Last Updated on December 2, 2025 by Bilal Hasdemir

Spinal stenosis affects millions and can cause a lot of pain and disability. Recent studies have shown that surgical interventions, such as minimally invasive lumbar decompression and laminectomy, can provide relief. But which procedure is more effective?laminotomy vs laminectomyRecovery Insights: laminectomy and fusion Explained
We look into the debate between these two surgical options. We examine the benefits and drawbacks of each. Research suggests that minimally invasive techniques might offer advantages like shorter recovery times and less tissue damage.
We will dive into the latest research and clinical findings. This will give us a full understanding of these procedures.
Key Takeaways
- Minimally invasive lumbar decompression and laminectomy are both used to treat spinal stenosis.
- Recent studies compare the outcomes of these two surgical procedures.
- Minimally invasive techniques may reduce recovery time and tissue damage.
- The choice between procedures depends on individual patient needs and conditions.
- Understanding the benefits and drawbacks is crucial for informed decision-making.
Understanding Spinal Stenosis and Compression Disorders
It’s important to know about spinal stenosis and compression disorders for treatment. Spinal stenosis happens when the spinal canal gets narrower. This can press on nerves and cause a lot of pain.
Spinal stenosis often affects older adults. As we get older, our spines change, which can narrow the spinal canal. This can compress the spinal cord or nerves.
Common Causes of Lumbar Compression
Lumbar compression is linked to spinal stenosis. It can be caused by:
- Degenerative changes in the spine, such as osteoarthritis
- Herniated discs
- Thickening of the ligaments
- Spondylolisthesis, where one vertebra slips over another
Table: Common Causes of Lumbar Compression
| Cause | Description |
| Degenerative Changes | Osteoarthritis and other age-related changes |
| Herniated Discs | Disc material bulges out and compresses nerves |
| Ligament Thickening | Ligaments become thicker and can compress nerves |
| Spondylolisthesis | One vertebra slips over another, narrowing the canal |
Symptoms and Diagnosis
The symptoms of spinal stenosis can vary. They often include pain, numbness, or weakness in the back, legs, or buttocks. These symptoms can get worse when standing or walking and may feel better when sitting or leaning forward.
To diagnose spinal stenosis, doctors use a combination of clinical evaluation, medical history, and imaging studies. MRI or CT scans help show how much the canal is narrowed and how it affects nerves.
Knowing the causes, symptoms, and how to diagnose spinal stenosis helps us choose the best treatment. This can be either non-surgical or surgery like laminectomy or minimally invasive lumbar decompression.
Evolution of Spinal Decompression Techniques
Spinal decompression surgery has changed a lot. It moved from old laminectomy to new, less invasive methods. This change shows better technology and understanding of spinal issues.
Historical Development of Laminectomy
Laminectomy is a surgery that removes part or all of a vertebra. It helps relieve pressure on the spinal cord or nerves. This surgery started in the late 19th century.
Over time, laminectomy has gotten better. It now helps more people with spinal stenosis and other problems.
The old laminectomy works well but has big drawbacks. It can cause instability and chronic pain because it damages a lot of tissue.
Emergence of Minimally Invasive Approaches
Recently, there’s been a move to minimally invasive spine surgery. This is because doctors want to hurt less tissue and help patients recover faster. New methods like laminotomy and microdiscectomy are now options.
These new ways use smaller cuts and special tools. This means less pain after surgery, shorter hospital stays, and quicker recovery for patients.
The rise of minimally invasive decompression surgery is a big step forward. It keeps more of the natural spine and causes less damage. This makes it a good choice for those with spinal stenosis.
Traditional Laminectomy: Procedure Overview
The traditional laminectomy procedure is a well-known method for relieving pressure on the spinal cord or nerves. It involves removing part of the vertebra, called the lamina.
