Craniotomy Survival Rate
Nearly 50,000 craniotomies are done every year in the United States. A craniotomy involves temporarily removing a portion of the skull to access the brain. This lets surgeons treat serious brain conditions Craniotomy Survival Rate.
The success of a craniotomy depends on many things. These include the medical condition being treated and the patient’s health. We will look into these factors closely. This will give us insights into the craniotomy survival rate and what affects it.
Key Takeaways
- Craniotomy is a surgical procedure to access the brain.
- The survival rate varies based on the underlying condition.
- Patient’s overall health is a significant factor.
- Craniotomy is used to treat life-threatening brain conditions.
- The procedure’s success rate is influenced by multiple factors.
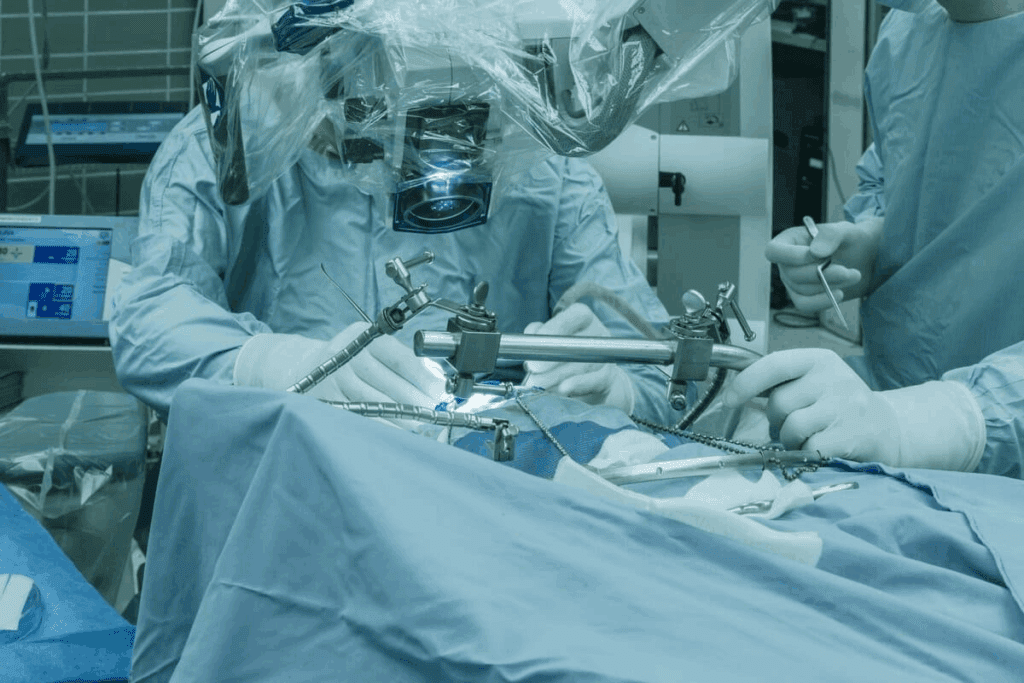
Understanding Craniotomy Procedures
A detailed surgical scene depicting an intricate craniotomy procedure. A skilled neurosurgeon, gowned in sterile attire, carefully manipulates specialized instruments as they delicately open the skull to expose the brain. Bright surgical lights illuminate the meticulously rendered surgical field, revealing the intricate anatomical structures with photorealistic clarity. The image conveys a sense of focused intensity, the surgeon’s intense concentration mirrored in the precise, controlled movements. The background is clean and clinical, emphasizing the gravity and importance of the procedure. This image aims to educate and inform, providing a visually compelling illustration of the craniotomy surgical process.
A craniotomy is a complex surgery. It involves removing part of the skull to reach the brain. This is done to treat brain issues like tumors, aneurysms, and hemorrhages.
Definition and Medical Purpose
A craniotomy is a surgery where a part of the skull is removed. This allows surgeons to work on the brain. It’s used when other treatments fail.
Choosing to do a craniotomy is a big decision. It needs careful planning and skill.
The Surgical Process Explained
The craniotomy surgery has several steps. First, the patient is given anesthesia for comfort.
- The scalp is cut, and the skin is moved to show the skull.
- A special tool makes holes in the skull, and a bone flap is taken out.
- The outer brain membrane is opened to get to the brain.
- The surgery is done, like removing a tumor or fixing a blood vessel.
- After the surgery, the membrane is closed, and the bone flap is put back.
