Did you know that nearly 20,000 people in the United States undergo brain surgery every year? This surgery, known as a craniotomy, involves removing part of the skull to reach the brain. It’s key for diagnosing and treating brain issues.
We are dedicated to top-notch medical care, including for international patients. Our team offers personalized care and support during the surgical procedure.
Key Takeaways
- Exploratory brain surgery is often referred to as a craniotomy.
- A craniotomy involves temporarily removing part of the skull to access the brain.
- This surgical procedure is necessary for diagnosing and treating various brain conditions.
- Our medical team provides personalized care and guidance throughout the process.
- We are committed to delivering world-class healthcare for international patients.
Craniotomy: The Primary Form of Exploratory Brain Surgery
Craniotomy is a key neurosurgical procedure. It lets doctors access the brain by taking out a part of the skull. This surgery is vital for both diagnosis and treatment.
Definition and Medical Purpose
A craniotomy means removing a part of the skull, called a bone flap, to see the brain. Neurosurgeons use this to treat serious issues like brain tumors, aneurysms, and injuries.
The main goal of a craniotomy is to get to the brain directly. This helps doctors diagnose and treat severe conditions. The bone flap is kept safe and put back after the surgery is done.
Historical Development of Craniotomy Techniques
Craniotomy methods have changed a lot over time. The first versions were used by ancient people, known as trephining.
Today’s craniotomy methods have improved thanks to new medical tech. This includes MRI and CT scans, and better surgical tools.
- Microsurgical Techniques: New microsurgical methods make procedures more precise and less invasive.
- Image-Guided Surgery: Image-guided systems help surgeons navigate the brain more accurately.
- Minimally Invasive Approaches: There’s a push for less invasive craniotomies. This helps patients recover faster and do better.
The Exploratory Nature of Craniotomy Procedures
Craniotomy is a key surgery in neurosurgery. It involves removing a bone flap from the skull to reach the brain. This method is essential for diagnosing and treating brain issues.
Craniotomy can be used for both diagnosis and treatment. Diagnostic craniotomy is done when other tests don’t give clear answers. Surgeons then look at the brain tissue to find out what’s wrong.
Diagnostic vs. Therapeutic Objectives
The main goal of a craniotomy can change based on the patient’s situation. Sometimes, it’s just to find out what’s causing symptoms. For example, if scans can’t show what’s wrong.
But, a therapeutic craniotomy aims to fix a known problem. This might mean removing a tumor, fixing an aneurysm, or easing brain pressure.
“The decision to perform a craniotomy is always made with careful consideration of the possible benefits and risks.” – Neurosurgical Expert
When Exploratory Craniotomy is Necessary
Exploratory craniotomy is needed in a few situations:
- When tests don’t give clear results.
- In severe brain injuries or trauma.
- When it’s necessary to see and check the brain tissue directly.
It’s important to understand the balance between finding out what’s wrong and fixing it. This helps surgeons and patients make good choices about surgery. It’s about the chance for brain surgery recovery and the best outcome.
Craniotomy vs. Craniectomy: Understanding the Differences
In neurosurgery, knowing the difference between craniotomy and craniectomy is key. These two procedures are related but differ in their methods and uses.
A craniotomy removes a part of the skull temporarily. This lets neurosurgeons do things like remove tumors or fix aneurysms. Then, they put the bone flap back.
A craniectomy removes a part of the skull but doesn’t put it back right away. This is often to reduce brain pressure from swelling or injury.
Temporary vs. Permanent Skull Opening
The main difference is how the bone flap is handled. In a craniotomy, the bone flap goes back after surgery. But in a craniectomy, it stays out, sometimes forever.
We do craniotomies when we need temporary brain access and can close the skull later. Craniectomies are for emergencies where we need to reduce brain pressure.
Clinical Indications for Each Procedure
Choosing between craniotomy and craniectomy depends on the patient’s situation and the doctor’s opinion. Craniotomies are used for:
- Tumor removal
- Aneurysm clipping
- Arteriovenous malformation (AVM) treatment
Craniectomies are for urgent cases, like:
- Traumatic brain injury with swelling
- Stroke with severe swelling
- Intracranial hemorrhage with pressure
It’s important for patients and families to understand these differences. This helps them make better choices about their care. We help our patients choose the best surgery for their needs.
