery Procedures
Trauma surgery treats severe injuries. It’s done in emergencies to keep patients stable. This helps prevent further problems.
Abdominal Trauma Surgery
Abdominal trauma surgery fixes injuries inside the belly. It’s needed for blunt or penetrating trauma. This includes damage to vital organs like the liver or spleen.
Surgeons carefully check the injuries. They then fix the damage to keep the patient stable.
Thoracic Trauma Surgery
Thoracic trauma surgery treats chest injuries. This includes damage to the heart, lungs, or major blood vessels. It’s for severe chest trauma.
Surgeons might do a thoracotomy. This is an incision into the chest. They repair or remove damaged tissues and control bleeding.
Orthopedic Trauma Surgery
Orthopedic trauma surgery fixes bone and joint injuries. It’s key for patients to move and function again.
Surgeons use plates, screws, and rods to fix bones. They aim for the best healing and alignment to avoid long-term issues.
Procedure | Description | Key Objectives |
Abdominal Trauma Surgery | Addresses injuries to abdominal organs | Repair damaged organs, control bleeding |
Thoracic Trauma Surgery | Treats injuries to the chest cavity | Repair or remove damaged tissues, restore cardiac and respiratory function |
Orthopedic Trauma Surgery | Treats fractures and musculoskeletal injuries | Stabilize and repair fractured bones, restore mobility |
Emergency Trauma Surgery Protocols
In trauma surgery, emergency protocols are key to patient success. They ensure quick and effective action in emergencies.
Triage and Assessment
Triage sorts patients by how urgent they need care. In trauma surgery, triage and assessment are vital. They quickly check the patient, find serious injuries, and decide how to use resources.
The first check usually follows ATLS (Advanced Trauma Life Support) rules. These rules help assess the patient’s airway, breathing, circulation, disability, and exposure in a systematic way.
Assessment Component | Description | Action |
Airway | Evaluate the patient’s airway for obstruction or compromise. | Secure the airway; intubation if necessary. |
Breathing | Assess the patient’s breathing for adequacy. | Provide oxygen; mechanical ventilation if needed. |
Circulation | Check for signs of shock or circulatory compromise. | Control bleeding; fluid resuscitation. |
Golden Hour Concept
The golden hour is the first hour after an injury. Quick medical help during this time greatly improves patient chances. It’s all about fast assessment and treatment.
Research proves that care in the golden hour leads to better survival rates. So, trauma surgery focuses on quick triage, assessment, and action to improve treatment success.
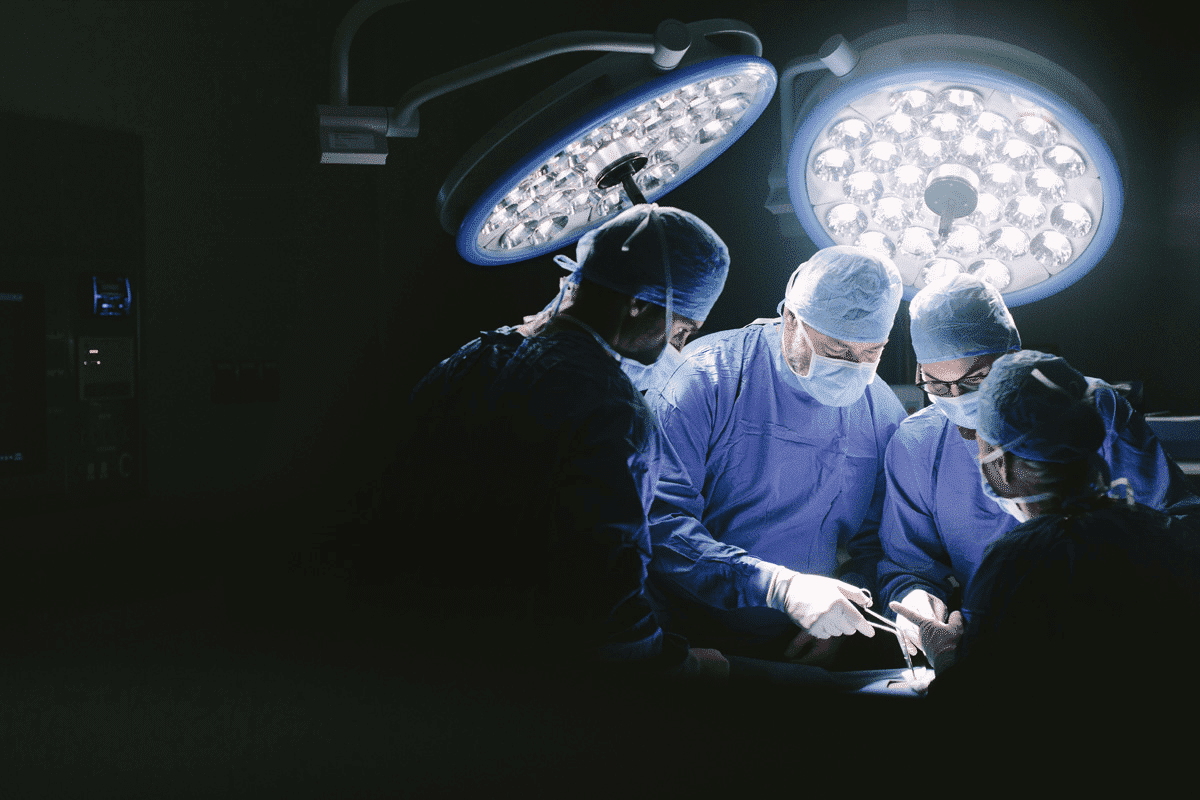
The Trauma Surgeon’s Role and Responsibilities
The role of a trauma surgeon is complex. They need to be skilled in surgery and make quick decisions in stressful situations. These doctors are vital in the healthcare world, giving immediate care to those with severe injuries.
Required Skills and Training
Trauma surgeons go through tough training to get the skills needed. They finish a surgical residency and might get extra training in trauma surgery. This training helps them handle complex injuries and make fast, important decisions.