- The scalp is closed with stitches or staples.
Knowing the steps of a craniotomy shows its complexity and the need for precision.
Step | Description |
1 | Preparation and anesthesia administration |
2 | Incision and exposure of the skull |
3 | Removal of the bone flap |
4 | Accessing the brain and performing surgery |
5 | Closing the dura mater and replacing the bone flap |
6 | Closing the scalp |
Types of Craniotomy Procedures
A detailed anatomical cross-section of a craniotomy procedure, revealing the surgical exposure of a meningioma brain tumor. The foreground depicts the carefully opened skull, exposing the delicate dural layers and the prominent meningioma mass, rendered in high definition. The middle ground showcases the precise surgical instrumentation used to carefully manipulate the tumor, with a moody, focused lighting casting dramatic shadows. The background provides a sense of depth, with a hazy, clinical environment suggesting a modern operating theater. Render this scene with a photorealistic, high-contrast aesthetic to convey the technical precision and gravity of the medical intervention.
Doctors use different craniotomy techniques for various medical needs. These procedures vary by the skull area and the surgery’s size and depth.
Location-Based Approaches
Craniotomies are divided by where they are done. Supratentorial craniotomies are above the tentorium cerebelli. They are used for tumors or aneurysms in the brain’s hemispheres.
Infratentorial craniotomies are below the tentorium. They access the posterior fossa, where the brainstem and cerebellum are.
Other location-based approaches include:
- Frontal craniotomy: Targets the frontal lobe, often for tumors or injuries.
- Temporal craniotomy: Focuses on the temporal lobe, used for epilepsy surgery or tumor removal.
- Parietal craniotomy: Aims at the parietal lobe, used for various conditions including tumors.
- Occipital craniotomy: Accesses the occipital lobe, typically for tumors or vascular lesions.
Size and Invasiveness Classifications
Craniotomies are also classified by size and invasiveness. A mini-craniotomy uses a small incision and bone flap. It causes less damage and leads to quicker recovery. This method is often used for precise surgeries like craniotomy meningioma removal.
A standard craniotomy uses a larger bone flap. It offers more access to the brain. This is needed for complex surgeries or large tumors or vascular issues.
Medical Conditions Requiring Craniotomy
A detailed and intricate medical illustration showcasing the craniotomy procedure for a meningioma brain tumor. In the foreground, a high-resolution anatomical cross-section depicts the exposed dura mater and underlying brain tissues, with the tumor mass clearly visible. The middle ground features surgical instruments and the craniotomy opening, captured in a clinical, well-lit setting. The background subtly conveys the sterile operating room environment, with clean walls and recessed lighting. The overall tone is informative and scientific, capturing the technical complexity of the procedure while maintaining a sense of photorealism.
Craniotomy is a key surgery for serious brain issues. It’s needed for life-threatening problems that other treatments can’t fix.
Brain Tumors and Craniotomy Meningioma Removal
Brain tumors, both benign and malignant, might need craniotomy for removal or biopsy. Meningiomas, which are usually benign, grow from the meninges. They are often treated with craniotomy. The goal is to remove the tumor completely, easing symptoms and stopping it from coming back.
“Removing meningiomas via craniotomy is very successful,” say neurosurgeons. Many patients see big improvements after surgery.
Non-Tumor Conditions
Craniotomy is also used for non-tumor conditions. These include:
- Aneurysms: These are abnormal blood vessel dilations in the brain. They can rupture and cause bleeding.
- Hemorrhages: Bleeding in or around the brain, often from trauma or vascular malformations.
For aneurysms or hemorrhages, craniotomy allows for quick action. Surgeons can clip aneurysms or remove hematomas. This reduces brain pressure and prevents more damage.
Thanks to new medical tech and surgery methods, patients are doing better. This brings hope for a better recovery and life quality.
Craniotomy Survival Rate: Comprehensive Statistics
A detailed and realistically rendered medical infographic showcasing comprehensive statistics on craniotomy survival rates. The infographic presents key data points and percentages in a clean, uncluttered layout against a neutral background, allowing the information to take center stage. The lighting is soft and evenly distributed, creating a professional, authoritative tone. The camera angle is slightly elevated, providing an overview of the entire composition. The color palette is muted and clinical, with the text and data visualizations standing out in a clear, legible manner. The overall aesthetic conveys a sense of medical expertise and factual reliability, suitable for inclusion in a scholarly article on this topic.