Types of Craniotomy Procedures
Craniotomy procedures vary based on the brain region needing access. This allows neurosurgeons to tailor their approach for each patient’s condition. It ensures the best possible outcomes for patients.
Bifrontal Craniotomy
A bifrontal craniotomy accesses both frontal lobes of the brain. It’s used for conditions affecting both sides of the frontal region, like tumors or vascular issues. This way, surgeons can treat complex conditions that need both sides of the brain.
Frontal Craniotomy
A frontal craniotomy targets one frontal lobe. It’s common for treating tumors, aneurysms, or other issues in the frontal brain area. This method allows for precise treatment with little disruption to the surrounding brain.
Regional Approaches and Specialized Techniques
There are many regional approaches used depending on the brain area needing surgery. These include temporal, occipital, and suboccipital craniotomies, among others. Each method is chosen based on the patient’s condition, the location and nature of the problem, and their overall health.
We use these specialized techniques to give our patients the best care for their needs. Advanced imaging and precise surgery help us achieve great results in treating complex brain conditions.
Medical Conditions Requiring a Craniotomy
Several medical conditions need a craniotomy, a surgery that opens the skull. This lets neurosurgeons treat serious conditions directly.
Brain Tumors and Mass Removal
Brain tumors can greatly affect a person’s life and chances of survival. Craniotomy is often used to remove these tumors. The goal is to take out as much tumor as possible while keeping the brain safe.
The National Brain Tumor Society says the type and location of the tumor matter for surgery. Tumors near important brain areas might need special care to avoid damage.
Tumor Type | Location | Surgical Considerations |
Glioblastoma | Cerebral hemispheres | Aggressive resection, possible adjuvant therapy |
Meningioma | Near meninges | Often fully removed, small ones might be watched |
Traumatic Brain Injuries and Hematomas
Traumatic brain injuries (TBI) can cause hematomas, dangerous blood collections outside brain vessels. Craniotomy is used to remove the hematoma and ease brain pressure.
“Prompt surgery is key for severe TBI to prevent more brain damage.”
American Association of Neurological Surgeons
Deciding on a craniotomy for TBI depends on injury severity, hematoma size and location, and the patient’s health.
Vascular Abnormalities and Aneurysms
Vascular issues, like aneurysms, are risky because they can burst and bleed. Craniotomy is a treatment option, mainly for those in critical areas.
Choosing between clipping and coiling for aneurysms depends on location, size, and patient health.
- Clipping involves placing a clip around the aneurysm’s neck.
- Coiling is less invasive, using coils to fill the aneurysm.
Craniotomy gives neurosurgeons direct access to the aneurysm for clipping.
The Bone Flap: Critical Component of Craniotomy Surgery
In craniotomy, the bone flap is key. It’s a part of the skull removed to reach the brain.
Creation and Preservation Techniques
Making the bone flap requires precise surgery. We use special tools to cut and remove it carefully. This way, we avoid harming the surrounding tissue.
Keeping the bone flap clean is also vital. We store it in a sterile solution or freeze it for later use. This prevents infection.
Reattachment Methods and Materials
Putting the bone flap back is a major part of the surgery. We use different materials and methods to fix it in place. This helps the healing process and reduces risks.
The choice of material depends on the bone flap’s size and the patient’s health. We often use titanium plates, sutures, and bioabsorbable materials.
Reattachment Method | Material Used | Advantages |
Titanium Plates | Titanium | Strong, durable, and biocompatible |
Sutures | Non-absorbable sutures | Flexible, easy to use |
Bioabsorbable Materials | Polylactic acid | Absorbs over time, reducing long-term complications |
By carefully making, keeping, and putting back the bone flap, we aim for the best results for patients.
Step-by-Step Craniotomy Procedure
Surgeons follow a detailed plan for a craniotomy to keep patients safe and get the best results. This complex surgery has many important steps, from getting ready before surgery to closing up afterwards.