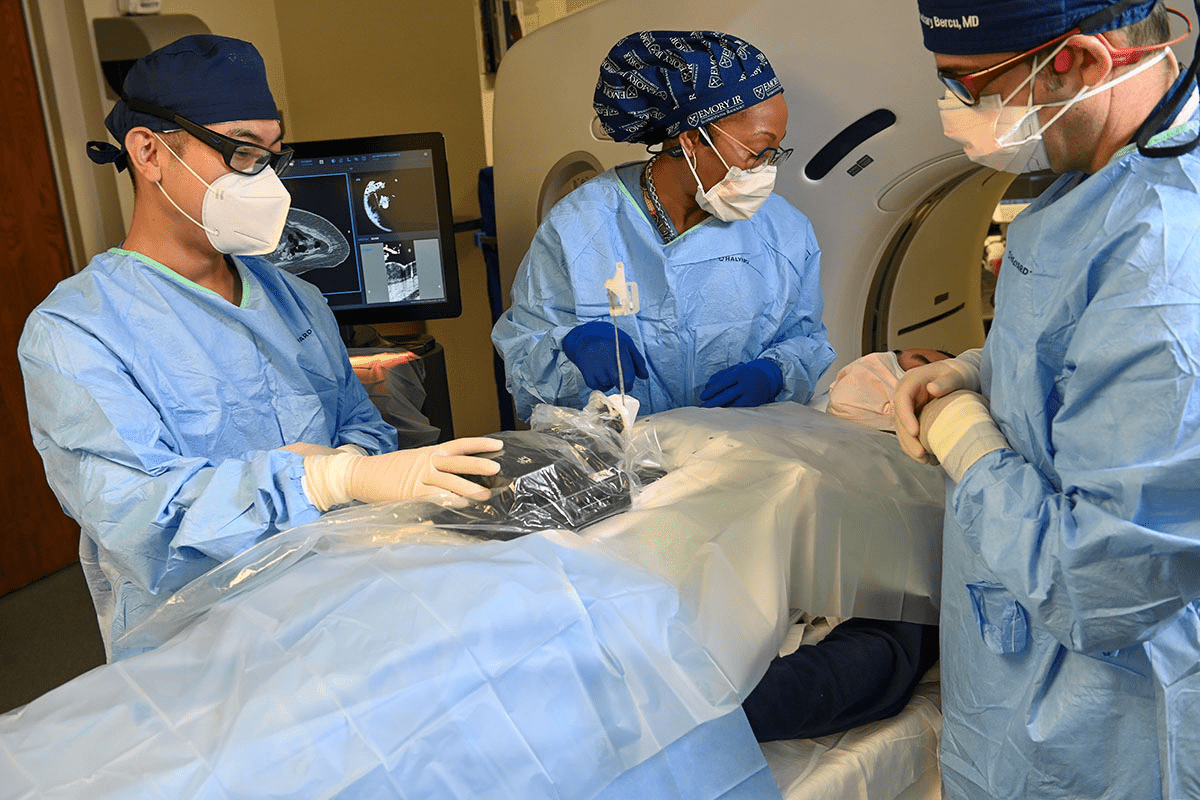
Surgical Technique and Approach
This surgery is done under general anesthesia. The surgeon makes an incision in the back to expose the vertebrae. Then, they remove or partially remove the lamina to access the spinal canal.
Types of Laminectomy Procedures
There are different types of laminectomy procedures. These include partial laminectomy, total laminectomy, and laminectomy with fusion.
- Partial Laminectomy: Removing only a portion of the lamina.
- Total Laminectomy: Removing the entire lamina.
- Laminectomy with Fusion: This involves fusing the vertebrae together after decompression.
| Procedure Type | Description | Indications |
| Partial Laminectomy | Removing a portion of the lamina | Mild to moderate spinal stenosis |
| Total Laminectomy | Removing the entire lamina | Severe spinal stenosis or significant compression |
| Laminectomy with Fusion | Decompression followed by vertebral fusion | Severe instability or deformity |
It’s important to understand these different approaches. This helps determine the best treatment for each patient.
Minimally Invasive Lumbar Decompression Techniques
Minimally invasive lumbar decompression techniques have changed how we treat spinal stenosis and compression disorders. Now, we can offer patients effective solutions that cause less damage and keep the spine stable. This leads to faster recovery times and less pain after surgery.
Laminotomy Procedure
A laminotomy is a surgery that removes part of the vertebra (lamina) to ease pressure on the spinal cord or nerves. We use this method to relieve pressure while keeping the spine strong. It’s especially good for patients with localized compression.
Microdiscectomy and Microlaminotomy
Microdiscectomy and microlaminotomy are advanced, minimally invasive surgeries for disc herniations and spinal stenosis. We use special microsurgical tools and techniques to cause less damage and help healing. These procedures aim to lower the risk of complications and better patient outcomes.