Looking into the survival rates of craniotomy procedures gives us important insights. The survival rate depends on many things. These include the patient’s health, the type of surgery, and the condition being treated.
Overall Survival Metrics
Research shows that survival rates for craniotomy vary. On average, about 70-80% of patients survive the first year after surgery. But, this number can change a lot based on the condition and the surgery’s complexity.
Key factors influencing overall survival metrics include:
- The patient’s age and overall health
- The nature and severity of the underlying condition
- The expertise of the surgical team
- The quality of post-operative care
Survival Rates by Procedure Type
Craniotomy procedures vary, and so do their survival rates. For example, patients getting a tumor removed might have different survival chances than those with a traumatic brain injury or aneurysm clipping.
Survival rates for specific procedure types:
Procedure Type | 1-Year Survival Rate | 5-Year Survival Rate |
Tumor Removal | 75% | 50% |
Aneurysm Clipping | 85% | 70% |
Traumatic Brain Injury | 60% | 40% |
These numbers highlight the need to know the survival rates for different craniotomy procedures. By looking at these statistics, we can understand the challenges of neurosurgery better. We also see what makes a surgery successful.
Factors Influencing Craniotomy Success Rate
Craniotomy success rate factors: a detailed medical illustration. A crisp, high-resolution photograph showcasing the key elements that influence the survival rate of a craniotomy procedure. In the foreground, a cross-section of the human skull reveals the intricate network of blood vessels, nerves, and brain matter. Subtle lighting accentuates the textures and shades of the anatomy, creating a sense of depth and realism. In the middle ground, a series of data visualizations and statistical charts display the crucial factors, such as patient age, underlying health conditions, and surgical techniques. The background features a clean, clinical environment with muted tones, allowing the core subject matter to take center stage.
It’s important to know what affects the success of a craniotomy. This is true for both patients and healthcare providers. The success of a craniotomy depends on many things.
Patient-Related Factors
Factors related to the patient are key in determining success. Age and overall health are very important. Older patients or those with serious health issues may face more risks.
The patient’s pre-operative condition also matters. This includes how severe their brain problem is and if they have other serious health issues.
Having comorbidities like diabetes or heart disease can make things harder. It’s important to manage these conditions well before, during, and after surgery.
Surgical and Hospital Factors
Surgical and hospital factors also play a big role. The experience and skill of the neurosurgeon are very important. A skilled surgeon can greatly improve the chances of success.
The quality of care at the hospital matters too. This includes the nursing staff and post-operative care facilities. Hospitals with specialized neurosurgery departments and the latest equipment tend to have better results.
The surgical technique and quality of post-operative care also matter a lot. New techniques and better care after surgery help improve success rates.
Condition-Specific Craniotomy Outcomes
A detailed, high-resolution medical illustration showcasing the outcomes of a craniotomy procedure for brain tumors. The image should depict the surgical site, with clear visualization of the skull opening, brain tissue, and any visible tumor remnants or scarring. The lighting should be bright and clinical, with a slight depth of field to draw the viewer’s attention to the key details. The overall composition should convey a sense of scientific accuracy and medical professionalism, suitable for inclusion in a scholarly article on craniotomy survival rates.
Craniotomy results depend a lot on the condition being treated. Some conditions do better than others. The success of the procedure greatly depends on the medical condition.
Brain Tumor Survival Statistics
For brain tumors, craniotomy outcomes vary a lot. Studies have shown that low-grade gliomas have better survival rates. This is compared to high-grade glioblastomas. We will look into these statistics to understand what affects outcomes.
Trauma and Hemorrhage Survival Rates
Craniotomy is used for traumatic brain injury or intracranial hemorrhage. The outcome in these cases depends on the injury’s severity, the patient’s age, and health. We will look at survival rates and what affects them.
It’s important to understand these outcomes to manage patient expectations. By analyzing data, we can see the complexity of neurosurgical procedures.
Craniotomy Mortality Rate: Understanding the Risks
A detailed and realistic medical illustration depicting a craniotomy surgical procedure, showcasing the mortality rate associated with this complex operation. The foreground features a precise cross-section of the human skull, with the brain and its intricate structures visible. The middle ground displays a team of skilled surgeons performing the delicate procedure, their expressions focused and their movements precise. The background presents a clinical, sterile environment, with medical equipment and monitors providing vital data. The lighting is crisp and directional, highlighting the gravity of the situation and the high-stakes nature of the procedure. The overall mood conveys a sense of urgency, professionalism, and the sobering realities of the craniotomy mortality rate.