Some key skills for trauma surgeons are:
- Technical surgical skills
- Decision-making under pressure
- Effective communication
- Leadership abilities
Skill | Description | Importance Level |
Technical Surgical Skills | Proficiency in performing surgical procedures | High |
Decision-making | Ability to make quick and accurate decisions | High |
Communication | Effective communication with the healthcare team | Medium |
Multidisciplinary Collaboration
Trauma care is a team effort. It needs multidisciplinary collaboration among many healthcare workers. Trauma surgeons work with emergency department staff, anesthesiologists, nurses, and other experts to give full care to trauma patients.
This teamwork is key for many reasons:
- It makes sure care is well-coordinated.
- It helps share important information among team members.
- It improves the quality of care for trauma patients.
Good teamwork is what makes trauma care successful. It shows how complex and dynamic treating critical injuries can be.
Trauma Surgery Specialties and Subspecialties
The field of trauma surgery is diverse, with many specialties and subspecialties. These have emerged to handle specific trauma cases. This diversity leads to more focused care and better outcomes for patients with different injuries.
Trauma surgery specialties have grown to meet the needs of various demographics and injuries. Each specialty demands unique skills and knowledge. This allows surgeons to give the best care to their patients.
Pediatric Trauma Surgery
Pediatric trauma surgery focuses on injured children. Children are not just small adults; their bodies and how they react to injury are different. Pediatric trauma surgeons need to be skilled in handling delicate tissues and understanding pediatric trauma care.
Military Trauma Surgery
Military trauma surgery deals with injuries from combat or military operations. Military trauma surgeons are trained for complex, multi-system injuries like blast injuries and high-velocity gunshot wounds. Their expertise is vital in both military and civilian settings, applying principles of damage control surgery and resuscitation.
Critical Care Trauma Surgery
Critical care trauma surgery combines trauma surgery with critical care medicine. Surgeons in this field manage trauma patients’ surgery and post-operative care in intensive care units. Critical care trauma surgeons need to be skilled in managing life-supporting therapies and complications in critically ill patients.
The following table summarizes the key aspects of these trauma surgery specialties:
Specialty | Focus | Key Skills |
Pediatric Trauma Surgery | Surgical care of injured children | Knowledge of pediatric anatomy and physiology, delicate tissue handling |
Military Trauma Surgery | Treatment of combat-related injuries | Management of complex, multi-system injuries, damage control surgery |
Critical Care Trauma Surgery | Surgical management and post-operative care of trauma patients | Life-supporting therapies, management of complications in critically ill patients |
Trauma Systems and Organization of Care
Trauma systems are key in giving structured care to those with severe injuries. They involve many people and need good coordination.