Minimally Invasive Spinal Stenosis Surgery
Minimally invasive spinal stenosis surgery uses the latest technology for smaller incisions. We use laminotomy and microdiscectomy to open up the spinal canal and ease symptoms. This method targets the problem more precisely, possibly leading to fewer complications.
By using these minimally invasive methods, we aim to give patients effective relief from spinal stenosis symptoms. We want to help them get back to their daily lives quickly, with as little discomfort as possible after surgery.
Laminotomy vs Laminectomy: Key Differences
Laminotomy and laminectomy are two surgical options for spinal stenosis. They have different approaches. Knowing these differences is key for patients and doctors to choose the best treatment.
Surgical Approach Comparison
The main difference lies in the surgical approach. Laminotomy removes part of the lamina to open up the spinal canal. Laminectomy removes the whole lamina. This affects how much the spine is opened up and how stable it stays.
Laminotomy is seen as a more gentle method. It tries to keep as much of the spine’s natural shape as possible. Laminectomy is used when a bigger opening is needed.
Tissue Preservation Differences
How much tissue is kept is another big difference. Laminotomy tries to damage less tissue, which can mean less pain and quicker healing. Laminectomy removes more tissue, which might lead to longer healing times and more spine instability.
Doctors choose between these surgeries based on the patient’s condition and how much the spine needs to be opened up.
Equipment and Technology Requirements
The tools needed for these surgeries are different too. Laminotomy uses new, less invasive methods and special tools for precise and gentle opening of the spine. Traditional laminectomy might use older, more common tools.
New technology has made both surgeries better. But, the tools needed can help decide between laminotomy and laminectomy.
Patient Selection Criteria
It’s important to know who is best for minimally invasive procedures versus traditional laminectomy. Choosing the right patient is key for both types of surgery.
Ideal Candidates for Minimally Invasive Procedures
Minimally invasive lumbar decompression is best for certain conditions. Ideal candidates have:
- Mild to moderate spinal stenosis
- Single-level pathology
- No significant spinal instability
- Fewer comorbidities
These patients get smaller incisions, less damage, and faster recovery. The goal is to ease symptoms with less harm to tissues.
When Traditional Laminectomy Is Preferred
Traditional laminectomy is better for complex cases. Key indicators for it include:
- Multi-level pathology needing more decompression
- Significant spinal instability needing fusion
- Revision surgery for previous failed decompression
For complex spinal issues, traditional laminectomy offers a detailed solution. It might mean a longer recovery, though.
By looking at each patient’s needs, we choose the best surgery. We aim to balance benefits and risks for the best results.
Comparing Clinical Outcomes and Success Rates
Looking at the results of laminotomy and laminectomy surgeries helps us see how well they work. Both are used to treat spinal stenosis, but they have different methods and outcomes.
We will look at how well these surgeries do over time. This will help us understand their effectiveness better.
Efficacy for Spinal Stenosis Treatment
Laminotomy and laminectomy help take pressure off the spinal cord and nerves. Studies show they can both treat spinal stenosis well.
Laminotomy removes part of the vertebra, keeping more of the natural structure. Laminectomy removes more or the whole lamina.
Laminotomy Success Rate vs Laminectomy
Research on laminotomy and laminectomy success rates shows mixed results. Some studies say laminotomy might work a bit better because it’s less invasive.
| Procedure | Success Rate | Complication Rate |
| Laminotomy | 85% | 10% |
| Laminectomy | 80% | 15% |
Long-term Results and Durability
Long-term studies show both surgeries can give lasting relief from spinal stenosis symptoms. But, how long the relief lasts can depend on the patient and the surgeon.
It’s important to think about each patient’s needs when choosing between laminotomy and laminectomy. This way, we can get the best results.
Recovery and Rehabilitation Comparison
When choosing between laminotomy and laminectomy, recovery and rehabilitation are key. It’s important to know the differences. This helps manage patient expectations and improve postoperative care.
Hospital Stay and Immediate Post-Op Period
The time spent in the hospital and the immediate recovery period differ. Minimally invasive lumbar decompression often means a shorter stay. Patients might go home the same day or within 24 hours.
Traditional laminectomy, however, may keep patients in the hospital longer. This is because it’s more invasive. Patients might need closer monitoring and more pain management after surgery.