Preoperative Preparation and Anesthesia
The first step is preoperative preparation. We give the patient anesthesia to keep them comfortable and safe. We watch their vital signs and get the surgery area ready.
- Administering general anesthesia to the patient
- Preparing the surgical site by cleaning and disinfecting
- Positioning the patient correctly on the operating table
Surgical Incision and Skull Access
After getting the patient ready, we make a surgical incision. We plan the incision carefully to reach the brain area we need. Then, we do a craniotomy to open the skull.
- Making a surgical incision in the scalp
- Retracting the scalp and muscle to expose the skull
- Drilling burr holes and using a craniotome to create a bone flap
Brain Exploration and Intervention
With the skull open, we start brain exploration. We find the area we need to work on and do the intervention. This could be removing a tumor, clipping an aneurysm, or fixing damaged tissue.
- Identifying the target area within the brain
- Performing the necessary surgical intervention
- Monitoring the patient’s brain activity throughout the procedure
Our team works together with great care and precision. We focus on the patient’s safety and well-being at every step of the craniotomy procedure.
Advanced Imaging Technologies in Craniotomy Planning
In neurosurgery, advanced imaging is key for planning and doing craniotomies. These tools have made surgeries more precise and safe.
Intraoperative Imaging and Navigation
Intraoperative imaging and navigation systems are key for craniotomy success. They give real-time updates during surgery, keeping the team on track with the patient’s anatomy.
Intraoperative MRI and CT scans help check tumor removal or update navigation data during surgery. This is very helpful when tumors are close to important brain areas.
Advanced imaging in craniotomy planning has changed neurosurgery. It makes surgeries more precise and less invasive. This has led to better patient outcomes and faster recoveries.
Awake Craniotomy: A Specialized Exploratory Approach
Awake craniotomy is a new way in neurosurgery. It lets surgeons map and watch the brain in real time. This method has changed how we treat some brain problems, making surgery more precise.
Patient Selection and Preparation
Choosing the right patient is key for awake craniotomy. People with brain tumors or epilepsy near important brain areas are often chosen. We check each patient’s health and brain condition to see if they’re a good fit.
Getting ready for the surgery is also important. Patients learn about the risks and benefits. They also find out how brain mapping works and why their help is needed during the surgery.
Procedure Differences and Brain Mapping
Unlike usual craniotomies, awake craniotomy lets surgeons talk to patients during surgery. This is important for brain mapping. It helps us keep important brain functions like speech and movement safe.
We use special tools to watch brain activity and map brain areas in real time. This helps us make better choices during surgery. We can remove bad tissue without harming the brain.
Benefits and Challenges for Patient and Surgeon
The benefits of awake craniotomy include more accurate tumor removal and less chance of brain damage. Patients can also recover faster. Being awake can be scary, but it lets them tell us how they feel right away.
For surgeons, it’s hard to keep patients calm and comfortable while working. We team up with anesthesiologists to make sure patients are safe and comfortable.
In short, awake craniotomy is a complex surgery with big benefits. By picking the right patients and using advanced brain mapping, we can do better surgeries. This improves our patients’ lives.
Minimally Invasive Alternatives to Traditional Craniotomy
The world of neurosurgery is changing fast. Now, we see more use of new, less invasive methods. These new ways aim to cause less damage, help patients heal faster, and lead to better results.