Trauma Team Composition
A trauma team has doctors, nurses, and support staff. The team changes based on the injury’s severity and the patient’s needs.
The team leader is usually a surgeon or experienced doctor. They coordinate the team and make important decisions for the patient.
Trauma Activation Criteria
Criteria for activating a trauma team exist. They look at how the injury happened, the patient’s vital signs, and injury severity.
Good criteria ensure the team is ready quickly. This allows for fast assessment and treatment of the patient.
Criteria | Description | Activation Level |
Mechanism of Injury | Severity of the injury | High |
Vital Signs | Patient’s vital signs | Medium |
Injury Severity | Severity of the patient’s injuries | High |
Transfer Protocols
Protocols for transferring trauma patients are in place. They ensure safe and efficient transfer between facilities. This involves working together between facilities.
Good transfer protocols reduce delays in care. They help ensure patients get the right care.
In summary, a well-organized trauma system is vital for quality care. The team’s makeup, activation criteria, and transfer protocols are all key. They help ensure patients get timely and right medical help.
Life-Saving Trauma Surgery Interventions
Life-saving trauma surgery has changed the game, giving hope to those with severe injuries. These methods are key in treating trauma, cutting down death rates, and bettering patient results. Damage control surgery and resuscitative procedures are at the forefront of this progress.
Damage Control Surgery
Damage control surgery is a new way to handle severe injuries. It starts with quick surgery to stop bleeding and prevent infection. Then, the patient gets time to recover before more surgery.
“The concept of damage control surgery has revolutionized the management of critically injured patients, allowing for a staged approach to their care.”
Michael Rotondo
This method cuts down on deaths and lets doctors tackle complex injuries step by step. It leads to better results for patients.
Resuscitative Procedures
Resuscitative procedures are essential in the first steps of treating trauma patients. They help restore blood flow, manage shock, and keep organs working. The aim is to make the patient stable for more detailed care.
Procedure | Description | Benefits |
Damage Control Surgery | Initial surgery to control bleeding and contamination | Reduces mortality, allows for staged care |
Resuscitative Procedures | Techniques to restore blood volume and manage shock | Stabilizes patient, improves outcomes |
In summary, trauma surgery interventions like damage control and resuscitative procedures are vital. They’ve made a big difference in treating trauma patients. These methods have lowered death rates and improved patient care, marking a big leap forward in trauma treatment.
Patient Experience in Trauma Surgery
Patients going through trauma surgery face many challenges. These start from the first emergency response to the surgery and recovery. How patients feel during this time is very important. It affects their health and the quality of care they get.
Initial Emergency Department Experience
The first time a patient sees the emergency department is key. Efficient triage and rapid assessment are vital. They help patients get the right care quickly. The team in the emergency department works hard to make sure patients are ready for surgery.
Surgical Intervention and Critical Care
Surgery is a big part of trauma care. It needs skill and quick thinking. The surgeon must make fast decisions to help the patient. After surgery, critical care is just as important. It helps the patient recover and deal with any problems.
Aspect of Care | Description | Importance |
Emergency Department Care | Initial assessment and stabilization | High |
Surgical Intervention | Trauma surgery and repair | Critical |
Critical Care | Post-surgical management and recovery | High |
Post-Surgical Recovery Process
Recovering after surgery is hard for patients. It’s not just about getting better physically. Patients also need emotional and mental support. A good recovery plan, including pain management and physical therapy, is key.
Understanding what patients go through helps doctors and nurses improve care. They can find ways to make things better for future patients.
Trauma Surgery Techniques and Innovations
New techniques in trauma surgery are helping patients recover faster. The field is changing with new methods and technologies. These changes are making patients better and healing quicker.
Minimally Invasive Approaches
Minimally invasive surgery (MIS) is key in today’s trauma care. It uses small cuts for big surgeries. This means less damage and faster healing.
MIS cuts down on pain and hospital time. But, it needs skilled surgeons and the right tools.