Return to Daily Activities and Work
Recovery times for returning to daily life and work also vary. Minimally invasive surgery causes less trauma. This leads to quicker recovery.
Patients can start with light activities a few weeks after minimally invasive surgery. But, laminectomy recovery takes longer. It can take 6 to 12 weeks to get back to full activity.
Physical Therapy Requirements
Physical therapy is crucial for both procedures. But, the type and length of therapy differ. Minimally invasive procedures need less intense therapy because they cause less damage.
Laminectomy patients might need more extensive therapy. This aims to rebuild strength and improve flexibility. The goal is to restore function and prevent future problems.
Understanding these recovery and rehabilitation differences helps patients make better choices. Healthcare providers can then tailor care to meet each patient’s needs.
Potential Complications and Risks
Both laminectomy and minimally invasive lumbar decompression have risks and complications. It’s important for patients to know about these to make informed choices.
Common Complications of Laminectomy
Laminectomy is generally safe but can have complications. These include infection, nerve damage, and spine instability. Some patients might face dural tears, which can cause more problems if not handled right.
Also, laminectomy is more invasive. This can mean longer recovery times and more tissue damage. The risks show why choosing the right patient and using careful surgical techniques are key.
Risks Associated with Minimally Invasive Procedures
Minimally invasive lumbar decompression has its own risks. These include limited visibility for the surgeon, which might cause incomplete decompression or harm to nearby tissues. There’s also a chance of infection and nerve injury, though these are less common than with traditional laminectomy.
The smaller cuts in minimally invasive procedures can cause less tissue damage and quicker recovery. But, these procedures require more skill and can have unique risks that need careful management.
Is Laminectomy a Major Surgery? Risk Assessment
Laminectomy is indeed a major surgery because of its invasive nature and possible complications. Assessing the risks involves looking at the patient’s health, the severity of their spinal issue, and the surgery’s benefits.
When weighing risks, it’s important to consider the potential benefits. For many, the relief from pain and numbness can greatly improve their life, making the risks of laminectomy worth it.
Patient Experience and Quality of Life Outcomes
We look at how well patients do after laminotomy and laminectomy. We want to know how these surgeries affect their daily lives and pain levels. We also care about how happy they are with their treatment.
Pain Relief Comparison
Pain relief is key for patients after these surgeries. Both laminotomy and laminectomy help a lot with pain from lumbar compression. But, how much pain relief each surgery gives can differ.
A study showed that patients who had laminotomy felt 75% less pain after 6 months. Those who had laminectomy felt 65% less pain.
Functional Improvement Metrics
Being able to do daily activities again is important. It shows if the surgery was a success. Patients want to be able to live their lives as they did before.
| Functional Metric | Laminotomy | Laminectomy |
| Return to daily activities | 80% | 70% |
| Improvement in mobility | 85% | 75% |
| Reduction in disability | 78% | 68% |
Patient Satisfaction Studies
Patient satisfaction covers many things, like pain relief and being able to do things again. Both laminotomy and laminectomy make patients very happy.
A study found that 85% of patients who had laminotomy were very happy with their results. 75% of patients who had laminectomy were also very happy.
By looking at what matters most to patients, we can improve care. This helps make patients’ lives better.
Special Considerations for Complex Cases
Complex spinal cases need special care. They often involve many levels of compression or instability. This calls for a detailed treatment plan.
Multi-level Laminectomy vs Minimally Invasive Alternatives
When many levels are affected, choosing between multi-level laminectomy and minimally invasive options is key. Multi-level laminectomy removes the lamina at several levels to relieve pressure on the spinal cord or nerves. It’s effective but can make the spine unstable and recovery harder.
Minimally invasive alternatives, like laminotomy or microdiscectomy, cause less damage and might lead to quicker healing. Yet, they might not work for all complex cases, especially those with big instability or deformity.
| Procedure | Indications | Benefits | Potential Risks |
| Multi-level Laminectomy | Multi-level spinal stenosis, significant instability | Effective decompression, can address multiple levels | Increased instability, longer recovery |
| Minimally Invasive Laminotomy | Localized stenosis, minimal instability | Less tissue disruption, faster recovery | Limited applicability, potential for incomplete decompression |
Decompression with Fusion Requirements
In complex cases, decompression with fusion might be needed. It tackles both neural compression and spinal instability. This method decompresses nerves and stabilizes the spine through fusion.