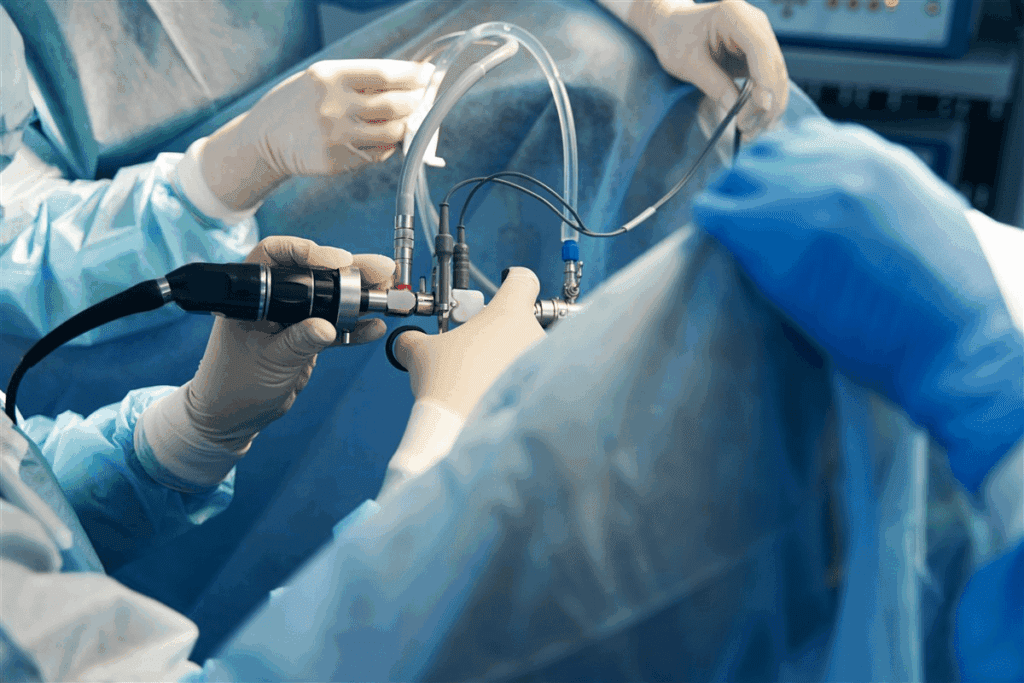
Endoscopic and Keyhole Approaches
Endoscopic and keyhole surgery are big steps forward in neurosurgery. They use smaller cuts and cause less harm. This means patients can get back to their lives sooner and face fewer risks.
Endoscopic surgery uses a tiny camera and tools through small holes. It lets doctors work on the brain’s tricky parts with great care. Keyhole surgery also uses a small opening in the skull. It gives access to certain brain spots without needing to remove much tissue.
Stereotactic Radiosurgery Options
Stereotactic radiosurgery (SRS) is another minimally invasive choice instead of traditional craniotomy. It’s a precise radiation therapy that focuses on specific brain spots. This helps avoid harming healthy tissue. It’s great for treating some brain tumors and other hard-to-reach conditions.
Treatment Option | Description | Benefits |
Endoscopic Approaches | Utilizes a small camera and specialized instruments through tiny incisions | Less tissue disruption, quicker recovery |
Keyhole Surgery | Involves a small craniotomy for access to specific brain areas | Minimizes tissue removal, reduces risk |
Stereotactic Radiosurgery | Highly precise radiation therapy targeting specific brain areas | Non-invasive, spares healthy tissue |
These minimally invasive alternatives are changing neurosurgery for the better. They offer safer, more effective treatments. Patients get to heal faster and face fewer problems. As technology gets better, we’ll see even more improvements in these methods.
Immediate Post-Craniotomy Care
After a craniotomy, care focuses on managing pain, intracranial pressure, and other vital signs. This approach is key to improving patient outcomes and lowering the risk of complications.
Intensive Care Monitoring Protocols
Patients are moved to the ICU for close monitoring after a craniotomy. We use advanced tools to watch vital signs, neurological status, and intracranial pressure. This helps us spot and act on any changes quickly.
The ICU team keeps an eye on several important things, including:
- Level of consciousness and neurological function
- Intracranial pressure
- Blood pressure and cardiovascular stability
- Oxygen saturation and respiratory function
Managing Pain and Intracranial Pressure
Managing pain is vital for patient comfort and can affect intracranial pressure. We use both medicines and non-medical methods to control pain, such as:
- Opioid analgesics and other pain medications
- Positioning and comfort measures
- Relaxation techniques
Keeping intracranial pressure in check is also a top priority. High ICP can cause serious problems. So, we use various methods to keep ICP at a safe level, including:
- Elevation of the head of the bed
- Administration of osmotic diuretics
- CSF drainage if necessary
Care Aspect | Monitoring/Intervention | Goal |
Neurological Status | Frequent neurological assessments | Early detection of neurological deterioration |
Pain Management | Pharmacological and non-pharmacological interventions | Optimal pain control |
Intracranial Pressure | ICP monitoring, CSF drainage, osmotic diuretics | Maintenance of normal ICP |
By following these intensive care protocols and managing pain and intracranial pressure well, we can greatly improve patient outcomes after a craniotomy.