Technological Advancements
New tech is changing trauma surgery. Things like 3D printing and robotic surgery are making surgeries better. They help doctors work more precisely.
Technology | Application in Trauma Surgery | Benefits |
3D Printing | Creation of patient-specific models and implants | Improved preoperative planning and customized patient care |
Robotic Surgery | Enhanced precision in complex procedures | Reduced risk of complications and improved outcomes |
Advanced Imaging | Better visualization of injuries | More accurate diagnoses and targeted treatments |
New tech is making care better and treating more complex cases. As tech keeps improving, trauma surgery will keep evolving.
Challenges and Ethical Considerations in Trauma Surgery
The field of trauma surgery is filled with challenges. It requires a deep understanding of medical and ethical principles. Trauma surgeons face complex situations that need both technical skill and ethical judgment.
Resource Allocation
One big challenge is managing resources. Trauma centers have to deal with limited resources like operating room time and blood products. It’s important to allocate these resources well to give patients the best care.
End-of-Life Decisions
Trauma surgeons often have to make tough decisions about the end of life. This is when patients have severe injuries with poor chances of recovery. These decisions balance patient autonomy, family expectations, and medical needs.
Psychological Impact on Providers
The psychological toll on trauma surgeons and healthcare providers is significant. The stress of trauma care can cause burnout and mental health issues. It’s vital for institutions to support their staff to prevent these problems.
Challenge | Description | Potential Solution |
Resource Allocation | Managing limited resources for optimal patient care | Implementing efficient resource management protocols |
End-of-Life Decisions | Making difficult decisions for patients with severe injuries | Establishing clear guidelines for end-of-life care |
Psychological Impact | Mitigating the psychological effects on healthcare providers | Providing mental health support and resources |
Conclusion
Trauma surgery is key to saving lives and improving health outcomes. It deals with severe injuries that need a team effort. This includes skilled surgeons, nurses, and other healthcare experts.
The history of trauma surgery shows how it has grown. From old methods to new technologies, it has come a long way. It covers many areas like abdominal, thoracic, and orthopedic surgery, each needing special skills.
The importance of trauma surgery is clear. It needs ongoing improvement to tackle injury challenges. Healthcare providers must know how to triage, assess, and save lives. This ensures top-notch care for those in need.
As trauma surgery advances, focusing on research, education, and training is vital. This ensures that trauma teams can handle complex injuries. It leads to better patient care and highlights trauma surgery’s critical role in healthcare.
FAQ
What is trauma surgery?
Trauma surgery is a field that deals with emergency care for severe injuries. It involves surgeries to fix or remove damaged tissues and organs.
What are the different types of trauma that require surgical intervention?
There are three main types of trauma needing surgery. These are blunt trauma, penetrating trauma, and burn trauma. Each type has its own unique needs and surgical methods.
What is the golden hour concept in trauma surgery?
The golden hour is a critical time right after an injury. Quick medical help during this time is key to saving lives and improving recovery chances.
What are the common procedures used in trauma surgery?
Trauma surgery includes many procedures. These include surgeries for abdominal, thoracic, and orthopedic injuries. Each uses specific techniques to treat different injuries.
What is damage control surgery?
Damage control surgery is a fast approach in trauma care. It aims to stop bleeding and contamination, stabilize the patient, and prevent further harm. It’s often a lifesaving step.
What are the skills and training required to become a trauma surgeon?
To be a trauma surgeon, one needs special training and skills. This includes knowledge in surgery, critical care, and emergency medicine. They must also handle high-pressure situations well.
How is trauma care organized?
Trauma care is organized through a trauma system. This system includes trauma teams, activation criteria, and transfer protocols. It ensures coordinated care for trauma patients.
What are the challenges faced by trauma surgeons?
Trauma surgeons face many challenges. These include managing resources, making end-of-life decisions, and dealing with the emotional toll of their work. They need strong emotional resilience and professional skills.
What are the latest innovations in trauma surgery?
New innovations in trauma surgery include minimally invasive techniques and technology. These aim to improve patient outcomes, reduce complications, and enhance care quality.
What is the role of multidisciplinary collaboration in trauma care?
Multidisciplinary collaboration is vital in trauma care. It involves working together with surgeons, nurses, and other specialists. This teamwork ensures effective and complete care for trauma patients.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30131000/