It’s important to know the mortality rate of craniotomy to understand its risks. This surgery removes part of the skull to access the brain. It’s used for serious conditions.
Causes of Mortality Following Craniotomy
Several factors can lead to death after a craniotomy. These include the condition needing surgery, other health issues, and surgery problems. Knowing these risks helps improve care.
The main reasons for death are:
- Brain herniation from too much pressure
- Post-surgery bleeding
- Infections like meningitis or abscess
- Heart problems
Risk Stratification Models
Risk models are key for predicting outcomes after craniotomy. They help spot patients at higher risk. This allows for better care before and after surgery.
Risk Factor | Description | Impact on Mortality |
Age | Advanced age | Increased risk |
Comorbidities | Presence of other health conditions | Higher mortality |
Surgical Complexity | Extent and difficulty of the surgery | Increased risk with complexity |
Understanding these risks and using models helps doctors manage care better. This can lower the death rate from craniotomy.
Craniotomy Complications: Frequency and Management
It’s important to know about the risks of craniotomy to better care for patients. This surgery opens the skull to reach the brain. It’s a lifesaver for many, but it comes with dangers.
Common Complications
Craniotomy can lead to serious issues. Here are some common ones:
- Infection: Infections at the surgery site are a big worry. They can get very serious if not treated fast.
- Hemorrhage: Bleeding during or after surgery is a risk. It can cause more pressure in the brain and other problems.
- Neurological Deficits: Patients might face issues like weakness, numbness, or changes in thinking. This depends on where in the brain the surgery is done.
- Cerebral Edema: Brain swelling can happen. This can increase pressure inside the skull.
- Seizures: Some patients might have seizures after surgery. This is especially true for those who have had seizures before.
Managing and Preventing Complications
Dealing with and avoiding craniotomy problems needs a team effort. Preoperative planning is key. It includes checking the patient’s health and getting them ready for surgery. Surgical techniques and post-operative care are also vital in reducing risks.
To handle complications well, we use several methods:
- Antibiotic Prophylaxis: Giving antibiotics before surgery to lower infection risk.
- Close Monitoring: Keeping a close eye on the patient’s brain function and vital signs after surgery.
- Early Intervention: Quickly dealing with any problems that come up, like removing blood clots or managing seizures.
- Rehabilitation: Starting rehabilitation early to help patients recover from brain-related issues.
By knowing the risks of craniotomy and taking steps to prevent and manage them, we can make the surgery safer and more successful for patients.
Head Surgery Side Effects: Short and Long-Term
Head surgery can lead to many side effects, both right after and later on. It’s key for those having craniotomy and their families to know about these effects.
Immediate Post-Operative Effects
Right after a craniotomy, patients face several side effects. These come from the surgery and how the body reacts. Some common ones are:
- Pain and discomfort at the surgical site
- Swelling and bruising around the eyes and face
- Fatigue and general weakness
- Nausea and vomiting
- Headaches
Doctors use medicine and rest to help with these issues. It’s also important to watch patients closely to catch any problems early.
Long-Term Side Effects
Some people may deal with side effects for a long time after a craniotomy. These can depend on the surgery, the reason for it, and how extensive it was.
Long-term side effects might include:
- Cognitive changes, such as memory issues or trouble focusing
- Neurological deficits, like weakness, numbness, or seizures
- Emotional and psychological changes, such as mood swings or depression
- Changes in sensory perception, like vision or hearing changes
We will look into these long-term effects more, and how to handle them.
Side Effect | Potential Management Strategies |
Cognitive Changes | Cognitive rehabilitation, memory aids, and lifestyle adjustments |
Neurological Deficits | Physical therapy, medication to control seizures, and assistive devices |
Emotional/Psychological Changes | Counseling, support groups, and psychiatric medication if necessary |
Knowing about the side effects of craniotomy and how to manage them can really help a patient’s recovery. It can also improve their long-term health.
Craniotomy Recovery: Timeline and Expectations
Recovering from a craniotomy has two main parts: the hospital stay and care after leaving the hospital. Knowing about these phases helps patients and their families understand the recovery journey.
Hospital Phase
The hospital phase is key for watching for any problems right after surgery. Patients usually stay in a specialized care unit after surgery.
How long a patient stays in the hospital varies. It depends on their health, the surgery’s complexity, and how quickly they recover. Most stay 4 to 7 days. The medical team watches their brain health, manages pain, and fights off infections.