Craniotomy Recovery Timeline and Expectations
Recovering from a craniotomy takes several stages. These include immediate care after surgery and long-term rehabilitation. Knowing these stages helps manage expectations and ensures a smooth recovery.
Hospital Stay Duration and Care
The time spent in the hospital after a craniotomy varies. It can be a few days to over a week. During this time, patients are watched closely in the ICU for any immediate issues.
Intensive care monitoring is key to managing pain, intracranial pressure, and neurological deficits. The medical team keeps a close eye on the patient’s condition. They adjust care plans as needed.
Day | Typical Care Activities |
1-2 | ICU monitoring, pain management, initial neurological assessment |
3-5 | Continued monitoring, possible move to a regular ward, start of rehabilitation |
6+ | Rehabilitation therapy, planning for discharge, scheduling follow-up appointments |
Short-term Recovery Milestones
In the short term, patients can reach several recovery milestones. These include regaining basic motor functions, improving cognitive abilities, and managing post-operative pain.
- Regaining independence in daily activities
- Improving mobility with physical therapy
- Enhancing cognitive function through occupational therapy
As one neurosurgeon noted, “The key to successful recovery is a multidisciplinary approach. This involves neurosurgeons, rehabilitation specialists, and family support.”
“Recovery is a journey, not a destination. With the right care and support, patients can achieve significant improvements in their quality of life.”
Long-term Rehabilitation and Follow-up
Long-term rehabilitation is vital for restoring functional abilities and improving quality of life. This phase includes ongoing physical, occupational, and speech therapy.
Follow-up care is emphasized. Regular appointments are needed to monitor progress, address complications, and adjust rehabilitation plans as necessary.
Understanding the craniotomy recovery timeline and expectations helps patients and their families navigate the recovery process. This ensures the best possible outcomes.
Potential Complications and Side Effects of Craniotomy
Choosing to have a craniotomy means weighing the good against the bad. Like any big surgery, there are risks and effects on the brain. Patients and doctors must think about these possibilities.
Immediate Surgical Risks and Complications
Right after surgery, there are dangers like infection, bleeding, and bad reactions to anesthesia. These dangers are lessened by careful prep and watching closely during surgery.
- Infection: Even with clean methods, infections can happen.
- Bleeding: Bleeding can happen during or after surgery, causing big problems.
- Anesthesia complications: Reactions to anesthesia can be mild or serious.
A study in the Journal of Neurosurgery found that complications in craniotomy patients are common. This shows the importance of choosing the right patient and using careful surgery.
“The risk of complications following craniotomy is not trivial, and understanding these risks is essential for informed decision-making.”
Journal of Neurosurgery
Short-term Neurological Effects
Right after surgery, you might feel confused, have trouble remembering things, or have weakness or numbness. These problems usually depend on where in the brain the surgery was.
Neurological Effect | Description | Typical Recovery Time |
Confusion | Feeling disoriented and mentally off | Days to weeks |
Memory issues | Struggling to remember recent events or learn new stuff | Weeks to months |
Focal deficits | Weakness, numbness, or other problems in the area of surgery | Variable, might last forever |
Long-term Side Effects and Management
Long-term problems can include seizures, changes in thinking, and mood or behavior changes. How to deal with these depends on the problem and might include medicine, therapy, or other treatments.
Seizure management is key after craniotomy. Doctors often give medicines to stop seizures, mainly for those who have had seizures before.
Cognitive rehabilitation helps patients get back their thinking skills and adjust to any lasting changes. These programs are made just for the person and might include speech, occupational therapy, and more.
It’s important for patients and doctors to know about the risks and side effects of craniotomy. By understanding these and taking steps to lessen them, we can help patients recover better.