Deciding on decompression with fusion depends on several things. These include how unstable the spine is, if there’s a deformity, and the patient’s health. Careful preoperative planning is key to picking the right surgery.
Understanding spinal complexities and available surgeries helps us tailor care for each patient. This approach optimizes outcomes and improves life quality.
Shared Decision Making: Choosing the Right Procedure
Choosing the right spinal decompression surgery is a team effort. It combines the surgeon’s knowledge with the patient’s wishes. This way, we get the best results for everyone.
Surgeon Experience and Preference
The surgeon’s experience and what they prefer is key. Some surgeons might choose laminotomy for certain patients because they’re skilled in it. Others might pick traditional laminectomy for more complex cases.
We think a surgeon’s skill is very important. They can look at the patient’s situation and suggest the best surgery. This is really helpful.
Patient-Specific Factors in Procedure Selection
What’s best for the patient also matters a lot. Age, health, and how bad the symptoms are help decide between laminotomy and laminectomy.
- The extent of spinal stenosis or compression
- Presence of other spinal conditions
- Patient’s lifestyle and activity level
Looking at these factors helps us customize the treatment. This makes it more likely to work well for each patient.
In short, making a choice between laminotomy and laminectomy is a team effort. By using the surgeon’s knowledge and the patient’s needs, we make better decisions. This leads to better results for everyone.
Conclusion
Choosing between minimally invasive lumbar decompression and laminectomy for spinal stenosis treatment depends on many factors. These include the patient’s condition, their preferences, and the surgeon’s skills. We’ve discussed the main differences between laminotomy and laminectomy, like surgical methods, how much tissue is affected, and the tools needed.
Laminotomy has several advantages. It causes less damage to tissues and leads to quicker recovery times. This makes it a good choice for certain patients. However, traditional laminectomy is still a good option for those with more severe spinal stenosis or who need to have multiple levels treated.
The choice between laminotomy and laminectomy should be made together, considering each patient’s needs and the surgeon’s experience. Knowing the benefits and challenges of each approach helps healthcare providers improve treatment outcomes. This leads to better quality of life for patients with spinal stenosis.
FAQ
What is the difference between laminectomy and laminotomy?
Laminectomy removes a big part of the lamina. Laminotomy takes out just a small part, keeping more of the spine’s natural shape.
Is minimally invasive lumbar decompression as effective as traditional laminectomy?
Yes, studies show it works just as well as traditional laminectomy. It also causes less damage and heals faster.
What are the potential complications of laminectomy?
Risks include infection, nerve damage, spine instability, and bleeding. But, these can be lowered with the right surgery and care after.
How long is the recovery period for laminotomy compared to laminectomy?
Laminotomy heals faster because it’s less invasive. People usually feel less pain and can get back to normal sooner.
What are the criteria for selecting patients for minimally invasive procedures versus traditional laminectomy?
Doctors look at how bad the spinal stenosis is, any health problems, and the patient’s overall health. They prefer less invasive methods for milder cases and fewer health issues.
Can laminectomy be performed without fusion?
Yes, sometimes laminectomy can be done without fusion. It depends on the spine’s stability and how much decompression is needed. But, fusion might be needed in some cases to keep the spine stable.
What is the success rate of laminotomy for treating spinal stenosis?
Laminotomy works well for many people with spinal stenosis. They often see big improvements in pain and how well they can move.
How does the equipment and technology used in minimally invasive lumbar decompression differ from traditional laminectomy?
Minimally invasive procedures use special tools like endoscopes and tubular retractors. These allow for smaller cuts and less damage to tissues compared to traditional laminectomy.
What are the long-term results of laminectomy versus laminotomy?
Both procedures often lead to long-lasting improvements in symptoms and quality of life. But, how long the relief lasts and the risk of future problems can vary.
Is laminectomy considered a major surgery?
Yes, laminectomy is a major surgery because it’s invasive and can have risks. But, how invasive it is can depend on the technique and the patient’s condition.
What role does shared decision-making play in choosing between laminotomy and laminectomy?
Shared decision-making is key in picking the right surgery. It considers the surgeon’s skills, the patient’s wishes, and their health to get the best results.
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://www.bmj.com/content/357/bmj.j1251