Post-Discharge Recovery
After leaving the hospital, patients start the post-discharge recovery phase. This can last weeks to months. It’s vital to follow the doctor’s instructions to recover well. This includes taking medicine, going to check-ups, and slowly getting back to physical activities.
Patients and their caregivers need to watch for signs of trouble. These include headaches, fever, confusion, or weakness
Recovering from a craniotomy is more than just healing from the surgery. It’s about getting strong again and doing daily tasks. Eating well and exercising helps support recovery.
Helping patients through recovery shows that a craniotomy needs a lot of care and support. Knowing the recovery timeline and what to expect helps patients prepare for their journey.
Modern Advances Improving Craniotomy Success Rates
Thanks to technological innovations and better perioperative care, craniotomy success rates have gone up. These changes have made a big difference in neurosurgery. Now, doctors can get better results for patients who have craniotomy procedures.
Technological Innovations
Modern technology has been key in boosting craniotomy success rates. Some important innovations include:
- Advanced Imaging Techniques: High-resolution imaging like MRI and CT scans help plan surgeries better. They let surgeons know exactly what they’re dealing with before they start.
- Intraoperative Navigation Systems: These systems help find the right spot during surgery. This makes surgeries safer and more accurate.
- Minimally Invasive Surgical Tools: New tools and methods mean less damage to tissues. Patients can recover faster because of this.
Perioperative Care Improvements
Improvements in perioperative care have also helped a lot. Key areas include:
- Enhanced Anesthesia Techniques: New anesthesia methods have made surgeries safer. Patients are more comfortable and have better results.
- Post-Operative Care Management: Better care after surgery, like ICU stays and rehab, helps patients heal faster. It also lowers the chance of problems.
- Multidisciplinary Care Teams: Working together, doctors, nurses, and specialists make sure patients get the best care. This team approach helps a lot.
By using technological innovations and improved perioperative care, we’ve made craniotomy success rates much better. Patients now have better outcomes and a better quality of life.
Preparing for a Craniotomy Operation
Getting ready for a craniotomy is crucial. It involves checking your health, improving your well-being, and getting emotional support.
Medical Preparation
Medical prep is a big part of getting ready for surgery. It includes tests and checks to see how you’re doing and why you need surgery.
Tests like MRI or CT scans are used to see the brain area that needs surgery.
IPractical and Emotional Preparation
Getting ready isn’t just about the medical stuff. It’s also about being ready for what comes after surgery. Patients and their families need to know what to expect during recovery.
Practical steps include making plans for care after you leave the hospital. You might need to set up your home for recovery or plan for follow-up visits.
“Emotional support is just as important as medical prep,” says a patient support group member. “Helping patients find support groups or counseling can help them feel less scared and more positive.”
By focusing on both medical and emotional preparation, patients can handle the challenges of a craniotomy better.
Post-Operative Care Following Craniotomy
Effective post-operative care is key for patients after a craniotomy. It affects their recovery and long-term health. The post-operative period is crucial for managing complications and ensuring patients get the support they need.
Immediate Care Needs
Patients need close monitoring in a specialized care unit right after a craniotomy. Monitoring for complications is vital. It helps healthcare providers address any issues quickly.
Another important part is pain management. Patients may feel pain or discomfort after surgery. We use medications and other strategies to manage pain effectively.
Long-Term Follow-Up
After the hospital, patients recover at home, needing ongoing support. Rehabilitation is key in the recovery process. It helps patients regain strength, mobility, and cognitive function.
Regular follow-up care is also crucial. We schedule appointments to check on the patient’s recovery. We manage ongoing issues and provide support as needed.
By focusing on both immediate care and long-term follow-up, we ensure patients get the best post-operative care. This optimizes their recovery and outcomes.
Real-Life Craniotomy Experiences and Outcomes
Patients who have had a craniotomy share a wide range of experiences. Some have made amazing recoveries, while others face tough challenges. These stories show the surgery’s complexity and the strength of those who go through it.
Success Stories
Many patients have overcome the hurdles of craniotomy and seen big improvements in their health. For example, a patient might say,
“After my craniotomy, I was able to return to my normal life within a few months. The support of my medical team was invaluable.”
Thesesuccess stories show that with the right care and support, positive outcomes are possible.
Challenges and Coping Strategies
Not all patients have an easy time after a craniotomy. They might deal with physical, cognitive, or emotional issues. Effective coping strategies are key to managing these challenges. Patients often find help from medical teams, family, and their own inner strength.