Patient Decision-Making and Preparation for Craniotomy
Patients facing a craniotomy need to know a lot to make good choices. This surgery is complex and requires understanding risks, benefits, and recovery.
Understanding Surgical Consent
Surgical consent is key to ensure patients know what they’re getting into. It’s not just a formality; it’s a vital step in patient care. The neurosurgeon will explain the surgery, risks, and alternatives. Patients should ask questions and share any worries.
The consent process is an opportunity for patients to understand their role in the recovery process. It’s important for patients to know they play a big part in their recovery.
Questions to Ask Your Neurosurgeon
Preparing a list of questions for the neurosurgeon can help patients feel more in control and informed. Some key questions to consider include:
- What are the primary reasons for recommending a craniotomy in my case?
- What are the possible risks and complications of this procedure?
- Are there other treatments I could try, and how do they compare to craniotomy?
- What’s the expected recovery time, and what kind of care will I need after surgery?
- Are there any specific risks or considerations based on my medical history?
Psychological Preparation and Support
Going through a craniotomy can be stressful for patients and their families. Psychological preparation is key for coping with the procedure and recovery. Patients should talk about their fears and worries with their healthcare provider.
Support systems, like family, friends, or support groups, are very important. Having a strong support network can greatly help a patient cope with surgery and rehabilitation.
In conclusion, patient decision-making and preparation are key to the craniotomy process. By understanding consent, asking the right questions, and preparing mentally, patients can face this complex procedure with more confidence and clarity.
Conclusion: Advances in Exploratory Brain Surgery
As we wrap up our look at craniotomy and exploratory brain surgery, it’s clear that medical tech and surgery methods are getting better. Neurosurgery has made big strides, changing how we find and treat brain problems.
Thanks to advanced imaging like MRI and CT, surgeons can now plan and do craniotomy surgeries more accurately. These brain surgery improvements have made exploratory brain surgery safer and more effective. They also open up new ways to treat conditions that were once too hard to fix.
Looking ahead, neurosurgery’s future looks bright. New technologies and methods will keep improving care and results for patients. The future of neurosurgery is full of promise, with new tools and techniques ready to change exploratory brain surgery again.
FAQ
What is a craniotomy?
A craniotomy is a surgery where part of the skull is taken off to reach the brain. It’s often needed to diagnose and treat brain issues.
What is the difference between a craniotomy and a craniectomy?
A craniotomy removes part of the skull to access the brain and then puts it back. A craniectomy removes part of the skull but doesn’t put it back right away.
What are the purposes of a craniotomy?
Craniotomy can help diagnose, relieve pressure, or remove tumors or damaged brain tissue. It can be for checking or treating.
What is an awake craniotomy?
An awake craniotomy is done while the patient is awake. It lets the surgeon map and monitor the brain in real-time. It has its benefits and challenges.
What are the risks and possible complications of a craniotomy?
Like any surgery, craniotomy has risks and complications. These can include immediate surgical risks, short-term brain effects, and long-term side effects.
How long does it take to recover from a craniotomy?
Recovery time after a craniotomy varies. It includes the hospital stay, short-term goals, and long-term care and follow-up.
What are the alternatives to traditional craniotomy?
Options include minimally invasive surgeries like endoscopic and keyhole surgery, and stereotactic radiosurgery. Each has its own uses and benefits.
What is the role of advanced imaging technologies in craniotomy planning?
Technologies like MRI and CT scans give detailed images. They help the surgical team during the procedure, improving results.
How is the bone flap handled during craniotomy?
The bone flap is handled carefully. Techniques are used to create, preserve, and reattach it. Materials are used for reconstruction.
What are the benefits of craniotomy for patients with brain tumors or vascular abnormalities?
Craniotomy is often needed for brain tumors, injuries, and vascular issues like aneurysms. It aims to improve patient outcomes.
What should patients consider when preparing for a craniotomy?
Patients should understand the procedure, risks, and benefits. Asking questions to the neurosurgeon is key. Psychological preparation and support are also important.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560922/