Some coping strategies include:
- Seeking support from family and friends
- Engaging in rehabilitation programs
- Practicing stress-reduction techniques such as meditation or yoga
As one patient shared,
“The road to recovery was tough, but with the right mindset and support, I was able to overcome the challenges and regain my independence.”
These experiences underline the need for a strong support network during recovery.
Selecting the Right Medical Team for Craniotomy
Choosing a skilled medical team is key for craniotomy surgery patients. The knowledge of your neurosurgeons and the medical care you get can greatly affect your recovery.
Finding Specialized Neurosurgeons
For craniotomy, your neurosurgeon’s experience matters a lot. Look for those with a strong track record in craniotomies and who use the latest methods.
Make sure to check the qualifications and experience of potential neurosurgeons. Look at their credentials, understand their approach to your condition, and read patient feedback.
Essential Questions for Your Surgical Team
It’s important to ask the right questions to feel confident in your care. Here are some key questions to ask:
- What experience do you have with craniotomy procedures?
- Can you explain the surgical plan and the techniques you’ll be using?
- What are the potential risks and complications associated with my specific case?
- How will my pain be managed during and after the surgery?
- What is the expected recovery time, and what kind of post-operative care will I receive?
By asking these questions and choosing a surgical team that makes you feel confident and cared for, you can improve your chances of a good outcome.
Conclusion: The Future of Craniotomy Prognosis
Craniotomy is a complex surgery that needs careful thought and precision. Thanks to new medical technology and care, survival rates have greatly improved.
We’ve talked about what affects craniotomy outcomes. This includes the patient’s health, the surgery method, and aftercare. Knowing these helps patients and doctors improve results together.
Looking ahead, we expect neurosurgery to keep getting better. This will lead to even higher survival rates and better care for patients. As research and technology grow, treatments will get more effective, helping more people recover from craniotomy.
FAQ
What is a craniotomy?
A craniotomy is a surgery where part of the skull is removed. This lets surgeons work on the brain. They treat brain conditions this way.
What is the survival rate for a craniotomy?
The survival rate for a craniotomy depends on many things. These include the condition being treated and the patient’s health. The complexity of the surgery also plays a role. Generally, many people survive, but it varies.
What conditions are treated with craniotomy?
Craniotomy treats many conditions. These include brain tumors, aneurysms, hemorrhages, and injuries to the brain.
What are the different types of craniotomy procedures?
There are different types of craniotomy. They are based on where the surgery is done and how big it is. For example, there are frontal, temporal, and parietal craniotomies. There are also mini-craniotomies and decompressive craniectomies.
What are the common complications of craniotomy?
Complications can include infections, bleeding, swelling in the brain, seizures, and problems with brain function. The risk of these issues depends on the surgery and the patient.
How long does it take to recover from a craniotomy?
Recovery time varies. It depends on the person, the surgery, and the condition being treated. Patients usually stay in the hospital for a few days to a week. They may need weeks or months to fully recover.
What is the mortality rate associated with craniotomy?
The death rate for craniotomy depends on several factors. These include the patient’s health, the condition being treated, and the surgery’s complexity. While death is rare, it’s not unheard of. Patients should talk to their surgeon about their risks.
How can I prepare for a craniotomy operation?
Preparing involves a medical check-up and improving your health. You should also prepare emotionally and practically. Follow your surgeon’s advice and ask questions to be ready.
What kind of post-operative care is required after craniotomy?
After surgery, you’ll need to watch for complications and manage pain. You’ll also have follow-up appointments. You might need rehabilitation to regain lost functions or manage side effects.
How do I choose the right medical team for my craniotomy?
Choose a team with experienced neurosurgeons. Ask them about their expertise, the procedure, and aftercare. This ensures you’re in good hands.
What are the long-term side effects of craniotomy?
Long-term effects can include brain function problems, seizures, and changes in thinking or mood. The risk and severity depend on the individual and the surgery.
Can craniotomy be performed on elderly patients?
Yes, craniotomy can be done on older patients. The decision depends on their health, the condition, and the surgery’s benefits and risks.
What is the role of rehabilitation after craniotomy?
Rehabilitation is key. It helps patients regain lost functions, manage side effects, and improve their life quality after surgery.
Are there any new technologies or techniques improving craniotomy outcomes?
Yes, new imaging, surgical tools, and care methods are making craniotomy safer and more effective. These advancements are improving outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/23472847/